Download PDF
At least one thing is known about nonarteritic anterior ischemic optic neuropathy (NAION): It is a devastating ocular condition that causes permanent visual loss. Researchers have presumed—but not yet proved—its underlying pathophysiology. And, thus far, few risk factors have been found, other than a small optic nerve head with a small cup-to-disc ratio. Due to the low incidence of NAION, previous small studies about its risk factors have lacked statistical power.1
Recently, however, a large retrospective longitudinal cohort study has identified several modifiable risk factors, adding insight into this largely inscrutable condition. Drawing from a pool of nearly 1.4 million eligible enrollees in a large U.S. managed care network, researchers at the University of Michigan and the Massachusetts Eye & Ear Infirmary, Harvard University, assessed more than 20 social, demographic, systemic, and ocular risk factors for NAION among 977 patients who developed the condition between 2001 and 2014.1
Methodology. Beneficiaries between the ages of 40 and 75 with no previous history of NAION at baseline were monitored for at least 2 years and were seen at least twice by an eye care professional. New diagnoses of NAION arising in this group were identified based on ICD-9 billing codes. The researchers excluded conditions that can mimic NAION, such as giant cell arteritis and optic neuritis, as well as patients who had undergone lumbar spine surgery, which has been linked with ischemic optic neuropathy.
Systemic and ocular risks. “We found that systemic hypertension is by far the main modifiable vascular risk factor for this disease, which is consistent with the vascular hypothesis of NAION,” said lead author Dean M. Cestari, MD, assistant professor in the department of ophthalmology at Harvard Medical School. In addition, patients with blood-clotting abnormalities had a 146% increased hazard of a NAION diagnosis. Although previous studies have linked diabetes to NAION, this study showed an increased risk of NAION only in diabetic patients with end-organ involvement in comparison to well-controlled diabetics.
Ocular associations with NAION were seen only with age-related macular degeneration (AMD) and retinal vein occlusion (RVO). Patients with RVO were 4 times more likely to develop NAION than patients without RVO. “Given that CRVO can cause a swollen optic nerve head,” said Dr. Cestari, “we were initially concerned that this finding of an increased risk could have been due to a coding issue. But after controlling for this, it turned out not to be the case.”
Demographic factors. As expected, age was a risk factor: Each additional year was associated with a 2% increased risk of NAION. Less expected was a correlation between NAION and gender and ethnicity: NAION was more common in men than in women; however, both Latinos and Latinas were highly protected from the disease. This points to potential hormonal and genetic influences, said Dr. Cestari. “Preliminary data from more than 60 samples have revealed more genetic abnormalities than you would expect in this disease.” The researchers are following up with a genetic study of NAION patients around the country.
Clinical practice and collaboration. Although it’s premature to suggest treatment based on this study’s findings, said Dr. Cestari, understanding modifiable risk factors such as systemic hypertension may be especially helpful because there is approximately a 30% chance of developing NAION in the second eye within 5 years.
Dr. Cestari applauds the study’s collaboration between researchers in glaucoma and neuro-ophthalmology, who used big data to better understand disease risk factors. “These 2 fields have traditionally been considered separate, but as we learn more about diseases that affect the optic nerve, we see they actually have more in common than originally thought. Great research can come from this kind of collaboration.”
—Annie Stuart
___________________________
1 Cestari DM et al. Ophthalmology. 2016;123(12):2446-2455.
___________________________
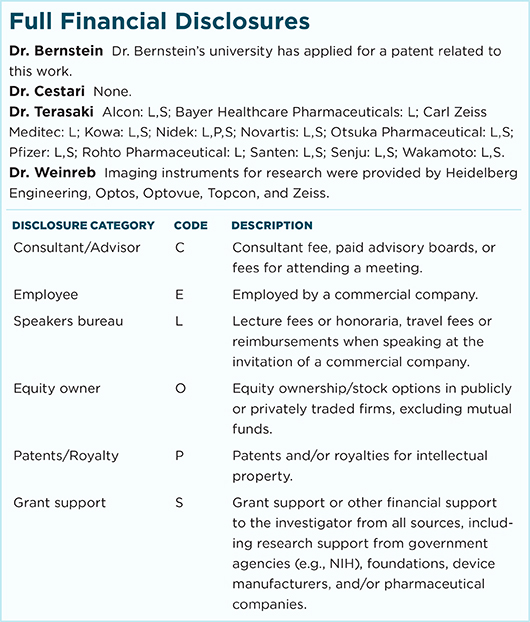
Relevant financial disclosures–Dr. Cestari: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review