By Gabrielle Weiner, Contributing Writer, interviewing Jason J. Jones, MD, Samuel Masket, MD, and Steven I. Rosenfeld, MD, FACS
Download PDF
Posterior capsular tear, or rupture, can occur at various points during cataract surgery and intraocular lens (IOL) insertion. If a single-piece acrylic (SPA) IOL had been selected preoperatively, what would your options be in case of a rupture?
Many surgeons would consider exchanging the SPA IOL for a 3-piece IOL designed for the sulcus. If, however, you have a well-centered and intact anterior capsulotomy, there’s another option: reverse optic capture (ROC).
Defining ROC
ROC is a technique of IOL implantation in which the haptics of a 3-piece or single-piece C-loop haptic lens are posterior to the anterior capsulotomy, while the optic is anterior to the edge of the anterior capsular opening, according to Jason J. Jones, MD, in private practice in Sioux City, Iowa. In terms of method, he said, “It matters little whether the entire lens is placed into the bag and then the optic is brought forward, or the optic is kept anterior to the anterior capsule plane and the haptics are placed into the bag. The result is the same anatomically.” He said that the approach the surgeon chooses will likely depend on when the PC tear is noted and on the size of the tear.
When to consider ROC. There are 3 scenarios in which ROC is useful:
- Treatment for symptomatic negative dysphotopsia (ROC’s best-known use). In 2011, Masket and Fram reported early results.1
- Prevention of rotation of a toric SPA. Gimbel et al. reported a successful case in 2013.2
- Posterior capsular rupture (PCR), when the surgeon wants to use an SPA lens. Jones et al. published a retrospective study in 2012.3
ROC for PCR. In the case of a PCR, if the surgeon were to implant the entire posterior chamber IOL in the capsular bag, the size of the tear could increase, leading to risk of a dislocated IOL. Conversion to a 3-piece IOL in the sulcus is an option, said Steven I. Rosenfeld, MD, FACS, but “ROC enables placement of the optic in the posterior chamber in the same effective lens position as would be obtained in an uncomplicated case. In general, this technique allows the surgeon to use the same style IOL and IOL power that was ordered for the case, except in cases of very-high-power IOLs.” Dr. Rosenfeld is in private practice in Delray Beach, Fla.
History. The concept of using the capsulotomy for optic capture was introduced after the development of continuous curvilinear capsulorrhexis (CCC), explained Samuel Masket, MD, in private practice at Advanced Vision Care in Los Angeles. The traditional posterior optic capture was used with 3-piece lenses, where the loops of the IOL were left in the ciliary sulcus in the posterior chamber and the optic was prolapsed posteriorly through the anterior capsulotomy.
“With the advent of SPA lenses, we learned that their design, in particular the thick haptics, is not compatible with posterior iris contact. So in the case of PCR, if you still want to implant an SPA lens, you can put the haptics behind the anterior capsule but then prolapse the optic anteriorly.” This is referred to as a reverse, or anterior, optic capture. “With ROC, you keep the thick haptics away from the iris, where they can induce damage that might, for instance, lead to uveitis-glaucoma-hyphema [UGH] syndrome,” Dr. Masket said. The bottom line is that you can use a well-sized and well-positioned anterior capsulotomy to capture the optic anteriorly or posteriorly through the capsulotomy, but in the case of an SPA lens, it’s inappropriate to put the haptics anterior to the capsule.
ROC Criteria
Whether ROC can be performed in the setting of PCR depends on the specifics of the case. This technique requires that the anterior capsular rim of the capsulorrhexis be intact for the full 360 degrees (no anterior radial tear), said Dr. Rosenfeld. “If vitreous is present in the anterior chamber or extending up to the cataract incision, a vitrectomy should be performed using whatever technique the surgeon is most comfortable with, either an anterior vitrectomy or a pars plana vitrectomy,” Dr. Rosenfeld said. Dr. Jones added that the anterior capsular opening must be smaller than the optic, centered appropriately, and relatively circular and symmetric.
