By Mike Mott, Contributing Writer, interviewing Luis J. Haddock, MD, Andrew M. Hendrick, MD, Carolyn K. Pan, MD, and Michael Ullman, MD
Download PDF
Consider the many settings in which fundus photography may be needed: the emergency department, nursing homes, the clinic, remote settings, and more. Yet the current gold standard—the tabletop fundus camera—is bulky and expensive, depends on a trained technician, and requires that a patient be seated upright, a challenge for those who are immobile or hospitalized.
The evolution of the high-resolution smartphone camera offers the potential to revolutionize traditional fundus photography. By replacing a binocular indirect ophthalmoscope with a smartphone, many ophthalmologists are innovating a new field of funduscopy. Not only is the technique inexpensive and relatively easy to learn, but the expansion of mobile networks into all sectors of everyday life also is creating unique opportunities for telemedicine, resident training, and clinical care around the world.
What Is Smartphone Funduscopy?
“The main concept is to use the smartphone screen to perform the exam rather than a binocular indirect ophthalmoscope,” said Michael Ullman, MD, at Georgetown University/Washington Hospital Center in Washington, D.C. “You still need a 20- or 28-diopter lens in the other hand, but your smartphone serves as the ophthalmoscope, the coaxial light source, and the recording device.”
And it’s relatively simple to capture useful fundus images:
- Enable the device’s video mode.
- Set the flash to “on” for uninterrupted illumination.
- With the lens held in the other hand, start recording.
- Use the smartphone’s “pinch” zoom feature to focus as needed.
- Once the exam is complete, stop the recording.
- To obtain a still image from the sequence, replay the video and capture a screenshot at the desired time.
Practice, practice, practice. Don’t expect to get the best photos from your first attempt, said Carolyn K. Pan, MD, at Stanford Medicine in Palo Alto, California. “Don’t get discouraged. Like most procedures, it’s all about muscle memory. With practice, you’ll figure out the best distance from the retina and how to position the patient relative to your hands.”
 |
|
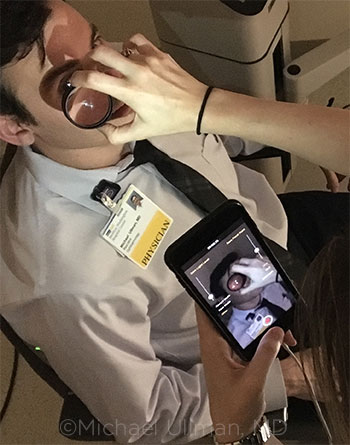
SMARTPHONE IN USE. A colleague performs smartphone funduscopy on Dr. Ullman.
|
Applications Across the Board
Who currently uses this technology and who should consider adopting it?
Residency. Smartphone funduscopy is quickly becoming common practice in residency programs as a learning tool. “It plays an essential role in training,” said Luis J. Haddock, MD, at the Bascom Palmer Eye Institute in Miami. “If a patient’s fundus finding is atypical or particularly interesting, for example, a smartphone provides an ideal educational opportunity for residents to share the case with other trainees and colleagues.” (See “Keep It Secure.”)
Residents are also using the technology as a teleconsultation tool, said Andrew M. Hendrick, MD, at Emory Eye Center in Atlanta. “A resident on call might see retinal whitening, for example, and might be unable to discern if it’s due to necrotizing retinitis or chorioretinitis. Having the ability to share the image and communicate with a specialist via a smartphone is why this new technology is a major boon for training,” he said.
Because young ophthalmologists have grown up around smartphones, they are taking to this technique rather quickly, said Dr. Hendrick. Recent studies have shown that medical students and residents inexperienced with traditional indirect ophthalmoscopy can learn smartphone funduscopy after just brief training.1,2
Telemedicine. The ease of use, portability, and availability of smartphones also presents a unique opportunity for telemedicine. “Today’s expansive mobile networks make this technique ideal for community settings and isolated rural areas with poor resources,” said Dr. Haddock.
Although the smartphone does not typically produce images that are as sharp as traditional cameras, he said, researchers have found that they are of sufficient quality for glaucoma and diabetic retinopathy screening.3,4 “Many medical mission and humanitarian organizations—at home and abroad—are already using smartphone funduscopy in the field as a way to screen for eye disease by sending out images for remote consultation to determine which patients need to be referred for the proper care.”
In the clinic. While it’s uncommon for ophthalmic clinics or private practices with traditional desktop cameras to employ smartphone funduscopy, that might change in the near future, said Dr. Haddock. For ophthalmologists considering adding smartphone funduscopy to their repertoire, he recommends identifying needs and determining if it fits into current workflows.
