This article is from March 2007 and may contain outdated material.
While cataract surgery for patients with pseudoexfoliation is much safer than it once was, “We still think that pseudoexfoliation deserves special attention,” said I. Howard Fine, MD. “It is not infrequently connected with glaucoma, small pupils and compromised zonular integrity, for instance. These and other issues must be addressed.”
Below, Dr. Fine and two other experts offer tips in six strategic areas that can help reduce the risk of intra- and postoperative complications.
Strategy #1: Before Surgery, Assess Confounding Problems
If a patient has glaucoma, “First, get the glaucoma under control, then see how well the pupil dilates,” said Dr. Fine, clinical professor of ophthalmology at Oregon Health & Science University and in private practice in Eugene. With regard to medication, he avoids prostaglandins because of the postoperative risk of macular edema.
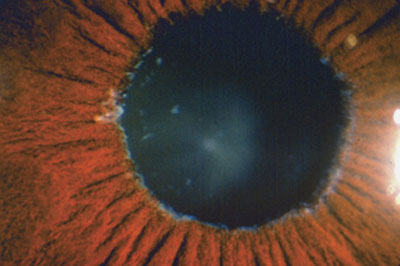
Weak zonules are of particular concern. “There is a wide range of zonulopathy in cataract patients with pseudoexfoliation, ranging from seemingly normal zonular tension to frank phacodonesis,” said David F. Chang, MD, clinical professor of ophthalmology at the University of California, San Francisco, and in private practice in Los Altos. “Two preoperative signs in particular forewarn me of weak zonules: Patients with very poor dilation and obvious white accumulation on the pupillary margin will tend to have more advanced zonular weakness. Another red flag is a shallow chamber despite a normal axial length.”
 |
|
Pseudoexfoliative material at the pupillary margin.
|
Strategy #2: Prepare for Small Pupils
The small pupil can be managed in several ways, including iris hooks and rings. “Most of the time, I prefer stretching the pupil,” said Mark Packer, MD, clinical associate professor of ophthalmology at Oregon Health & Science University and in private practice in Eugene.
“I use a Beehler dilator, a two- or three-pronged device, which gives a nice symmetrical stretch. You will still get some damage to the sphincter muscle, because stretching essentially creates microsphincterotomies. Then, I like to use Healon 5 to maintain the enlargement of the pupil. This is my usual approach.”
In cases in which this isn’t adequate, Dr. Packer usually turns to pupil rings. “Hooks tend to produce bleeding due to the necessary posterior location of the incisions; they’re a little messier. Rings protect the pupil margin—you won’t inadvertently snag the iris in the phaco needle—and a circle gives you the most exposure.”
Dr. Chang noted, “Mechanical pupil stretching works quite well with the fibrotic pupillary margins of pseudoexfoliation patients. However, I might use iris retractors to maximize my exposure if there are multiple other risk factors, such as a brunescent lens, a crowded anterior chamber, intraoperative floppy iris syndrome or a history of weak zonules in the contralateral eye.”
Strategy #3: Take Care With the Capsulorhexis
The capsulotomy requires special care and attention, the experts agree, given the potential threat to weakened zonules. “You need to look for any wrinkling in the lens capsule during the capsulorhexis—if you see wrinkling, that’s an area of zonular weakness and a definite sign for putting a capsular tension ring in,” Dr. Packer said.
“Controlling the capsulorhexis is difficult in the presence of weak zonules because the capsule is ‘pseudoelastic,’” Dr. Chang noted.
“Without good zonular countertraction, the peripheral capsule moves along with the advancing flap, as though it were of an elastic material. Because the capsulorhexis is so crucial, if I see pseudoelasticity, I err on the side of a smaller diameter to maximize control and to avoid a radial tear.”
Other surgeons prefer a larger rhexis, noting that pseudoexfoliation patients are particularly susceptible to marked shrinkage of the rhexis. However, Dr. Chang said, “Depending on the degree of zonular weakness, there are three strategies to counter capsule contraction. I would first implant a capsular tension ring. After the IOL has been implanted, I then enlarge the capsulorhexis by making a small oblique snip with microscissors, and re-tearing it. In doing so, I might try to extend the capsulorhexis out to or beyond the optic edge, which really reduces its tendency to contract. Finally, making a few small relaxing cuts in the capsulorhexis edge [away from the haptic] would accomplish the same thing.”
Strategy #4: Watch for Stress on Zonules
To minimize the amount of stress placed on the zonules, Dr. Fine said that he uses “hydrodelineation and a horizontal chop, never pushing down on the lens.”
Hydrodelineation produces an epinuclear shell, which acts as a safeguard. As for chopping vs. grooving and cracking techniques, “With phaco chop, the nucleus is fragmented by the mechanical force of the chopper moving forward and against the phaco tip,” Dr. Chang said. “Miyake-Apple video analysis shows that this significantly reduces zonular stress, as compared with dividing a dense nucleus with sculpting.”
Cortical cleanup can be “very difficult” with pseudoexfoliation patients, Dr. Fine noted. If there are areas of zonular dehiscence, “strip tangentially toward the dehiscence.” Do not strip away from the dehiscence, as that will localize forces on the weakened zonules and may unzip the dehiscence.
Strategy #5: Choose the Best IOL
“With very weak zonules, we must worry about capsule contraction syndrome and delayed bag-IOL dislocation postoperatively,” Dr. Chang said. “I select a three-piece hydrophobic acrylic IOL to provide the stiffest haptics possible and to minimize anterior capsule fibrosis.”
Overall, you’ll see less capsular contraction with acrylic IOLs, Dr. Fine agreed. “We try to not use silicone lenses, as they stimulate anterior subcapsular cells to produce extracellular matrix—and as this contains collagen precursors, it promotes contraction and phimosis.”
Strategy #6: Consider Capsular Tension Rings
“I don’t use CTRs in every case of pseudoexfoliation, though many surgeons do,” Dr. Packer said. Dr. Fine, who uses CTRs “100 percent of the time because they add safety,” noted that “they will add centration of the IOL.” However, he acknowledged, “This is not indefinite, long-term centration.” Nonetheless, “if the lens does detach, as the zonular apparatus continues to deteriorate, the ring can be sutured to the sclera in any meridian.”
One question up for consideration is, when do you put the CTR in—at the beginning of surgery or later? Dr. Packer, who acknowledged that this is a controversial area, said, “I’m a strong proponent of putting them in at the beginning, although most physicians wait until the end of surgery.”
Either way, putting in a CTR is not a completely atraumatic process, he said. “Whether it’s before phaco or after phaco, it will still put stress on zonules. The advantage to earlier implantation is that it prevents damage to the bag during phaco.”
Dr. Packer pointed out that “removal of cortex is more difficult when a CTR is in place, as it pins the cortex against the bag. You have to strip the cortex tangentially, and that takes a little longer. Your trade-off is confidence that it’s stabilizing the capsule during phaco, putting the posterior capsule on stretch and preventing damage. I don’t mind taking the extra time—in my mind, that doesn’t outweigh the benefits.”
Overall, in the long term, Dr. Packer said, a CTR “doesn’t prevent subluxation or dislocation of the whole complex, and it doesn’t prevent phimosis either —those arguments for its use are moot. The clear benefit is that if you have a bag that’s decentered, the CTR will center it during surgery.”
_____________________________
Drs. Chang, Fine and Packer are consultants for AMO. Dr. Chang is also a consultant for Alcon.