By Tanvi Gaonker, MS, Alka Yadav, MS, Anju Rastogi, MS, and Pooja Bansal, MS
Edited by Bennie H. Jeng, MD
Download PDF
Necrotizing scleritis is a severe inflammation of the sclera with an aggressive and rapid course that can lead to blindness if it’s not adequately treated. It is commonly associated with collagen vascular disorders and other autoimmune diseases. When seen following any uneventful ocular surgery, at or adjacent to the surgical site, it is termed surgically induced necrotizing scleritis (SINS; Figs. 1 and 2). The clinical diagnosis is made when the scleritis is associated with vascular hypoperfusion (ischemia) or nonperfusion and after an infective etiology is ruled out; active inflammation may or may not be present.1 SINS should be distinguished from postoperative infectious scleritis.
SINS can occur following a variety of anterior and posterior segment ocular procedures, and its onset may range from a few days to many years after surgery.1 Histologic findings show inflammatory scleral granulomas with fibrinoid necrosis.2
Risk Factors
SINS has been reported after various ocular surgeries, including the following.
Pterygium excision. The surgery most commonly implicated in SINS is pterygium excision (accounting for 63.4% of cases in one series),3 most likely resulting from the use of adjunctive therapies to prevent recurrence, such as irradiation or mitomycin C (MMC), especially when it is applied for longer duration and at higher concentration. These adjunctive therapies can cause prolonged inhibition of wound healing, predisposing to necrosis. Excessive cauterization during bare sclera technique is another possible trigger.
Cataract surgery. Cataract surgery is the second most common type of surgery associated with SINS (17.5% of cases in one series).3 The incidence is higher for limbal incisions than for clear corneal incisions because the limbal approach causes greater vascular disruption. Excessive cautery to the sclera can be another cause.
Retinal detachment surgeries. SINS following vitreoretinal surgeries is relatively rare compared with anterior segment surgeries.4 However, excessive energy used in diathermy or in cryotherapy, polyglactin sutures used in conventional vitreoretinal procedures, or recurrent retinal detachment repairs can precipitate SINS at the site of sclerostomy.5 In scleral buckling surgery, the buckle can cause local ischemia due to disruption of episcleral vasculature.
Trabeculectomy. Indiscriminate use of cautery and antimetabolites such as MMC and 5-fluorouracil (for example, inadequate washout after removal of MMC-soaked sponges or a retained MMC sponge) during a trabeculectomy increases the risk. The biodegradable Collagen Matrix implant (Ologen) can theoretically cause excessive inflammation owing to its porcine origin.6
Strabismus surgery. Because it disrupts the episcleral vasculature, potentially leading to local ischemia, strabismus surgery can cause SINS.
Other surgeries. Other procedures reported as risk factors for SINS include diode laser transscleral photocoagulation, excision of conjunctival tumors, treatment of ocular surface squamous neoplasia with MMC, and placement of a ganciclovir implant.
 |
|
CLINICAL CASE 1. SINS in a 56-year-old man with rheumatoid arthritis, six months after small-incision cataract surgery. Signs include scleral thinning with uveal show at the site of the scleral tunnel. Systemic steroids were initiated, and complete resolution of inflammation was noted at the end of three weeks.
|
Etiology
An eye that has undergone multiple operative procedures has a significantly higher risk of developing SINS. The condition may be a clinical expression of an underlying systemic autoimmune disease: Overall, 63% of patients with SINS have an associated autoimmune disorder, with rheumatoid arthritis and granulomatosis with polyangiitis being the most common.3 Diabetes mellitus, thyroid disorders, herpes zoster ophthalmicus, and hyperuricemia are some of the other systemic diseases associated with SINS.
