By Aileen Sy, MD, and Rona Z. Silkiss, MD, FACS
Edited by Steven J. Gedde, MD
Download PDF
For 5 years, Alice Evans,* a 34-year-old African-American woman, felt that her left upper eyelid was more swollen than her right. She didn’t think much about it until she noticed that her vision was becoming progressively blurry in her left eye, but it was only when she developed double vision with upgaze that she decided to seek medical attention. Her general ophthalmologist noted left orbital proptosis in addition to a swollen left upper eyelid and referred Ms. Evans to our clinic. An MRI had been scheduled but hadn’t yet been performed when she came to see us.
What We Saw
During our initial clinic visit, Ms. Evans denied any fatigue, weight loss or weight gain, or cold or heat intolerance. She also did not have any headaches or prior history of trauma. Past medical, ocular, surgical, and family history were all unremarkable.
Vision exam. Ms. Evans’ BCVA was 20/20 in the right eye and 20/40 in the left eye, with pinhole improvement to 20/25. She had normal pupillary response in both eyes without afferent pupillary defect, as well as normal ocular motility, confrontation visual field, and color vision bilaterally.
External exam. We noted moderate left upper eyelid swelling and orbital fullness, with a margin-reflex distance of 4 mm on the right and 3 mm on the left. On Hertel exophthalmometry, her left eye was noted to be mildly proptotic. The anterior segment exam was unremarkable. The undilated fundus exam appeared normal, with no optic disc edema in either eye.
What Tests Revealed
MRI revealed an enhancing mass surrounding the left optic nerve, extending to the orbital apex, compatible with thickening of the optic nerve sheath; the optic nerve itself appeared normal. Extraocular muscles, optic chiasm, and right orbital anatomy all appeared normal. Appearance of the mass was suggestive of optic nerve sheath meningioma (ONSM). Discovery of the mass on imaging prompted evaluation with Humphrey visual fields, which were within normal limits in both eyes.
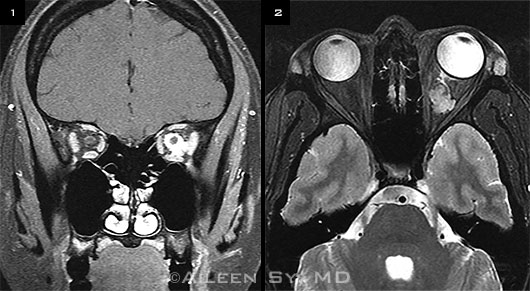 |
ON MRI. We noted an enhancing mass surrounding the left optic nerve. This extended to the orbital apex, but the optic nerve itself looked normal. (1) Coronal MRI T1 view. (2) Axial MRI T2 view.
|
About the Disease
Optic nerve sheath meningioma is an uncommon type of intraorbital tumor that is reported to represent 2% to 14% of orbital tumors.1-3 ONSM typically affects middle-aged women, causing a slowly progressive, painless vision loss. In most cases, ONSM is unilateral. Many patients do not present to a physician until several years after onset of visual symptoms, and diagnosis itself can often take several years.1-3
Often, ONSM represents an extension from an intracranial lesion; primary intraorbital ONSM is uncommon. Despite being a benign tumor, ONSM eventually progresses to cause complete vision loss in the affected eye. Association of ONSM with neurofibromatosis 2 has been reported.3
Patients generally present with good vision but on exam are found to have mild proptosis and optic nerve swelling or atrophy. Optociliary shunt vessels can also be seen. There is no specific visual field defect that is pathognomonic for ONSM; peripheral constriction, enlarged blind spot, and scotomata have all been reported.2,3 Decrease in color vision can also be seen.
Due to a high risk of visual morbidity, biopsies of ONSM are generally not performed; diagnoses are most often presumptive based on imaging. ONSM appears as a hyperintense thickened mass surrounding the optic nerve on T2-weighted MRI, enhancing with gadolinium. The optic nerve itself is typically neither enhancing nor enlarged.2,3 On coronal MRI cuts, the enhancing lesion around the optic nerve has been referred to as a “doughnut” sign, whereas on axial MRI imaging, the ONSM appears as a “tram-track” sign.2 ONSM is most commonly tubular in shape, as compared with the fusiform shape more commonly seen with optic gliomas. However, the lesion has also been reported to take globular and fusiform patterns.2
Treatment
While reports indicate variability in the rate of ONSM progression, the majority of tumors progress slowly. Visual prognosis is ultimately poor in these patients. Historically, management consisted of observation until invasion of the optic chiasm required surgical removal of the lesion to protect vision in the fellow eye. In the last 10 years, radiotherapy has become the recommended treatment for patients with progressive ONSM (as denoted by a decrease in visual acuity, constriction of visual fields, or enlargement of lesion).
In 2002, a study by Turbin et al. reported a large retrospective case series comparing ONSM patients receiving observation, surgery, radiation, or surgery plus radiation.4 The study found that all therapies except for radiation alone resulted in significantly worse visual acuities at follow-up (mean, 150.2 months; minimum, 50 months).4 Additionally, 44% of patients treated with radiation showed at least 2 lines of improvement in visual acuity.4
At the time of that study, side effects of radiation therapy included radiation retinopathy, optic neuropathy, cataract formation, dry eye, hearing loss, pituitary dysfunction, cranial nerve dysfunction, and brain atrophy.4 Since then, improvements in radiotherapy technique have allowed for improved success rates and reduction in complications, with more precision in delivering higher isodose levels to smaller volumes of tissue.
A recent review of all studies reporting on radiotherapy for ONSM confirmed good visual outcomes with successful tumor control.2 Additionally, the review identified a possible trend toward better efficacy with fewer side effects with stereotactic fractionated radiotherapy over conventional radiotherapy.2
Patient’s Progress
Ms. Evans underwent a repeat MRI 3 months after her initial presentation. It showed no significant change in the size of her lesion. On further review of older studies, it appeared this mass had been present on a CT scan that had been performed 4 years previously but it was not diagnosed at the time. Symptomatically, Ms. Evans continued to experience swelling of her left upper eyelid and diplopia, but her visual acuity was stable on follow-up. The option of radiotherapy was discussed with her, and she will continue under observation until any decrease in visual acuity or change on imaging is noted.
___________________________
* Patient’s name is fictitious.
___________________________
1 Dutton JJ. Surv Ophthalmol. 1992;37(3):167-183.
2 Shapey J et al. J Clin Neurosci. 2013;20(8):1045-1056.
3 Wilhelm H. Curr Opin Neuro. 2009;22(1):11-18.
4 Turbin RE et al. Ophthalmology. 2002;109(5):890-899; discussion 899-900.
___________________________
Dr. Sy is a resident and Dr. Silkiss is chief of ophthalmic plastic, reconstructive, and orbital surgery; both are at California Pacific Medical Center in San Francisco. Related financial disclosures: None.