Download PDF
After many years, the landmark Ocular Hypertension Treatment Study (OHTS) is still broadening our understanding of risk factors for glaucoma. A recent long-term study shows that occurrence of an optic disc hemorrhage (ODH) strongly predicts subsequent development of primary open-angle glaucoma (POAG) in patients with ocular hypertension (OHT). Having a disc hemorrhage increased the risk of developing POAG 2.6-fold, or 260%.1
New factors emerged over time. The 13-year analysis of ODHs in the OHTS population also revealed 3 additional factors that increase the risk of ODH but had not been statistically significant in an interim analysis2: high baseline intraocular pressure (IOP), black race, and assignment to the group of OHTS patients who did not receive medication.
The findings suggest that clinicians should be vigilant in looking for ODHs, said Donald L. Budenz, MD, MPH, Kittner Family Distinguished Professor and Chair, Department of Ophthalmology, University of North Carolina at Chapel Hill.
In this prospective cohort study involving 3,236 eyes of 1,618 OHTS participants, the researchers examined annual stereoscopic optic disc photos to look for ODH. Among the findings:
- In patients with OHT before the development of POAG, the incidence of ODH was 0.5% per year over an average of 13 years, but it more than doubled to 1.2% during an average of 6 years after the development of POAG. (The incidence of ODH may be underestimated because of its transient nature and because people with ODH at baseline were excluded from the study.)
- ODH occurred less frequently in the OHTS medication group (7.4% cumulative incidence at 13 years) compared with the observation group (9.8%).
- While the presence of an ODH was associated with an increased risk of POAG, 78% of eyes with an ODH did not progress to glaucoma over a median follow-up of 49 months after developing the disc hemorrhage.
Clinical implications. Because ODHs are transient, looking for them annually may not be often enough to factor into a treatment algorithm. Dr. Budenz recommends checking carefully for disc hemorrhages at every exam. He said the best way to detect an ODH is with a dilated exam using a 78-D or 90-D condensing lens. But using the direct ophthalmoscope on an undilated patient is a reasonable alternative between annual dilated exams.
If an ODH is detected, he advised additional testing over the next 3 to 6 months. Changes in the visual field, optic nerve, or retinal nerve fiber layer, particularly if they correspond to the location of the optic disc hemorrhage, are indications for treatment.
Dr. Budenz stressed that initiating treatment of every OHT patient with a disc hemorrhage is not advised. “It’s important to remember that most OHT patients will not develop POAG after disc hemorrhage,” he said. It is, however, reasonable to start treatment in the presence of additional risk factors: older age, low corneal thickness, increased vertical cup/disc ratio, greater pattern standard deviation, and increased IOP.
In light of the findings, Dr. Budenz has become more vigilant in looking for disc hemorrhages in all of his OHT and glaucoma suspect patients. “It may be more important than measuring IOP at each exam because finding a disc hemorrhage likely increases the risk more than detecting a modest elevation in IOP.”
—Miriam Karmel
___________________________
1 Budenz DL et al. Am J Ophthalmol. 2017;174:126-133.
2 Budenz DL et al. Ophthalmology. 2006;113(12):2137-2143.
___________________________
Relevant financial disclosure—Dr. Budenz: None.
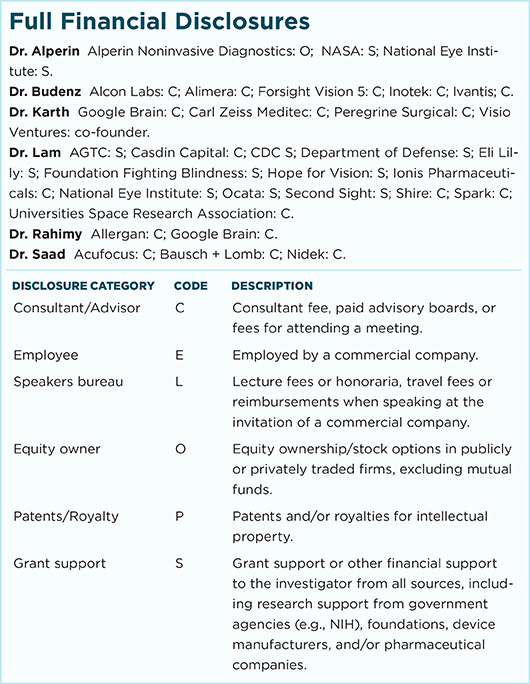
For full disclosures and disclosure key, see below.
More from this month’s News in Review