By Reena Mukamal, Contributing Writer, interviewing Melissa Barnett, OD, Lauren S. Blieden, MD, Michele C. Lim, MD, and Francis K. Manuel, OD
Download PDF
Advanced glaucoma patients who are contact lens–dependent have long posed a challenge for both ophthalmologists and contact lens specialists. This is because bleb-producing trabeculectomy or tube shunt surgery may become necessary. As the point of friction between the bleb and contact lens can lead to breakdown of the tissue and cause infection, lens wear is generally contraindicated. Traditionally, patients with blebs must permanently transition to glasses or choose an alternative procedure, which may leave them drop-dependent.
However, new impression-based scleral lens technology and minimally invasive glaucoma surgery (MIGS) devices may give glaucoma specialists more tools in their arsenal to help advanced glaucoma patients who need contact lenses.
Blebs and Contact Lenses
A small but growing number of glaucoma patients wear contact lenses, said Michele C. Lim, MD, at the University of California Davis Eye Center in Sacramento. “When older style rigid lenses were the only option, most patients chose glasses. But with the advent of more comfortable soft, hybrid, and custom-fitted scleral lenses, we’re seeing a shift.” And for certain patients, contacts aren’t just a preference, they’re a necessity.
When patients need contacts. While some people can make the switch to glasses, others either are severely hyperopic, myopic, or have corneal disease that makes them reliant upon contact lenses for best vision.
“I take care of a lot of high acuity corneal patients. Some have keratoconus, Fuchs dystrophy, or corneal scarring from infection or injury. Others have had corneal transplants, and only contact lenses can smooth out the irregular corneal surface and help reestablish clear vision,” said Lauren S. Blieden, MD, at the Cullen Eye Institute, Baylor College of Medicine in Houston. When these patients are faced with advanced glaucoma surgery, ophthalmologists generally steer them away from bleb-producing operations, she said.
The problem with lenses and blebs. “To date, advanced glaucoma patients who require contacts have generally been poor candidates for trabeculectomy or tube shunts because incisional surgery increases the risk of eye infection, and a contact lens can act like your kitchen sponge—a depot for bacteria to absorb and sit on the surface of the eye,” said Dr. Blieden.
Every type of contact lens introduces unique challenges when it meets a bleb, according to Melissa Barnett, OD, a scleral lens specialist who works with Dr. Lim at the University of California, Davis Eye Center.
- Conventional soft contact lenses may not adequately cover the ocular surface, including the bleb. If the edge of the lens overlaps the bleb, blink-activated friction could slowly erode or thin the epithelial tissue causing leakage, breakdown, or infection, explained Dr. Lim.
- A corneal gas-permeable contact lens can cause mechanical insult to the bleb if it rides high. This can be magnified by spontaneous dislodgement, a common issue with these lenses, Dr. Barnett said.
- Standard scleral lenses—large diameter rigid gas-permeable (RGP) lenses—may compress a bleb, reducing its functionality, explained Dr. Barnett.
Unpredictable bleb morphology. To complicate matters, one can’t predict how a bleb will form after surgery, how long it will take to heal, or whether it will transform over time. “An ideal bleb is low profile and has minimal vascularity,” said Dr. Lim. Additionally, when the bleb forms more posteriorly to the limbus, it is farther away from the edge of a contact lens. “But you can do the same surgery on 10 different people and end up with 10 different blebs. Blebs can continue to remodel for years,” she explained. That’s because a bleb is “a living, breathing entity, subject to change at any time,” said Francis K. Manuel, OD, the contact lens specialist who works with Dr. Blieden at Baylor.
 |
|
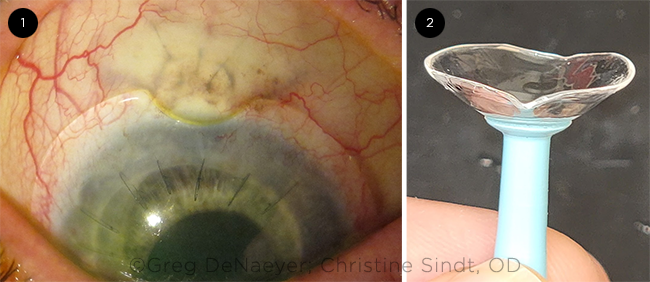
LENSES FOR BLEBS. (1) A photo of a scleral lens with a notch bypassing a conjunctival bleb. (2) An EyePrintPRO lens.