How It’s Done
In Dr. Jones’ experience, the lens is injected anterior to the capsulotomy using the manufacturer’s cartridge, while a spatula through the paracentesis provides countertraction. The spatula also serves as a manipulator when placed posterior to the optic as the lens is injected. The lead haptic is positioned into the nasal capsular fornix, with the spatula behind the optic. The surgeon then hands off the injector and uses a lens manipulator (Kuglen or Sinskey) through the main wound to place the trailing haptic through the capsular opening. As the haptics open, the optic is maintained anterior to the capsular membrane, where it is captured. The capsular opening often takes on a rectangular shape. The spatula and lens manipulator are then withdrawn from the eye. Viscoelastic is evacuated as usual, with the exception of behind the optic, and the wounds are secured (hydration and/or suture closure).
Pros and Cons
Pros. The main advantage of ROC is that the surgeon can use an SPA lens. “These are the most common type of lenses in ORs today and are readily available. The injector system and incision size remain routine,” Dr. Jones said. “SPA lenses have a gentle unfolding and more planar delivery compared to 3-piece IOLs, so less manipulation may be required.” One of the technical benefits of SPAs, Dr. Jones noted, is that designs are available to correct spherical aberration, astigmatism, and presbyopia (multifocal or extended range of vision).
Cons. ROC cannot be performed if the capsulotomy is too big to effectively capture the optic, as may occur with a manually performed CCC. “A femto-made capsulotomy will be smaller than the optic or at least of a known size,” said Dr. Jones.
In ROC, although the haptics are at a distance from the iris, the optic edge is anterior to the capsule and therefore close to the iris plane; this could predispose some patients to iris chafe, pigment dispersion, and UGH syndrome, said Dr. Jones. “It’s important to monitor patients for these potential issues so that they can be addressed early,” he said.
Another potential problem: Fibrotic posterior capsular opacification could result because the optic is not serving to separate the anterior and posterior capsules. Posterior capsular YAG capsulotomy can and should be applied when opacification occurs, said Dr. Jones.
The last drawback is that the more anterior position of the optic might produce a slightly myopic outcome if the same IOL power is used as that selected for in-the-bag placement. In Dr. Jones’ data set, he and his colleagues found that a slight myopic shift occurred within the limited range of lens powers included in the study. “Within a normal range of physiologic powers, adjusting the power by reducing the spherical IOL diopter by 0.5 would be reasonable. At lower powers, no change of lens power would seem advisable. At high powers, the surgeon may want to reduce the lens by 1.0 D,” said Dr. Jones. “These are general guidelines, and I have no specific evidence-based power ranges to suggest. If the planned in-the-bag power is used, a mild myopic result may occur, which is generally very well tolerated.”
Recognizing Posterior Capsular Rupture
PCR incidence is quite low—somewhere between 2% and 3%—but the posterior capsule is only 10 to 20 μm thick, so accidents do happen, said Dr. Masket.
Sometimes it can be challenging to detect a PCR. Dr. Rosenfeld delineated the following signs, many of which can be subtle:
- The anterior chamber deepens.
- The posterior capsule bows posteriorly.
- The lens material moves posteriorly or through the tear into the vitreous cavity.
- It becomes more difficult to engage nuclear material with the phaco tip.
- It becomes more difficult to aspirate cortical material with the I&A tip.
- The vitreous may present itself at the clear corneal incision; the surgeon can confirm this by touching a Merocel sponge to the wound.
- The pupil may become peaked or irregular in shape.
Dr. Rosenfeld emphasized the following tactic: When a PCR occurs, the key is to resist the temptation to withdraw the phaco tip or I&A tip. The surgeon should keep the instrument in the eye, lower the phaco bottle, and inject a dispersive viscoelastic through the side-port incision to keep the anterior chamber formed, thereby preventing the vitreous from prolapsing forward and into the anterior chamber or out the wound. After filling the anterior chamber with viscoelastic and tamponading the vitreous, it is safe to remove the phaco tip or I&A tip from the eye. The point is that if you quickly remove the instrument from the eye as the PCR occurs, you might create a pressure gradient, allowing the vitreous to follow the instrument tip into the area of lower pressure and prolapse out of the wound.
|
Clinical Pearls
Dr. Jones. One key to successful implementation of ROC is being aware of the concept as well as the mechanics of implanting an SPA lens with this technique. (See one of Dr. Jones’ videos here.)
