By Gabrielle Weiner, Contributing Writer, interviewing J. Bradley Randleman, MD, Sonal S. Tuli, MD, and David Varssano, MD
Download PDF
Corneal cross-linking (CXL) has been around since the late 1990s, but as of press time, it still awaits U.S. Food and Drug Administration (FDA) approval. Among international practitioners in the field, there is a consensus that CXL is a useful treatment for keratoconus and corneal ectasia, decreasing the progression of these diseases. There is also preliminary research supporting its use in treating corneal infections.
In the United States, cautious optimism defines the attitude toward CXL, as experts await—many impatiently, at this point—FDA approval for treating keratoconus. “We’re probably the last country to make CXL available. We are ready for it, and I believe we have the data to support FDA approval immediately,” said J. Bradley Randleman, MD, at Emory University School of Medicine in Atlanta. Approval has been anticipated since 2011, when Avedro’s riboflavin ophthalmic solution, used in conjunction with the company’s proprietary UVA irradiation system, was awarded orphan drug status by the FDA. So far, Avedro is the only company in the United States to submit data to the FDA from a clinical trial on CXL, but other trials are ongoing.
Infection: Nascent Evidence
Studies on CXL for corneal infections have been sporadic and limited to its use as a second-line treatment for severe refractory infectious keratitis. “There are case reports, but only a handful of controlled studies that show efficacy, and even those have very low numbers,” said Sonal S. Tuli, MD, at the University of Florida in Gainesville. Some studies have shown a benefit. One of these is the 2014 Geneva-Cairo trial—the first randomized prospective trial on CXL for bacterial keratitis—which reported a reduction in perforation, but no improvement in vision or the ulcer itself.1 There are also studies that show harm. For example, a 2015 study on deep stromal fungal keratitis demonstrated increased perforation and higher failure rates in patients receiving CXL.2
The theory behind using CXL for infection is to strengthen the cornea and thereby protect it from melting, while killing the infectious organism. CXL kills a range of microbes by causing irreversible damage to their RNA and DNA.3,4 “Research has shown positive results for patients with some multidrug-resistant bacteria and for some patients with severe fungal keratitis, but results have been mixed for using CXL for Acanthamoeba,” said Dr. Randleman. Dr. Tuli noted that the kill rates achieved with CXL are far lower than those achieved with antibiotics.
David Varssano, MD, at Tel Aviv University, in Israel, said that the depth of the ulcer plays an important role. “We know that CXL is less effective in the deeper layers of the cornea.”
Dr. Varssano, a coauthor of a recent study on the antibacterial activity of CXL in cases of severe infectious keratitis, is confident about the potential of CXL for treating infections. In this case series of 6 patients with severe infectious keratitis treated with CXL, patients showed rapid clinical improvement and significant subjective relief.5 The paper suggests that CXL be considered as part of the first-line treatment in cases of severe corneal infections. An earlier pilot study on CXL as a primary treatment reported similar results.6
Dr. Tuli countered that the reason corneas melt is that microbes and inflammatory cells in the eye produce collagenases, which break down collagen. “Inhibiting the source of the collagenases with drugs such as doxycycline and vitamin C, in addition to antimicrobial therapy, would be superior to cross-linking. [CXL] does nothing to the collagenases, although it does have some antimicrobial effects,” said Dr. Tuli. From her perspective, a randomized study comparing the perforation rate with CXL versus doxycycline plus vitamin C is needed to test whether CXL has a beneficial effect on corneal melting. “Unfortunately, such a trial would have to be very large, as perforations are uncommon, which makes it cost prohibitive,” she said.
Safety
“CXL [for ectasia] is a relatively safe procedure, with few patients suffering long-term side effects,” said Dr. Varssano. “That said, delayed epithelial growth, scarring, refractive changes, and endothelial damage can and do happen, sometimes causing permanent visual deterioration.” Indeed, many questions about CXL remain—for example, the optimal duration of treatment exposure and the minimum corneal thickness required for safe treatment.
Contraindications against treating ectatic corneas include corneal thickness of less than 400 μm, prior herpetic infection, severe corneal scarring or opacification, history of poor epithelial wound healing, severe ocular surface disease such as dry eye, and autoimmune disorders.7 These limitations do not appear as relevant for treating infectious keratitis, said Dr. Varssano.
“Cross-linking is not currently the standard of care for infectious keratitis,” said Dr. Randleman, but he added that it may be “a good alternative for corneal infections when other treatments have failed; and it may prove extremely useful in situations where access to antibiotic medications is limited or there are concerns about compliance or patient follow-up.”