|
Expanding the Toolkit
Customized scleral lenses. Contact lens technology is changing, with advances in lens materials, designs, imaging, and manufacturing techniques. This has fueled the innovation of customizable scleral lenses, flexible enough to fit a highly irregular eye, said Dr. Barnett. A notch, elevation, or impression mold can be incorporated into a scleral lens to avoid a glaucoma drainage device (Fig. 1). One such product is the EyePrintPRO (EyePrint Prosthetics), a large-diameter scleral lens, which is designed using a mold of the patient’s ocular surface, she said. The mold is taken by a contact lens specialist, then scanned using millions of data points to create a 3D model. Dr. Barnett noted that every point on an EyePrint PRO lens is modifiable so that extra clearance may be created over the bleb to allow for micro changes of the bleb and so that the lens will not compress the conjunctival/scleral tissue over a tube. The lab transforms that model into a scleral lens that meets the physical shape and physiologic needs of the eye, said Dr. Manuel. “The accuracy of the EyePrintPRO is within a 6-to 7-μm range of matching the ocular surface anatomy. The lens edge can even make a 90 degree turn up and over a bleb [Fig. 2],” he said.
The EyePrintPRO was FDA-approved in 2016 and has become more widely available over the last couple of years, said Dr. Manuel.
There are no prospective, randomized, multiyear studies that assess the effect of scleral lenses on patients with glaucoma. “A highly debated topic is whether intraocular pressure is affected by scleral lens wear,” said Dr. Barnett. Nonetheless, glaucoma surgeons see potential. “Impression-based scleral lenses are providing a new frontier,” said Dr. Lim.
Xen and Preserflo. Two MIGS devices—the Xen Gel Stent (Allergan) and the Preserflo Microshunt (Santen)—come close to achieving the drainage success of a trabeculectomy, said Dr. Blieden. She added that both devices are less invasive than a traditional tube shunt, allowing for faster recovery.
The Xen, which was FDA approved in 2016, bypasses the diseased trabecular meshwork to drain aqueous from the anterior chamber to a subconjunctival bleb. Whereas a trabeculectomy creates a hole in the sclera with a variable flap, the Xen uses a 6 mm–long shunt to create a 45-μm lumen outflow. Similarly, the Preserflo MicroShunt, approved in Australia, Canada, and Europe, but not yet FDA approved, is an 8.5 mm–long shunt with a 75-μm lumen outflow, said Dr. Blieden.
Compared with trabeculectomy, both devices are designed to drain fluid farther away from the limbus (2 to 3 mm posterior for the Xen and 7 mm posterior for the Preserflo). “The greater the distance between the bleb and the limbus, the easier it is for the patient to wear a contact lens,” said Dr. Lim.
There is much discussion among glaucoma surgeons about the blebs that these devices create. Some say they are more low lying, low profile, and diffuse than trabeculectomy blebs, said Dr. Lim. In Dr Blieden’s experience, “Sometimes Xen blebs form more posteriorly, but not consistently. Preserflo blebs tend to be flatter and more posterior to the limbus, making them more amenable to contact lens wear. But we’re still a way off from knowing what they will do in the long-term.”
Surgical Considerations
Preoperative expectation setting. Before surgery, it is important to have a practical discussion with the patient about their preferences for contact lens wear. “I caution my patients who are traditional soft contact or RGP lens wearers that there is a decent chance they may not be able to be fit with that type of lens again. If appropriate, I educate them about the EyePrintPRO lens and its cost,” said Dr. Blieden.
Trab or tube? For keratoconus patients or those who are truly lens-dependent for any other reason, she will also discuss the pros and cons of tube shunt and trabeculectomy procedures. This is because a tube shunt results in a more predictable limbal anatomy, better for contact lens wear. Its success rate is comparable to a trabeculectomy, although patients are more likely to require drops.1 Dr. Lim agreed that a tube surgery gives patients a greater potential to wear contact lenses.
Ocular surface disease. Close communication with both the surgeon and patient preoperatively can be valuable for the contact lens specialist. “An evaluation before surgery allows me to assess anatomy and acuity potential and look for the presence of ocular surface disease [OSD],” said Dr. Manuel. Dr. Barnett added, “It’s essential to optimize the ocular surface preoperatively for the best outcomes. Many patients with glaucoma have corneal irregularities. In addition, they are more likely to have OSD from long-term use of topical glaucoma medications. Multiple strategies can be used to manage their OSD, including eyelid hygiene, commercial eyelid cleaners, warm compresses, preservative-free eyedrops, topical immunomodulators, punctal plugs, and lifestyle changes.”
