By Jonathan T. Zoghby, MD, and Kenneth L. Cohen, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Corneal incision contracture (CIC), commonly known as corneal wound burn, is an uncommon but potentially serious complication that can result from even the most routine cataract surgical procedure.
Various factors contribute to the generation of high heat from the ultrasonic movement of the phacoemulsification needle, which is then transferred to the incision and leads to acute collagen contracture and distortion of the incision. This occurs once temperature at the incision reaches 60° centigrade.1
Several studies have published different rates of CIC; the largest survey in the United States and Canada documented an incidence of 0.037 percent.1 In an era in which patients expect postoperative perfection, CIC and its associated sequelae—corneal or scleral melting, wound gape, aqueous leakage, hypotony, iris atrophy, iris holes, synechiae, and/or irregular astigmatism—can result in loss of BCVA and a profoundly dissatisfied patient.
This review will look at the factors that are associated with CIC, techniques to reduce its incidence, and potential treatments.
Causes and Prevention
Although a number of different factors have been postulated to contribute to the development of CIC, only three were confirmed in a large-scale multivariate analysis.1
Surgical volume. There is a statistically significant decrease of 45 percent in the incidence of CIC with each doubling of the surgeon’s case load.1 This is not a modifiable factor.
Technique. With regard to techniques used for nuclear disassembly, those that use less ultrasound energy to divide the nucleus result in a lower incidence of CIC. The lowest incidence is seen with prechopping; conversely, the highest incidence occurs when divide-and-conquer, stop-and-chop, and carousel techniques are employed.2 Advanced disassembly methods (such as phaco-flip, horizontal chop, and vertical chop) were associated with the lowest risk because use of ultrasound energy is minimized.2
As the divide-and-conquer method is the most popular approach used in the United States today, this risk factor can easily be modified by learning and perfecting alternative nuclear disassembly techniques.
OVD choice. The use of ultrasound energy within an ophthalmic viscosur
gical device (OVD) causes an exothermic, or heat-releasing, reaction, which varies according to the characteristics of the specific OVD. The highest rate of CIC has been reported to occur with the use of Healon 5, followed by Ocucoat and Viscoat.1
In addition to remaining mindful of OVD selection as a variable, avoiding overfill can reduce the risk of CIC (see below).
 |
|
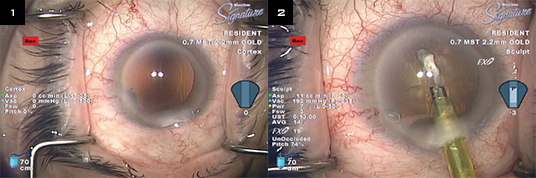
SIGNS OF TROUBLE. Intraoperative signs of a CIC include (1) whitening of the cornea at the incision and (2) lens "dust" or "milk" around the phaco needle.
|
Detection and Management
With CIC, early detection is important, as it can mean the difference between simply suturing the incision and managing complex sclerocorneal melt with resulting visually disabling irregular astigmatism.
Moreover, proper understanding of phacodynamics and fluidics is an important part of preoperative planning. A breakdown in either of these processes can lead to CIC.
Signs. Signs of CIC include whitening of the cornea at the incision (Fig. 1), lens “dust” or “milk” appearing around the phacoemulsification needle (Fig. 2), and gaping of the incision. If the CIC is not severe and is not recognized until the end of the operation, it can manifest as difficulty obtaining a watertight closure.
Management. If any of the above signs are noted during the operation, it is imperative to come out of foot position 3 and assess the etiology of the CIC as follows.
- Check equipment. Is the sleeve appropriate for the incision size and the phacoemulsification needle diameter? If not, then remove the handpiece and correct the situation. Power modulation and incision size have not been found to be associated with CIC. Nevertheless, it is important to make sure that the correct combination of irrigation sleeve, incision size, and phacoemulsification needle size is selected to ensure that there is no restriction to irrigation inflow.1
- Observe movement. After insertion of the phacoemulsification needle into the anterior chamber but before the initiation of ultrasonic energy, the surgeon—using only irrigation and aspiration—should ensure that there is adequate movement of fluid in the anterior chamber. If not, temporarily increase the vacuum until there is visually confirmed movement of cortical material into the needle. Then reduce the vacuum to its previous level once good movement is noted prior to starting nuclear disassembly.
- Correct OVD overfill. Is the anterior chamber overfilled with OVD? Many techniques have been described to help mitigate the risk associated with OVD use, but the easiest one to implement involves not overfilling the anterior chamber with OVD and making sure you have good movement of fluid within the anterior chamber prior to using any ultrasound energy.
To create a fluid pocket, aspirate the anterior cortex, epinucleus, and OVD just anterior to the lens. This will create a space between the crystalline lens and the surrounding OVD, which will still protect the endothelium and maintain the anterior chamber. Backpressure against irrigation will be reduced. There will be less OVD in contact with the needle, thus minimizing any excess heat production and resulting thermal damage.
 |
|
WOUND LEAK. Attempted suture closure of wound burn.
|
Treatment
Once CIC occurs, multiple treatment modalities may be considered. Placing interrupted suture(s) may or may not close the incision gape and prevent leakage of aqueous (Fig. 3). It is imperative that the incision be evaluated intraoperatively to determine whether it is Seidel negative. If there is a leak, advanced suturing techniques such as a gape suture should be used.3
Postoperatively, a small wound leak can be managed with a bandage contact lens and/or tissue adhesive. Aqueous suppressants should be considered. If there is a postoperative incision leak, the surgeon may consider a suture revision or increase the frequency of antibiotic drops. In addition, daily follow-up should be established. Residual astigmatism may be corrected with spectacles or a contact lens, and astigmatic keratotomy may be considered.
___________________________
1 Sorensen T et al. J Cataract Refract Surg. 2012;38(2):227-233.
2 Bradley MJ, Olson RJ. Am J Ophthalmol. 2006;141(1):222-224.
3 Sippel KC, Pineda R Jr. Semin Ophthalmol. 2002;17(3-4):102-109.
___________________________
Dr. Zoghby is a resident in ophthalmology and Dr. Cohen is professor of ophthalmology; both are at the University of North Carolina at Chapel Hill. The authors report no related financial interests.