Candidate Criteria
Dr. Varssano outlined his use of CXL as follows: “I tend to treat infections with CXL in cases that do not seem to respond to topical antimicrobial treatment, especially if culture results are not informative. I treat both superficial and deep infiltrates, although I assume the latter will be less affected by the treatment. I am sure my preferences will change in the next few years with added knowledge. History of refractive surgery is irrelevant to my decision. And I may use CXL as a primary treatment for selected cases in the future.”
If and when FDA approval comes, Dr. Tuli would use CXL only for infectious indications in cases not responding to medication, as a final attempt to sterilize the ulcer in order to avoid a therapeutic transplant.
Clinical Advice
Patient follow-up after procedure abroad. If you have a patient who has been treated in another country with CXL for microbial ulcer, your follow-up regimen should be similar to that used for traditional treatment with topical antimicrobial agents, according to Dr. Varssano. (In patients treated with CXL for ectasia, topography and refraction should be done every 3 months for at least a year, then according to clinical judgment, but not less often than every 12 months for several years. Retreatment can be performed if stability is not achieved, he said.)
Tips for performing CXL. Transepithelial (epi-on) versus epi-off treatment is still a controversial issue, but Dr. Varssano advised removing the epithelium over the entire infiltrate, plus a safety margin. He also warned against unnecessary treatment over the pupil.
The Future
Dr. Randleman does not anticipate CXL ever being approved for infectious indications. “Not a single antibiotic drop has ever been directly approved for corneal ulcers due to the challenges of such a study and associated costs, and that’s the gold standard of care.”
“It would be nice to have a way of cross-linking that is safer,” said Dr. Tuli, for instance, with medications. Although formaldehyde couldn’t be used on the cornea, it is an example of an agent that cross-links very well. “There may be other substances that induce cross-linking safely. Then we wouldn’t have to use UV light, which is the source of complications.” If CXL continues to include UV, the key will be to shorten exposure times as much as possible, Dr. Tuli noted. In the grand scheme of things, Dr. Randleman said, “If we could make infectious keratitis a clinical diagnosis and a one-time treatment in the office with CXL, that would be a complete paradigm shift in treating corneal ulcers! Could you imagine that?”
___________________________
1 Said D et al. Ophthalmology. 2014;121(7):1377-1382.
2 Uddaraju M et al. Am J Ophthalmol. 2015;160(1):131-134.e5.
3 Makdoumi K et al. Graefes Arch Clin Exp Ophthalmol. 2010;248(2):207-212.
4 Schnitzler E et al. Klin Monatsbl Augenheilkd. 2000;217(3):190-193.
5 Skaat A et al. Eur J Ophthalmol. 2014;24(1):21-28.
6 Makdoumi K et al. Graefes Arch Clin Exp Ophthalmol. 2012;250(1):95-102.
7 http://eyewiki.aao.org/Corneal_Collagen_Cross-Linking.
___________________________
Dr. Randleman is the John H. and Helen S. Hughes Professor of Ophthalmology, Emory University School of Medicine and Director, Cornea, External Disease & Refractive Surgery at Emory Eye Center, Atlanta, Ga. He is also Editor-in-Chief of the Journal of Refractive Surgery. Relevant financial disclosures: None.
Dr. Tuli is professor and chair of ophthalmology, director of the Cornea and External Diseases Service, and residency program director at the University of Florida in Gainesville. Relevant financial disclosures: None.
Dr. Varssano is Head of Cornea Service in the Department of Ophthalmology at Tel Aviv Sourasky Medical Center and Sackler School of Medicine, Tel Aviv University, in Israel. Relevant financial disclosures: None.
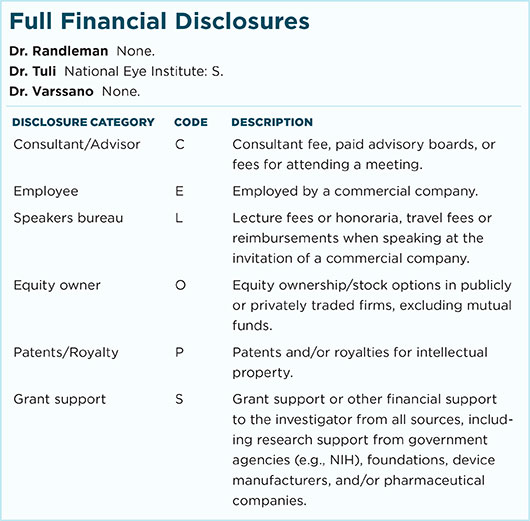
For full disclosures and the disclosure key, see below.