Download PDF
Evidence is building that there is a new patient risk factor for cataract surgeons to consider during preoperative planning: prior intravitreal injections.
Even a single intravitreal injection at some point in the past significantly raises the risk of posterior capsular rupture (PCR) during a later cataract surgery, British researchers have found.1
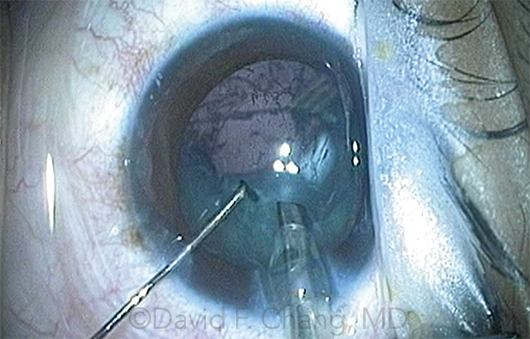 |
RUPTURE RISK. In the latest study, previous intravitreal injections were associated with a 66% increase in the risk of posterior capsular rupture (shown here).
|
More patients at risk. At a time when intravitreal injections are being performed to treat a wide variety of retinal problems, this risk could affect a significant segment of the cataract surgery population, the authors warned. They found that intravitreal injections were associated with a 66% rise in risk for PCR during cataract surgery.
“Given the increased risk, surgery should be performed by cataract surgeons able to amend their surgical technique according to need,” the researchers wrote. They further advised that preoperative biometry “should provide lens powers for sulcus 3-piece intraocular lens options, and anterior vitrectomy with triamcinolone should be available if required.”
EHR review. The London researchers gleaned their evidence for this new risk factor from a retrospective review of the electronic health records (EHRs) of 62,994 cataract procedures performed at Moorfields Eye Hospital in London. Capsular rupture occurred in 1.04% of the eyes in the total cohort. However, among the 1,035 eyes with an intravitreal injection history, the PCR rate was 1.88%, they reported.
“These eyes are certainly not routine eyes,” said coauthor Zaid Shalchi, FRCOphth, MRCP, MSc. “This is important when counseling patients for surgery, as well as when deciding on the seniority of the surgeon undertaking the surgery.”
Building on earlier reports. The group’s findings were similar to those reported by 3 groups of U.S. and U.K. researchers during 2016. One U.S. group analyzed Medicare data and found that patients with prior intravitreal injections had a significantly increased risk of requiring removal of retained lens fragments within 28 days of surgery.2 In another U.S. study, researchers found a higher risk of PCR among 197 previously injected eyes than in matched controls.3
The third study also combed thousands of EHR records to uncover a direct association between intravitreal injections and the risk of PCR.4
Question of dose response. In the third study, researchers concluded that the risk of PCR increased by 4% with each additional injection an eye had received, Dr. Shalchi noted. In contrast, Dr. Shalchi said that his group could not find any difference in risk between eyes that had a single injection and those that received 10 or more.
“We did not find a dose response,” he said. “It is a reminder that we still do not understand what leads to PCR in these eyes. Further work is necessary to consider potential hypotheses, such as weakness of the capsule due to previous trauma from injections.”
—Linda Roach
___________________________
1 Shalchi Z et al. Am J Ophthalmol. 2017;177:77-80.
2 Hahn P et al. Ophthalmology. 2016;123(2):309-315.
3 Hahn P et al. Eye (Lond). 2016;30(8):1101-1109.
4 Lee AY et al. Ophthalmology. 2016;123(6):1252-1256.
___________________________
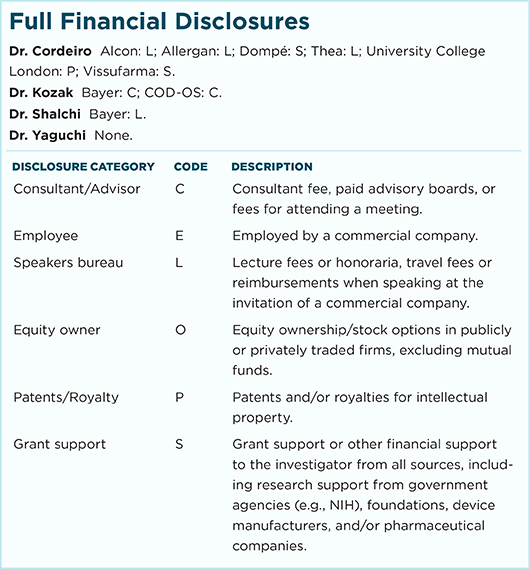
Relevant financial disclosures—Dr. Shalchi: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review