Download PDF
Although there are no epidemiological studies looking specifically at the prevalence of ocular allergy in the United States, several studies have determined that allergic disease overall is on the rise and that allergic conjunctivitis now affects at least 20 percent of the U.S. population (approximately 60 million Americans). About 35 percent of patients referred to an ophthalmologist’s office for red eye receive the diagnosis of allergic conjunctivitis, and about 95 percent of the cases of ocular allergy are seasonal or perennial in nature.1
The good news: More treatment options are available today than a decade ago, and many of the newer drugs require application only once a day, unlike the regimen of two or four times daily with the older agents.
Making the Diagnosis
Ocular allergy is usually a clinical diagnosis; in most cases, it is not hard to differentiate from other conditions. Even so, it can sometimes be challenging to make the diagnosis when other ocular surface diseases are also present. For example, it is not unusual for patients to have concomitant blepharitis or dry eye. As a result, patients with symptoms such as redness, itching, tearing, and burning should undergo an ophthalmic exam that includes examination of the lid margins and evaluation of tear breakup time. “Also, you need to be certain that the treatment you’re giving for one of these conditions is not worsening the others,” said Michael B. Raizman, MD, of Ophthalmic Consultants of Boston.
In some cases, it can be difficult to sort out the symptoms of the various conditions and determine the exact diagnosis and best therapy. Even so, if clinical symptoms and signs such as ocular irritation or redness are carefully elicited and observed, the diagnosis can still be made with a high degree of confidence, said Terrence P. O’Brien, MD, at the Bascom Palmer Eye Institute in Miami. If the clinical picture is not completely clear, point-of-care testing can sometimes help in making an accurate diagnosis. (See below, under “What About Skin Testing?”)
Importance of optimal therapy. Most patients with allergy have seasonal or perennial conjunctivitis, which almost never causes serious ocular abnormalities. “But vernal and atopic allergies are relatively rare and need to be treated aggressively by ophthalmologists, as scarring or even vision loss can occur,” said Dr. Raizman.
Treatment Trends
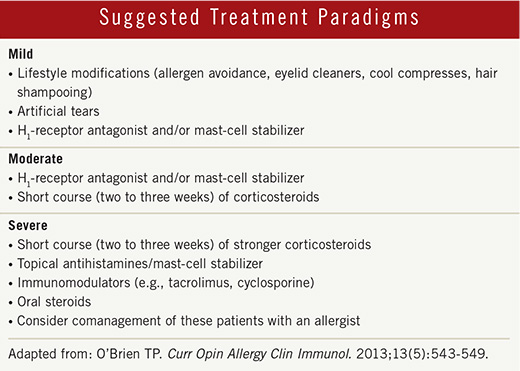
Dual-action drugs. In recent years, there has been an evolution toward using combination treatments for ocular allergy. For example, the front-line targeted medications for seasonal allergic conjunctivitis are dual-action topical antihistamines and mast-cell stabilizers. “Combination dual-action eyedrop therapy is not only convenient for the patient, but these medications also act rapidly to block the histamine receptor and help reduce symptom severity,” said Gregg J. Berdy, MD, at Ophthalmology Associates in St. Louis, Mo.
Fast-acting drugs. No matter what ophthalmic drug is chosen, the newer formulations tend to have a very fast onset of action (about three to five minutes), which can improve patient comfort and compliance. During allergy season, said Dr. Berdy, when patients wake up in the morning and before they go outside, they can instill a drop of a dual-action agent in their eyes, which will help prevent the symptoms of itching and redness.
|
Web Extra: Clinical Update
|
 |
Therapeutic Options
Preventive care. What about prophylactic treatment, especially for patients with a history of allergy? In many cases, the allergic response is already well under way by the time treatment is started, and the condition can hit like an explosive forest fire, said Dr. O’Brien. “Once the patient already has the redness, itching, and swelling of the allergy cascade, it is almost too late for mast-cell stabilization to have an immediate effect, although the topical antihistamine may help block the histamine receptors,” he added.
Nevertheless, in patients who are known to have the propensity for seasonal ocular allergy, medications may be prescribed in advance of the time when symptoms are most likely to erupt. Some patients prefer to start a couple of weeks before the onset of allergy season and then stay on the medication throughout the month (or months) in which they are usually affected. This strategy provides some protection and reduces the amount of allergic mediators that are released from conjunctival mast cells.