Also, an honest postop discussion with the patient about the events of surgery is prudent, as the refractive outcome may be different from what was intended, and vitreous management may place the patient at risk for retinal issues (e.g., retinal tear or detachment, macular edema).
After surgery, partial posterior capsular membranes may need early postoperative treatment with YAG laser to resolve undesired visual symptoms, he noted.
Dr. Rosenfeld. At the time of the posterior capsular tear, the surgeon must look for vitreous loss or vitreous incarceration. The vitreous has to be dealt with first. Remember to keep the phaco handpiece or I&A tip in the eye and tamponade the vitreous with the injection of a dispersive viscoelastic in the vicinity of the torn capsule. This keeps the vitreous back and prevents or minimizes the vitreous prolapse, before the handpiece is removed.
Regarding IOL selection, multifocal IOLs and toric IOLs can cause significant visual problems, such as glare, dysphotopsias, ghosting, and even loss of best-corrected visual acuity, if they are not properly centered and aligned inside the eye. When a surgeon is in doubt about the structural integrity and centration of the anterior capsular opening, it may be best to use a monofocal IOL instead, and ROC can still be utilized. Make sure that you have alternative IOLs ready to go in your OR at all times.
Dr. Masket. Optic capture requires an intact CCC, so the surgeon has to be very careful not to tear the anterior capsule. When doing ROC with PCR, the surgeon also needs to be cautious not to drop the lens through the capsular defect, as it can fall into the posterior segment, particularly in the case of a postvitrectomy eye. In cases at high risk for PCR—for example, posterior polar cataract—the surgeon may opt for the precision of a femtosecond laser anterior capsulotomy to ensure proper size and centration.
___________________________
ADDITIONAL COVERAGE. David F. Chang, MD, demonstrates ROC in PCR.
___________________________
1 Masket S et al. J Cataract Refract Surg. 2011;37(7):1199-1207.
2 Gimbel HV, Amritanand A. Case Rep Ophthalmol. 2013;4(3):138-143.
3 Jones JJ et al. Ophthalmic Surg Lasers Imaging. 2012;43(6):480-488.
___________________________
Dr. Jones is in private practice at the Jones Eye Clinic in Sioux City, Iowa. Relevant financial disclosures: Abbott Medical Optics: C,L.
Dr. Masket is founding partner of Advanced Vision Care in Los Angeles and is clinical professor of ophthalmology at the David Geffen School of Medicine, Stein Eye Institute, UCLA. Relevant financial disclosures: None.
Dr. Rosenfeld is in private practice with the Delray Eye Associates, PA, in Delray Beach, Fla., and is voluntary professor of ophthalmology at the Bascom Palmer Eye Institute, University of Miami School of Medicine. Relevant financial disclosures: None.
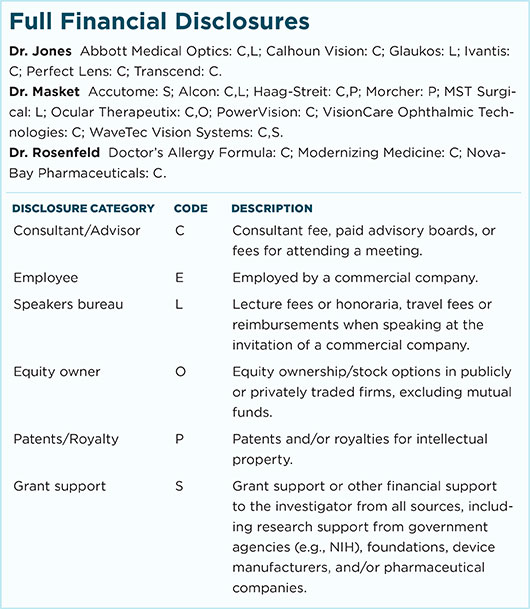
For full disclosures and the disclosure key, see below.