By Robert van der Vaart, MD, and Kenneth L. Cohen, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Pars plana vitrectomy (PPV) is now a frequently performed vitreoretinal surgery that, with improvements over the last decade, generally provides excellent anatomic, visual, and safety outcomes. The indications for PPV are numerous and include rhegmatogenous or tractional retinal detachment, proliferative diabetic retinopathy, macular hole, epiretinal membrane, trauma, vitreous hemorrhage, and endophthalmitis.
Although patients are commonly referred to a vitreoretinal specialist for PPV, the comprehensive ophthalmologist is likely to participate in the long-term care of postvitrectomy patients. For example, the ophthalmologist will probably be faced with making decisions about cataract surgery, as cataract develops and progresses in up to 70% of patients within 2 years after PPV.1 The cataract surgeon needs to understand the unique challenges of cataract surgery in post-PPV eyes.
Why Is Phaco After PPV Challenging?
Eyes that have undergone PPV have a higher risk of intraoperative and postoperative complications; this is a result of both the original disease that led to the PPV and the consequences of the vitrectomy procedure. The cataracts that occur most commonly after PPV are the denser nuclear sclerotic and posterior subcapsular types, rather than senile cataracts.2,3
The lack of posterior support for the cataractous lens makes performing the capsulorrhexis more difficult. Because of decreased resistance, the surgeon needs to exert more pressure with the cystotome or the point of the capsulorrhexis forceps. However, occult zonular instability and/or posterior capsule damage may be present after PPV, and greater pressure against the capsule may exacerbate the situation.
Removal of the nucleus, epinucleus, and cortex is complicated by the lack of vitreous support, compromise of the supporting structures of the lens, and large fluctuations in anterior chamber depth. These factors also make it more difficult to place the IOL in the capsular bag. The incidence of perioperative complications, including iris trauma, choroidal hemorrhage, and nuclear fragment loss, may be as high as 12.5%.2
Preoperative Considerations
PPV changes the structure of the eye, and the cataract surgeon’s preoperative evaluation should take into account the effect of these changes.
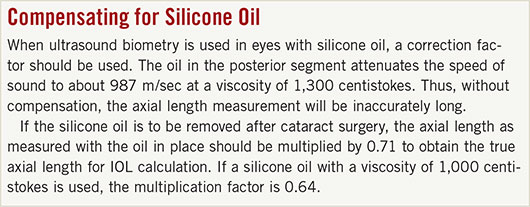
Biometry. Optical biometry is more accurate than ultrasound biometry in vitrectomized eyes for several reasons. First, myopia is a risk factor for many of the vitreoretinal conditions that are treated with PPV; therefore, these eyes are often highly myopic or have posterior staphylomas. Second, if silicone oil is present, axial length measurement will be incorrect unless a compensating factor is used (see “Compensating for Silicone Oil”).
If the cataract is too dense for optical biometry, then immersion ultrasound is preferred.
Assessing the need for cataract surgery. It can be difficult to confirm that the cataract—rather than coexisting vitreoretinal disease or prior treatment—is the primary cause of visual deficit in post-PPV eyes. Careful review of the medical record, including tracking visual acuity changes before and after vitrectomy, as well as use of instrumentation such as the potential acuity meter, can assist in making this decision.
Preparing for possible complications. It is vital for the cataract surgeon to carefully evaluate for the presence of sequelae from the PPV procedure; these may include zonular instability, phacodonesis, and posterior capsule compromise. Such findings require the surgeon to adapt his or her operative techniques.
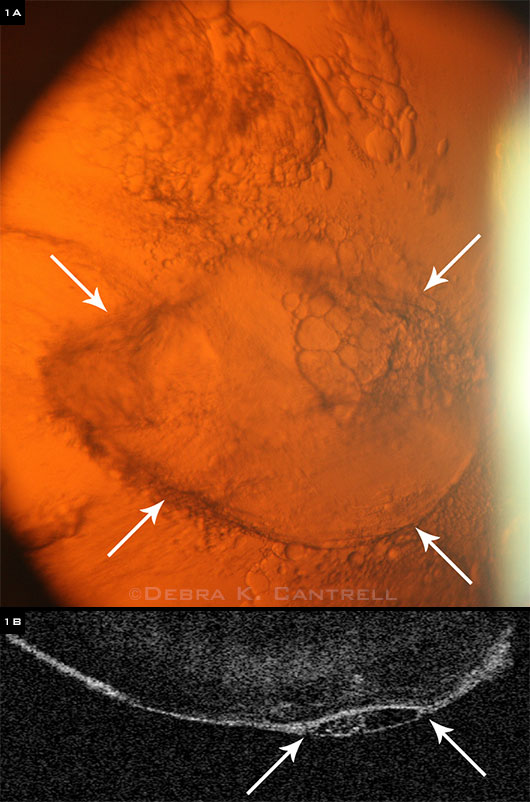
For example, during a preoperative evaluation on one of our patients, we identified the posterior capsular hole shown in Figure 1. Accordingly, we altered our surgical approach to eliminate hydrodissection, use less vigorous nuclear manipulation, and employ dispersive OVD more liberally. These adaptations produced an excellent outcome for the patient.
Informed consent. The consent process for the postvitrectomy eye should be customized to take into account the higher degree of risk associated with cataract surgery in this setting. It is essential for the patient to understand the increased risk for adverse events.
 |
|
PREOPERATIVE DISCOVERY. (1A) The arrows indicate a posterior capsule hole identified in preoperative evaluation for cataract surgery in a patient who had previously undergone PPV. (1B) In this anterior segment OCT taken in the same patient, the arrows indicate the area of posterior capsule injury with incomplete healing.
|
Perioperative Steps
Wound construction. It may be difficult to create a sclerocorneal tunnel incision in the presence of conjunctival scarring. A clear corneal incision is recommended in such eyes.