Widely prescribed. The current crop of ocular allergy drugs includes olopatadine 0.2 percent (Pataday), which is a dual-action drug. It was the first combined antihistamine/mast-cell stabilizer ophthalmic drug approved in the United States and is typically prescribed for once-a-day administration. Olopatadine 0.7 percent (Pazeo) is expected on the market soon.
Alcaftadine (Lastacaft) is a broad-spectrum antihistamine that is approved for the prevention of itching associated with allergic conjunctivitis. Yet another widely prescribed, topically administered drug for ophthalmic use is bepotastine (Bepreve). This potent dual-action drug can be administered twice a day and has shown efficacy in reducing allergy symptoms such as itching or watery eyes.
Other combination agents include epinastine eyedrops (Elestat) and azelastine (Astelin), which is administered as a nasal spray.
Considering corticosteroids. In cases where the allergy process is already well under way by the time patients seek treatment, newer and safer topical corticosteroids can help suppress some of the acute-phase (as well as the late-phase) reactions. This category includes loteprednol etabonate (Lotemax), which can be given in a lower concentration with a decreased likelihood of causing side effects, as it is a nonketone ester topical corticosteroid. If a clinician prescribes loteprednol along with one of the dual-action agents, the combination can bring symptoms under control rapidly and maintain comfort, said Dr. O’Brien. More potent corticosteroids can be reserved for intractable cases.
Oral immunotherapy. For patients who are sensitive to grass pollens, Oralair, the first approved sublingual allergen extract, made its debut on the market last spring. This medication, which is classified as an oral immunotherapy agent, is given in a once-daily tablet that dissolves under the tongue, and it can be started four months before the onset of grass pollen season. Patients typically take the first dose in the doctor’s office and are monitored for at least 30 minutes to make sure that no side effects occur. Thereafter, the drug can be taken at home.
In studies of about 2,500 patients in the United States and Europe, patients taking Oralair showed a 16 to 30 percent decline in allergy symptoms compared with those taking placebo.2
Nonpharmacologic strategies. Last but not least, clinicians should not ignore the nonpharmacologic therapies that can be used by patients with ocular allergy.3 For example, simple cool compresses are helpful for most patients. In addition, preservative-free chilled artificial tears can provide some symptomatic relief, and they can flush allergens (such as pollen) out of the eye. And simply shampooing one’s hair before going to sleep can reduce the allergen load on the pillow.
What About Skin Testing?
A relatively new skin test known as Doctor’s Allergy Formula is available for ophthalmologists to use in their offices. “Because allergy is so common, and screening panels may not be as helpful as you would like, options like in-office skin tests can be useful in some cases,” said Dr. O’Brien.
“A number of ophthalmologists are using this test, which is similar to the skin testing that has been available to allergists for decades,” said Dr. Raizman, who added that it can be administered by a technician or a nurse. With the test results in hand, the ophthalmologist may change or fine-tune the treatment approach for a particular patient. “Once the ophthalmologist confirms that the patient has an allergy—and not a condition such as dry eye, blepharitis, meibomian gland dysfunction, or a problem related to contact lens wear—then he or she can focus on a multimodal antiallergy therapy,” Dr. Berdy said.
In-office testing makes sense for patients who have chronic recurrent disease that has not followed a typical pattern of seasonal allergic conjunctivitis and has not responded well to therapy. “Allergists may balk at the thought of an ophthalmologist doing skin testing,” said Dr. Raizman, “but these are patients who, most of the time, are not going to see an allergist. By doing skin testing, you can encourage them to see an allergist.”
___________________________
1 Gomes PJ. Curr Opin Allerg Clin Immunol. 2014;14(5):451-456.
2 U.S. Food and Drug Administration. April 2, 2014. Accessed Nov. 20, 2014.
3 Bilkhu PS et al. Ophthalmology. 2014;121(1):72-78.
___________________________
Dr. Berdy practices at Ophthalmology Associates in St. Louis, Mo., and is assistant professor of clinical ophthalmology at Washington University School of Medicine. Financial disclosure: Has interests in Alcon, Allergan, and Bausch + Lomb.
Dr. O’Brien is professor of ophthalmology at Bascom Palmer Eye Institute in Miami. Financial disclosure: Has interests in Alcon, Allergan, and Bausch + Lomb.
Dr. Raizman practices at Ophthalmic Consultants of Boston and is director of the Cornea and Cataract Service at the New England Eye Center in Boston. Financial disclosure: Has interests in Alcon, Allergan, and Bausch + Lomb.