“This technology isn’t for everyone,” he said, “but there are many different reasons why an ophthalmologist might want to embrace it.” Some might want to enhance their ability to document and track clinical findings quickly and easily. Others might want to fill a gap in their practice to avoid using their staff photographer for imaging lower priority cases. Others might simply love the latest gadgets and want to embrace early adoption of new technologies.
“Regardless of the different motivations,” said Dr. Pan, “as interest in smartphone funduscopy continues to grow, ophthalmologists will become increasingly excited about it—and this will foster more development and further expansion into practice settings.”
 |
|
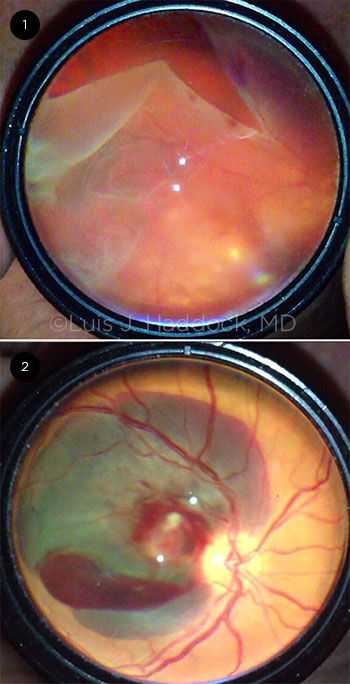
FUNDUS IMAGES. (1) Giant retinal tear and (2) retinal macroaneurysm images taken via smartphone funduscopy.
|
Benefits—But With Caveats
The advantages of smartphone funduscopy are numerous. Smartphones are portable and inexpensive, come equipped with a safe light source,5 and provide ready access to secure networks for data transmission—plus, they are everywhere. “This type of imaging is compelling simply because of the instrument’s ubiquity,” said Dr. Hendrick. “If you’re examining a young child or an immobile patient who’s unable to be positioned for conventional funduscopy, it’s nice to know you have a high-quality camera in your back pocket.”
But, it isn’t without limitations.
Field of view. “Compared with traditional tabletop devices, smartphone cameras don’t have the ability to access the full retina, and so your peripheral view is significantly smaller,” said Dr. Hendrick. Good dilation is also a necessity. But even then, the camera flash can induce a high frequency of optical artifacts—especially if the media is too dense.
Image quality. “Unfortunately, you are also sacrificing a lot in terms of image quality when using smartphone funduscopy,” said Dr. Ullman. “Because of the technology involved, the resolution is nowhere near that of a professional desktop camera.” Glare and improper exposure are the major culprits, but capturing a screenshot of the video sequence can further degrade image quality.
Learning curve. Similar to the conventional method of indirect ophthalmoscopy, the smartphone technique involves many moving parts—physician, camera, lens, patient—so the learning curve can be steep, said Dr. Hendrick. “One of the most important questions to ask when considering whether to adopt smartphone funduscopy is ‘Who will perform the imaging?’ There’s a fairly sophisticated skill set that needs to be cultivated, so unless you have someone already adept at indirect ophthalmoscopy or someone who takes quickly to smartphones in general, it can be challenging to obtain high-quality images that are useful for a comprehensive ophthalmologist or retina specialist.”
Smartphone Funduscopy 2.0
To overcome some of these limitations, innovators are developing new approaches and pushing the limits of the smartphone.
Apps. Many developers are introducing apps unique to funduscopy for streamlining the exam process. “The native smartphone settings simply aren’t designed for this type of work,” said Dr. Ullman, creator of the Ullman Indirect app. “But a new wave of downloadable software is allowing for independent manipulation of the camera.”
With the Ullman Indirect app, for example, users can control the camera’s functionality as follows:
- Manually focus the camera and save focal points for various condensing lenses
- Manually control the exposure of the camera to reduce glare
- Control the light level of the flashlight similar to a rheostat
- Rotate images and video to document findings in the correct orientation
- Export high-quality still images without the need to screenshot a video
3D-printed adapters. Ophthalmologists are also taking advantage of the 3D-printing revolution to expand the power of their mobile devices. Using free, open-source designs, you can print hardware adapters that attach the condensing lens to the smartphone at a prescribed—but adjustable—distance from the camera.6
“With this method, you are reducing the number of moving parts necessary to conduct the exam,” said Dr. Pan. “These adapters take a lot of the guesswork out of estimating distances and make it much easier to achieve reproducible, high-quality images; they also free up your second hand.”
All-in-one devices. Regardless of whether you use the apps or adapters mentioned above in conjunction with your smartphone, they are not FDA approved for funduscopy. As a result, the smartphone exam is designated for educational purposes only and is not billable as a service. However, several imaging companies, like Remidio, D-Eye, and Volk, are changing that.