Capsulorrhexis. As discussed above, capsulorrhexis may be difficult due to a lack of posterior support. In addition, visualization may be hindered by a poor red reflex caused by a dense cataract and capsular fibrosis. The use of Trypan blue should be considered to improve visualization of the anterior capsule. However, the surgeon should be aware that Trypan blue changes the elastic property of the capsule, which becomes more fragile and less elastic.
Hydrodissection. Hydrodissection should be slow and gentle because of the possibility of preexisting posterior capsular and zonular compromise. During this process, the surgeon should allow for egress of ophthalmic viscoelastic device so as to prevent posterior dislocation of the lens through an occult injury to the posterior capsule and/or zonules. If posterior capsule damage is known to be present, hydrodissection may be omitted.
Phacoemulsification. Post-PPV eyes have deep and unstable anterior chambers compared with nonvitrectomized eyes.3,4 If intraoperative fluctuation of anterior chamber depth occurs, the bottle height should be lowered and the irrigation maintained to help stabilize the anterior chamber.
Eyes with compromised zonules or posterior capsule damage are at risk for fluid misdirection syndrome, which is indicated by narrowing of the anterior chamber, a hard eye, and iris prolapse. In this condition, fluid flows into the posterior segment, and the ciliary body rotates anteriorly, blocking flow from posterior to anterior. Thus, raising the bottle will, paradoxically, cause more fluid to flow posteriorly, further shallowing the anterior segment and hardening the eye.
Fluid misdirection is managed by halting irrigation and putting external pressure on the incision to stop leakage. This anterior pressure counteracts the posterior pressure; the anterior chamber will deepen, and the eye will soften as the fluid equilibrates.
Techniques for dismantling the cataractous lens must be considered carefully. Both nuclear sclerotic and posterior subcapsular cataracts are common after PPV. Nuclear sclerotic cataracts are hard. In this situation, the surgeon should consider a vertical chop technique, which puts less stress on the zonules and creates less torque than does a horizontal chop technique.
Because posterior subcapsular cataracts tend to be dense and adherent, it may be safer to place the IOL in the capsular bag and perform a YAG capsulotomy after the eye is healed.
|
Web Extra: Ophthalmic Pearls
|
 |
IOL Selection and Placement
The surgeon should have calculations available for a 3-piece IOL to be placed into either the capsular bag or the ciliary sulcus. If there is zonular compromise, a 1-piece or a 3-piece IOL can be placed into the capsular bag with the haptics in the meridian of the zonular compromise.
If there is compromise of the posterior capsule, a 3-piece IOL may be placed in the ciliary sulcus. A 1-piece IOL should never be placed into the ciliary sulcus due to the risk of iris chafe and chronic uveitis.
In the case of anterior capsule compromise, an anterior chamber IOL should be considered, and the calculations should be available for that scenario. When an anterior chamber IOL is used, it is advisable to perform a peripheral iridectomy to avoid pupillary block. IOL placement may be confirmed with intraoperative aerial gonioscopy, as described by Dr. Charles Kelman.
Zonular weakness or loss during cataract surgery may necessitate the use of a capsular tension ring to provide stable support for placing the IOL. The ring should be placed with its opening 180 degrees from the area of zonular weakness.
The cataract surgeon should prepare for these possibilities and make sure that the appropriate instruments and supplies are readily available. However, complications may still occur despite precautions. Such instances emphasize the need for careful patient preparation and consent in the preoperative period.
Postoperative Considerations
Whether the cataract surgery was complicated or uneventful, there are important considerations for the postoperative care of these patients.
Short-term care. In eyes with capsular or zonular complications, complete removal of the viscoelastic is rarely possible. Thus, it is our practice to treat these patients prophylactically with oral or intravenous acetazolamide in the recovery area to avoid IOP elevation in the immediate postop period.
The cataract surgeon should consider performing dilated ophthalmoscopy in the immediate postoperative period, especially if the cataract had prevented an adequate view of the posterior segment. The cataract surgeon may also wish to consult with the vitreoretinal surgeon.
Long-term care. The risk of posterior capsule opacification is higher in these patients, and Nd:YAG capsulotomy may be necessary to achieve best visual outcome.2,3 Patients who underwent PPV for repair of retinal detachment have a higher risk of retinal redetachment following cataract surgery, with a rate of 5.6% in one study.2
Patient care should be coordinated between the cataract and vitreoretinal surgeon to evaluate for these potential postoperative complications. Patients should be counseled about these complications, which may occur months, or even years, after cataract surgery.
Results
Although these eyes carry a higher risk and may warrant a customized approach, phacoemulsification in post-PPV eyes generally yields good visual outcome, with up to 90% of patients seeing improvement in BCVA, and 75% attaining 20/40 or better.3 In the hands of an experienced cataract surgeon, complications can be minimized and may not be greater than in non-PPV eyes.5
___________________________
1 Jackson TL et al. Eye (Lond). 2013;27(5):644-651.
2 Cole CJ, Charteris DG. Eye (Lond). 2009;23(6):1377-1381.
3 Chang MA et al. Ophthalmology. 2002;109(5):948-954.
4 Akinci A et al. Int J Clin Pract. 2008;62(5):770-775.
5 Misra A, Burton RL. J Cataract Refract Surg. 2005;31(5):1011-1014.
___________________________
Dr. van der Vaart is a resident, and Dr. Cohen is the Sterling A. Barrett Distinguished Professor; both are in the department of ophthalmology at the University of North Carolina at Chapel Hill. Relevant financial dislosures: None.