Download PDF
Although definitive tests to diagnose Alzheimer disease (AD) in its earliest stages remain frustratingly elusive, recent developments in identifying retinal biomarkers—combined with new insights into the visual symptoms of the disease—are reenergizing the quest, shifting the spotlight from the brain to the eye.
A number of recently published studies report the efforts to identify potential biomarkers for early AD, including retinal ganglion cell layer (RGCL) and nerve fiber layer (RNFL) thickness and peripheral retinal deposits or pigmentary changes thought to contain accumulations of ß-amyloid protein. Other researchers are evaluating changes in eye movements. These and other efforts raise the tantalizing possibility of an eye test for AD.
Clinical Practice: On the Front Line
The clinical ophthalmology practice may represent the front line in identifying early AD, said neuro-ophthalmologist Eric R. Eggenberger, DO, who has had a longtime interest in the visual variant of AD.1
Older patients may present with difficulty reading or doing a task, and it often is challenging to pinpoint whether the underlying problem has to do with the patient’s vision or cognition. “In these patients, when all of the acuity, color, and perimetry tests appear overtly normal, the ophthalmologist should be prompted to think globally that something is going on in the brain,” said Dr. Eggenberger, at Michigan State University.
Conducting clinical research on this population is problematic, because many patients in the early stages of AD may experience difficulty taking eye tests, Dr. Eggenberger said. In his own practice, he tries to take a history while the spouse is in the room, as the patient may not be aware of any subtle visual changes. He also administers standard cognitive testing to help detect any early evidence of cognitive decline. This is followed up by visual exams, along with magnetic resonance imaging (MRI) and positron emission tomography (PET) scans.
Target: Imaging Biomarkers
Earlier this year, ophthalmologist Eleonora Lad, MD, PhD, captured the spotlight at the Alzheimer Disease International conference with her presentation on retinal imaging biomarkers for the early detection of the disease.2
This discovery opens the door to eye tests for AD—and such tests “have the potential to be superior to current diagnostic AD modalities,” said Dr. Lad, at Duke University. For instance, MRI and PET scans are costly, cerebrospinal fluid biomarkers require invasive tests, and genetic markers and serum amyloid provide suboptimal specificity and sensitivity.
Initially, Dr. Lad and her team of collaborators at Duke focused on the inflammatory injury that causes neurodegenerative disease in the brain. They postulated that patients with AD may experience a similar type of inflammatory injury in the retina that results in atrophy of the RGCL, manifesting during the prodromal stage of AD. They then investigated whether the RGCL or RNFL could serve as a noninvasive, inexpensive biomarker for AD. “The retina holds promise, as it is the only area of the body that provides access to noninvasive in vivo high-resolution images of central nervous system tissue,” she said.
Dr. Lad noted that her multidisciplinary team was determined to conduct a rigorous study. “This study is among the first of its kind to have 3 robustly characterized neurocognitive and age-matched groups; careful exclusion of AMD, glaucoma, and image artifacts; 1-year follow-up of cognition and retinal biomarkers; and spectral-domain optical coherence tomography [OCT] of the macula and optic nerve, widefield fundus color and autofluorescence photos, and stereo disc photography,” she said.
The researchers utilized an automated segmentation software program, the Duke OCT Retinal Analysis Program, to measure location-specific RNFL and RGCL thicknesses. Although the preliminary analysis did not reveal a reduction in RNFL or RGCL in a small sample of AD patients—a finding Dr. Lad attributes to “careful exclusion of normal-tension glaucoma”—some promising signals in RNFL/RGCL and peripheral drusen thought to be amyloid have been identified since the preliminary analysis.
Dr. Lad plans to expand her research to include patients at different stages of cognitive impairment. As an added note, she has found that the prevalence of AD appears to increase with the severity of AMD, supporting the hypothesis that these conditions are linked.
Target: Retinal ß-Amyloid
Researchers at Cedars-Sinai in Los Angeles have developed a noninvasive retinal imaging device designed to detect ß-amyloid protein, the primary material found in brain plaques characteristic of AD. The protein may be a “useful biomarker in patients with AD, since amyloid is one of the first pathological changes seen in the disease,” said neurosurgeon Keith L. Black, MD, at Cedars-Sinai. He added that the device is “designed for use in ophthalmologists’ offices, and we hope to have FDA approval in 2016.”
