Subretinal Air and tPA for Submacular Hemorrhage: First U.S. Results
By Jean Shaw
Selected By: Andrew P. Schachat, MD
Journal Highlights
Ophthalmology Retina, March 2018
Download PDF
At present, there is no consensus on the optimal management of submacular hemorrhage (SMH), which is a rare but potentially devastating complication of choroidal neovascularization. Sharma and Kumar et al. set out to determine whether massive SMHs can be managed with subretinal injections of tPA (tissue plasminogen activator) and air. They found that the combination was successful, resulting in consistent displacement of SMH out of the fovea as well as improved visual acuity (VA) and retinal thickness.
This retrospective interventional case series included 24 patients with SMH from 5 sites in the United States. The patients’ mean age was 79.1 years (range, 62-92 years). The underlying cause of SMH was polypoidal choroidal vasculopathy (n = 4) and age-related macular degeneration (n = 20). In addition, 13 (54%) of the patients were on anticoagulation therapy for stroke prevention (n = 9), stroke history (n = 3), or atrial fibrillation (n = 1). Main outcome measures included frequency and extent of SMH displacement and postoperative VA, retinal thickness, and complications.
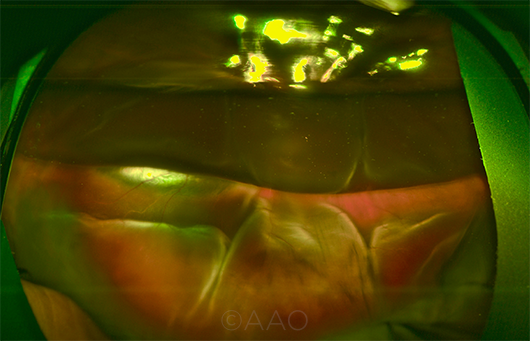 |
DISPLACED HEMORRHAGE. This wide-field image taken on postop day 1 shows an inferiorly displaced SMH, with partial gas fill in the vitreous cavity to prevent the subretinal air from migrating superiorly.
|
Based on image review, SMH was considered subretinal in 5 patients, sub-RPE (retinal pigment epithelium) in 2, and both subretinal and sub-RPE in 17. Hemorrhage size was small (does not reach arcades) in 6 patients, large (extending to the arcades) in 2, extensive (extending past the arcades) in 9, and massive (extending to 2 quadrants and/or past the equator) in 7. With regard to retinal thickness, the hemorrhages were < 500 μm in 7 patients and > 500 μm in 17.
All patients underwent pars plana vitrectomy (with induction of a posterior vitreous detachment, if necessary), followed by subretinal injection of tPA and filtered air. Most (n = 23) of the patients also received bevacizumab as part of the surgery or treatment. They were then followed for an average of 12.5 months (range, 3-28 months).
At 3 months postoperatively, there was complete displacement of SMH in all eyes. Although 13 eyes experienced no complications, 5 had a recurrent subretinal SMH that was successfully displaced with the same treatment. The remaining 6 eyes had a nonclearing vitreous hemorrhage (n = 3), retinal detachments (n = 2), or macular hole (n = 1). Mean retinal thickness improved from 463.7 μm preoperatively to 311.3 μm postoperatively, and VA improved in 23 eyes and remained stable in 1.
The original article can be found here.