Digital ophthalmoscopes are standalone, handheld devices that connect your smartphone to a specifically designed professional funduscope. Although this technology is still in its infancy, a growing number of these “point-and-shoot” fundus cameras include:
- Built-in data encryption for collecting patient data
- HIPAA-compliant storage and export capabilities
- Infrared lighting for nonmydriatic viewing
- A view of the peripheral retinal approaching 80 degrees
- Proprietary apps for independent camera control, autofocus, and autocapture
- FDA approval for billing purposes
“These devices are still using smartphone technology and so they do suffer from some of the limitations mentioned earlier,” said Dr. Pan. “But the benefit is that these all-in-one cameras do everything for you, sensing exactly what you are trying to image and making the necessary adjustments. Whether it be light, focus, exposure, or image stabilization, there’s really not much to troubleshoot. You’re basically on autopilot.”
Although these cameras are significantly more expensive than a smartphone, they are also cheaper than a table fundus camera. And according to a recent report, these point-and-shoot devices offer a high sensitivity and specificity for detecting retinal disease compared with traditional systems.7
Keep It Secure
When a mobile device is used to receive, send, access, or store a patient’s protected health information, it must strictly adhere to HIPAA guidelines. For smartphone funduscopy, compliance typically involves limiting access to the device and securely storing and sharing your images.
Access. At a minimum, you should password-protect your smartphone, avoid automatic logins for apps, and use an additional access key such as a fingerprint. You’ll also want to set the smartphone to log out or lock automatically if left idle. And if the device is ever lost or stolen, make sure you have the capability to “wipe” the smartphone remotely.
Storing and sharing. “Most native email or text applications don’t meet HIPAA requirements,” said Dr. Hendrick. “So you can’t simply take a patient photo, keep it on your phone, and send it to your colleagues thinking it’s secure.”
When storing any patient photographs, you’ll need a secure cloud-based server to restrict access from unauthorized individuals. When sharing, use an email account and text service with message encryption as well as an additional login to ensure that no one can intercept the transmission.
“In the end, consult with your IT department to make sure you are following all the necessary rules and regulations,” said Dr. Ullman. “And don’t forget to obtain the proper patient consent documentation.”
What’s Next
It remains to be seen whether smartphones will take the place of traditional desktop machines or the ultra-widefield capabilities of scanning laser ophthalmoscopy.
However, given the ongoing evolution in mobile operating systems and devices, this type of funduscopy will likely grow to be an important adjunct to traditional binocular indirect ophthalmoscopy, said Dr. Ullman.
Smartphones might also carve out entirely new niches in imaging. Augmented reality in combination with mobile technology could lead to an entirely new funduscopy experience, he said, in which examiners are prompted with heads-up displays about subtle pathology that can be automatically identified and graded in real time. “Smartphone funduscopy really is more than a passing fad or niche. It has an exciting future.”
___________________________
1 Adam MK et al. Invest Ophthalmol Vis Sci. 2014;55:1608.
2 Haddock LJ et al. J Ophthalmol. 2013;2013:518479. doi:101155/2013/518479.
3 Giardini ME et al. Conf Proc IEEE Eng Med Biol Soc. 2014:2177-2180.
4 Russo A et al. Am J Ophthalmol. 2015;159(2):360-364.
5 Kim DY et al. Ophthalmology. 2012;119(10):2200-2201.
6 Myung D et al. J Mob Technol Med. 2014;3(1):9-15.
7 Rajalakshmi R. et al. PloS One. 2015;10(9):e0138285. doi:10.1371/journal.pone.0138285.
___________________________
Dr. Haddock is an assistant professor of clinical ophthalmology at the Bascom Palmer Eye Institute in Miami. Relevant financial disclosures: None.
Dr. Hendrick is an assistant professor of ophthalmology at Emory Eye Center in Atlanta. Relevant financial disclosures: None.
Dr. Pan is a clinical assistant professor of ophthalmology at Stanford Medicine in Palo Alto, Calif. Relevant financial disclosures: None.
Dr. Ullman is a second-year ophthalmology resident at Georgetown University/Washington Hospital Center in Washington, D.C. Relevant financial disclosures: Prevention of Blindness Society of Metropolitan Washington: S; Ullman Indirect: O.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Haddock Genentech: C; Notal Vision: C.
Dr. Hendrick Clearside: C; National Eye Institute: S.
Dr. Pan None.
Dr. Ullman Prevention of Blindness Society of Metropolitan Washington: S; Ullman Indirect: O.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|