In a study published in 2011, Dr. Black and his team found that the ß-amyloid plaques associated with AD appeared not only in the postmortem brains from suspected and confirmed AD patients but also in postmortem retinas.3
More recently, the researchers found that ß-amyloid levels detected in the retina significantly correlated with ß-amyloid levels in the brain as detected by PET imaging. Although these preliminary findings involved just 40 patients, the study—which is being conducted in Australia as part of the Australian Imaging, Biomarkers, and Lifestyle Flagship Study of Aging—has now enrolled 200 patients.
Dr. Black emphasized the importance of detecting plaques in patients before they develop symptoms, “when they can possibly benefit from lifestyle interventions that improve cognitive function.” He pointed to a recent report showing that a comprehensive program of healthy eating, exercise, brain training, and management of metabolic and vascular risk factors appeared to slow down cognitive decline.4 “If we can not only detect these retinal changes early but also put patients on lifestyle intervention protocols, we may be able to prevent cognitive decline in those patients who are at risk for dementia,” he said.
Target: Eye Movement
The clinical, cognitive, and neurological implications of eye movement changes in AD, including alterations in saccades and smooth pursuit motion, may also hold promise as a method to help diagnose early AD.5
“I am not convinced that AD is a pure memory problem,” said neuropsychologist Brandon A. Ally, PhD, at Vanderbilt University. “Higher-level visual perception breaks down early in the disease and sometimes manifests itself as memory problems.” He cited cases in which a patient’s spouse says the problem appears to have more to do with vision than memory—for example, forgetting where a car is parked. “To the patient, all the cars may look the same, which may be attributed to visual perception issues.”
Dr. Ally and his team are investigating the role of the medial temporal lobe, particularly the issue of whether the perirhinal cortex is the intersection between visual perception and memory. Research has shown that the perirhinal cortex is one of the first areas of the brain affected by AD.
He noted that when comparing 2 objects, patients with early memory problems can identify target items. However, they are easily distracted by objects that share certain visual features, such as color and spatial frequency, and they have difficulty associating specific visual features of objects when making these comparisons. Dr. Ally’s lab has focused its work on better understanding the role of these visual features and the parietal cortex in memory retrieval. “If we can figure out how cognition problems and eye problems impact each other, we may be able to develop a whole new type of treatment to improve memory in these patients with AD,” he said.
___________________________
1 Eggenberger E. Ophthalmology. 2004;111(2):380-381.
2 Lad E et al. Abstract OC001 presented at: 30th International Conference of Alzheimer Disease International; April 16, 2015; Perth, Australia.
3 Koronyo-Hamaoui M et al. Neuroimage. 2011;54(suppl 1):S204-S217.
4 Ngandu T et al. Lancet. 2015;385(9984):2255-2263.
5 Molitor RJ et al. J Alzheimers Dis. 2015;44(1):1-12.
___________________________
Dr. Ally is assistant professor of neurology, psychiatry, and psychology at Vanderbilt University in Nashville, Tenn. Relevant financial disclosures: None.
Dr. Black is professor and chair of neurosurgery at Cedars-Sinai Medical Center in Los Angeles. He is also director of the Maxine Dunitz Neurosurgical Institute and the Johnnie L. Cochran Jr. Brain Tumor Center at Cedars-Sinai and chairman and founder of NeuroVision Imaging. Relevant financial disclosures: NeuroVision Imaging: O,P.
Dr. Eggenberger is professor and vice chair of neurology at Michigan State University in East Lansing. Relevant financial disclosures: None.
Dr. Lad is assistant professor of ophthalmology at Duke University in Durham, N.C. Relevant financial disclosures: None.
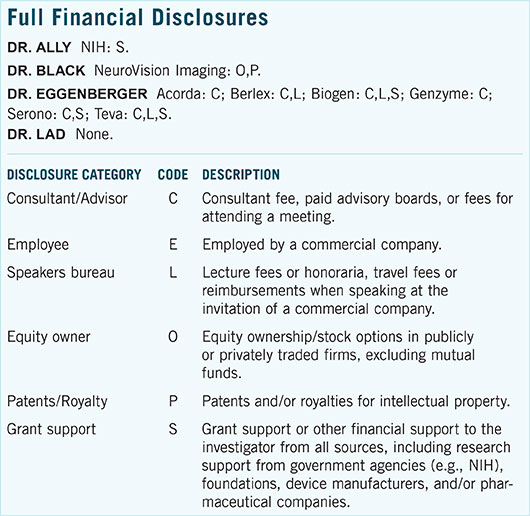
For full disclosures and the disclosure key, see below.