Trabeculectomy incision. Evidence suggests that while the type of surgical incision—fornix-based versus limbus-based—doesn’t have a measurable impact on the success rate of a trabeculectomy, it can affect the bleb formation. Compared with a limbus-based incision, a fornix-based incision may help create a lower, more diffuse bleb.2 “A fornix-based incision makes a more diffuse bleb because the posterior aspect of the bleb is not limited by the scar tissue that forms for the closure of a limbus-based bleb,” explained Dr. Blieden.
Mitomycin-C treatment. The method of mitomycin-C (MMC) application may also influence bleb construction. Blebs tend to be more diffuse and less vascularized when MMC is delivered via an injection rather than a soaked sponge.3 Dr. Blieden said she has switched to the injection method for her fornix-based trabeculectomies.
Postoperative healing. Complete healing of the ocular surface and stability of IOP are essential before contact lens fitting. Complications such as hypotony, erosion, bleb leakage or failure, infection, and corneal hypoxia need to be addressed and resolved. With this in mind, Dr. Blieden won’t recommend a patient for fitting for at least two months postoperatively, and Dr. Lim tells her trabeculectomy patients to wait about six months after surgery. This wait can be frustrating for lens-dependent patients, said Dr. Manuel. Indeed, “some patients are functionally on ‘stop’ until we can get contact lenses back on them,” he said.
Scleral lens fitting. Dr. Manuel often fits advanced glaucoma patients with EyePrintPRO lenses. He said that the impression molding process is gentle and takes a few minutes, and once the mold is sent to the lab, lenses are generated in two to three weeks.
It can take time for patients to get accustomed to putting on a scleral lens. “Getting the eyelids out of the way is the biggest challenge,” said Dr. Manuel. He noted that multiple tools are available to help with scleral lens application, such as a ring that is worn on the finger or a special applicator device with a guiding light.
Follow-up and collaboration. After being fitted for lenses, patients need regular follow-up with both their surgeon and lens specialist. “I’ll see them once a month after the initial fitting, then at three-to four-month intervals. At each visit, I do a fit analysis to prevent impingement of the lens on the bleb,” said Dr. Manuel. He uses a combination of anterior segment OCT scans and slit-lamp imaging to take cross-sectional pictures of the eye and lens. He targets 200-250 μm of clearance over the cornea and also checks for whiteness or blanching of tissue beneath the lens edge, and he relays what he sees at each visit to the surgeon.
Dr. Blieden makes sure contact lenses “are not fitting too tight across a tube shunt, compressing the bleb, or too loose and bumping into things they shouldn’t be.”
If the patient is on drops or topical medication, Dr. Barnett carefully monitors and manages OSD. Blebs in complex eyes are likely to keep transforming and may need contact lens refitting. “One of my EyePrintPRO patients with severe dry eye and an already large bleb just had a spontaneous bleb enlargement, requiring revision of the impression-based lens. But with careful monitoring and collaboration, glaucoma patients with blebs can succeed with scleral lenses,” she said.
___________________________
MORE ONLINE. For an article on Xen and Preserflo, see the July 2021 EyeNet.
___________________________
1 Gedde S et al. Ophthalmology. 2020;127(3):333-345.
2 Solus JF et al. Ophthalmology. 2012;119(4):703-711.
3 Esfandiari H et al. Ophthalmol Glaucoma. 2018;1(1):66-74.
___________________________
Dr. Barnett is a principal optometrist specializing in ocular surface disease and specialty contact lenses at the University of California, Davis Eye Center in Sacramento. Relevant financial disclosures: None.
Dr. Blieden is associate professor of ophthalmology, Baylor College of Medicine in Houston. Relevant financial disclosures: Allergan: C.
Dr. Lim is professor, vice chair, and medical director, University of California, Davis Department of Ophthalmology & Vision Sciences, Sacramento. Relevant financial disclosures: Santen: C.
Dr. Manuel is an optometrist specializing in glaucoma and ocular therapeutics and a faculty member at Baylor College of Medicine, Houston. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Barnett None.
Dr. Blieden Allergan: C.
Dr. Lim Santen: C.
Dr. Manuel None.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|