Download PDF
The latest study from the Diabetic Retinopathy Clinical Research Network (DRCR.net) supports the use of ranibizumab as an alternative to panretinal photocoagulation (PRP) to prevent worsening of proliferative diabetic retinopathy (PDR).1
At 2 years, eyes treated with ranibizumab experienced fewer worsening events—defined as vitreous hemorrhage, retinal detachment, anterior segment neovascularization, or neovascular glaucoma—than those receiving PRP. The cumulative probability was 34% for ranibizumab compared with 42% for PRP. “Panretinal photocoagulation has been the gold standard for 40 years, but physicians now have a new option for treating patients,” said Lee Jampol, MD, chair of the DRCR.net.
Other factors affecting outcomes. The randomized clinical trial at 55 U.S. sites involved 394 eyes of 305 adults with PDR and no previous PRP; 191 eyes were assigned to ranibizumab and 203 to PRP. However, regardless of group assignment, the study protocol required all eyes with vision-impairing center-involved diabetic macular edema (DME) to receive ranibizumab at baseline.
Because this requirement was a potential confounder, the researchers also performed subgroup analysis of eyes without DME—and found that the difference in treatment effect was more robust. In that subgroup, cumulative probability of worsening PDR was 45% with PRP and 31% with ranibizumab.
Regardless of treatment, severity of retinopathy at baseline was the most important factor. The risk of worsening in eyes with PDR classified as high-risk or worse was higher than in eyes with moderate or better PDR (64% vs. 23%, respectively).
Surprise finding. That the specific type of laser therapy makes a difference was unexpected, Dr. Jampol said. Pattern scan PRP was associated with higher risk of worsening than conventional single-spot laser—60% versus 39%, respectively. The finding may be a true effect, he said, or it might be due to chance or potential bias, as the choice of laser type was left to investigator discretion.
Clinical implications. Although the results support the use of ranibizumab, Dr. Jampol noted that “PRP is still the choice for many clinicians and patients, particularly if anti-VEGF treatment is unavailable or if there is a concern regarding patient compliance with follow-up visits.”
The researchers plans to follow these patients through 5 years. In the meantime, they emphasized: “Diligent follow-up of patients is required because more than one-third of eyes treated with either approach may experience a PDR-worsening event in this period.”
—Miriam Karmel
___________________________
1 Bressler SB et al. Ophthalmology. 2017;124(4):431-439.
___________________________
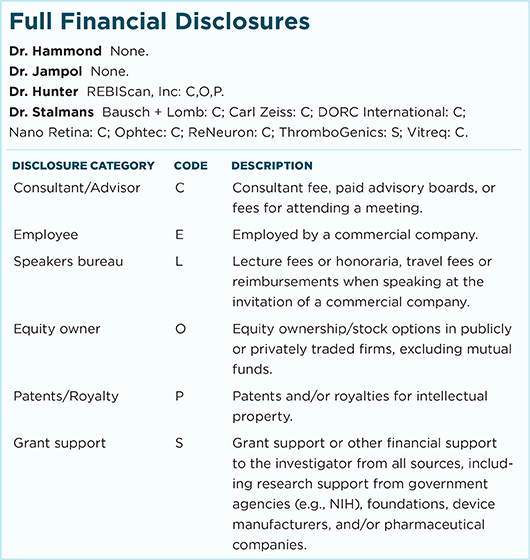
Relevant financial disclosures—Dr. Jampol: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review