Download PDF
In a multicenter randomized clinical trial involving patients with angle-closure glaucoma or angle closure with high intraocular pressure (IOP), those who underwent clear-lens extraction (CLE) did better than those who received standard-of-care laser peripheral iridotomy (LPI).1 Researchers reporting on the EAGLE trial said that CLE is a reasonable first-line treatment option for angle-closure patients.
Methods and participants. The trial enrolled phakic patients aged 50 years and older who had either newly diagnosed primary angle-closure glaucoma (n = 263) or primary angle closure with IOP of 30 mm Hg or greater (n = 155). Half of the patients underwent CLE by phacoemulsification with monofocal intraocular lens (IOL) implantation, while the other half received LPI.
The study measured all medical care costs for each participant during 3 years of follow-up. It also evaluated changes in quality of life.
 |
ANGLE CLOSURE—WHAT NEXT? Although the first-line therapy for angle closure is typically laser peripheral iridotomy, a new study suggests that clear lens extraction may be a better option for some patients.
|
Results favor CLE. Early lens extraction proved both more efficacious and cost-effective than LPI. While the differences between the groups were relatively modest, they were statistically and clinically significant, said Augusto Azuara-Blanco, MD, PhD, professor of ophthalmology at the Centre for Public Health, Queen’s University Belfast, in Belfast, Northern Ireland.
Perhaps the most striking difference between the groups was the use of medications or additional procedures to meet the target IOP (15-20 mm Hg): 61% of the LPI group required 1 or more medications, compared with 21% of the CLE group. Further, 24 LPI patients had an additional glaucoma surgical procedure, but only 1 CLE patient did.
Among other findings at 3 years:
- Mean IOP was 1.18 mm Hg lower after CLE than after LPI. According to the researchers, this difference is small because the treating physicians were allowed to use medications or further surgical interventions as needed to achieve the target IOP.
- Quality of life scores were significantly higher in the CLE group.
- Visual acuity was better by 3 ETDRS letters in the CLE group.
- Visual field loss was similar in the 2 treatment groups.
Costs and complications. Costs for the initial procedure were higher for CLE than for LPI (£2,467 vs. £1,486). However, the higher cost was partlyoffset by savings associated with reduced need for medications and/or subsequent procedures, and the cost-effectiveness is expected to improve over time.
While there were no serious adverse events, 25 patients in the CLE group and 50 in the LPI group had at least 1 reported complication. For the CLE group, complications were generally those seen in cataract surgery, including posterior capsule rupture, iris prolapse, and vitreous loss; 3 patients needed intraocular surgery to manage these complications. Among the leading complications in the LPI group were intraoperative bleeding and medication intolerance; in addition, 12 LPI patients required cataract surgery during the 3-year follow-up.
Applying the results to practice. The results cannot be extrapolated to patients outside the study parameters, for example, those younger than 50, said Dr. Azuara-Blanco. Since a younger patient would lose the ability to accommodate with CLE, “we do not know how they would rate their visual function and vision-related quality of life,” he said.
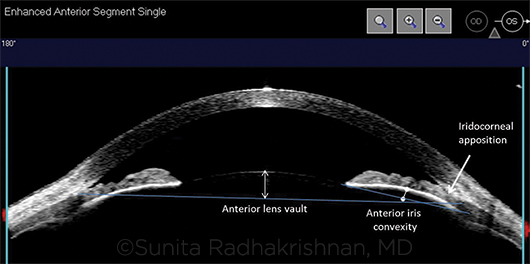
Another consideration for CLE is that angle-closure patients often have smaller eyes with crowded anterior segments. This configuration poses surgical challenges.
Dr. Azuara-Blanco plans to revisit the clinical data in 10 years and expects that, despite these caveats, “longer-term will show an even greater benefit of lens extraction.”
For now, said Dr. Azuara-Blanco, “I tell my patients that the EAGLE trial is providing strong evidence that supports the use of early lens extraction; and if they have this surgery, they are more likely to be better off than with laser. But there is a small risk of having a surgical complication. The final decision needs to be individualized.”
—Miriam Karmel
___________________________
1 Azuara-Blanco A et al. Lancet. 2016;388(10052):1389-1397.
___________________________
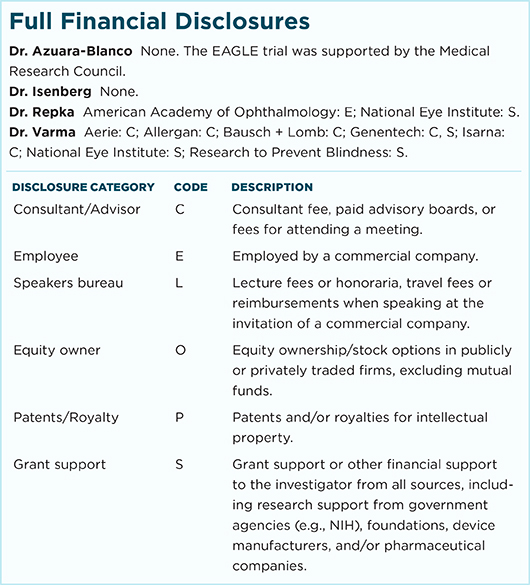
Relevant financial disclosures—Dr. Azuara-Blanco: None. The EAGLE trial was supported by the Medical Research Council.
For full disclosures and disclosure key, see below.
More from this month’s News in Review