However, in some procedures, especially pterygium excision, underlying systemic disease is rare. In one series, only a few cases of scleral necrosis after pterygium excision were attributed to SINS, while the majority were due to postoperative infection, most commonly with Pseudomonas aeruginosa.3
 |
|
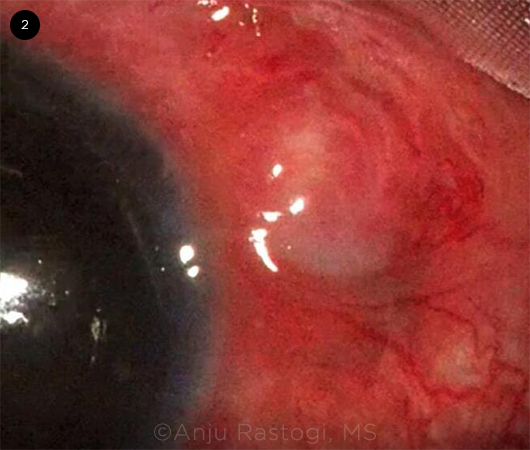
CLINICAL CASE 2. Necrotizing scleritis following four-point transscleral fixation of a posterior chamber IOL with 8-0 polytetrafluoroethylene in a patient with aniridia and lens subluxation. Signs include localized granuloma and scleral thinning with uveal show at the sclerostomy site. Patient received a course of oral steroids followed by a scleral patch graft at the site of thinning.
|
Pathophysiology
Several underlying mechanisms are responsible for scleral inflammation and necrosis after ocular surgery.
Immunologic mechanism. In predisposed patients, an immune complex–mediated vasculitis is triggered by the surgical trauma (which causes an antigen to be revealed or altered), resulting in accumulation of circulating immune complexes in the episcleral vessels at the surgical site. This subsequently incites an inflammatory process leading to scleral destruction and melting.
The rapid response of SINS to treatment with immunosuppressive agents supports this immunologic mechanism in its pathogenesis.
Surgical inciting factors. In addition, the following factors incite or exacerbate the necrotic process.
Ischemia. Local ischemia can be induced by strabismus surgery, particularly in multiple muscle surgeries, and scleral buckling procedures (overly tight buckles with multiple sutures) and excessive use of cautery.
Trauma. Intraoperative trauma due to excessive manipulation and epithelial damage can stimulate enzymatic destruction of scleral collagen.
Adjuncts. Liberal use of adjunctive treatment options such as MMC and irradiation can cause a breakdown of the epithelial barrier and weaken host defenses, making it susceptible to infections. This possibly explains the high incidence of infectious scleral necrosis following pterygium surgery.
Key Points: Surgically Induced Necrotizing Scleritis
- Characterized by sterile scleral inflammation at surgical site.
- Seen most frequently in eyes that have undergone multiple surgeries.
- Occurs most commonly after pterygium excision or cataract surgery.
- Associated with systemic autoimmune diseases.
- Must be differentiated from infectious causes of scleritis.
- Managed by prompt initiation of immunosuppressive therapy.
|
Diagnosis
Diagnosis is based on the patient’s history, symptoms, and clinical appearance, as well as laboratory and radiology investigations as appropriate.
History. The majority of patients with SINS have a history of two or more surgical procedures on the affected eye. The onset of inflammation is usually about three weeks after surgery but can vary from postoperative day 1 to 40 years later.1
Patients give a specific history of severe, deep, boring pain occurring over several days that awakens them from sleep and is worsened by eye movement.
Clinical features. The inflammation is typically noticed at or around the surgical wound or area of tissue excision. The eye is red, with a deep violaceous hue, while the affected area appears porcelain white. Eventually, a bluish hue is seen—the result of progressive thinning of the affected sclera with subsequent uveal show. The cornea may also be affected, especially following cataract or pterygium surgery.
Mucopurulence or scleral abscess is suggestive of infection, even in culture-negative cases.3 Hypopyon, if present, has a lesser diagnostic value for infection, as it can result from sterile inflammation as well.
Laboratory tests. The hematologic and immunologic workup for autoimmune diseases includes complete blood count, erythrocyte sedimentation rate, C-reactive protein, liver and kidney function tests, serum complement levels, antinuclear antibody, rheumatoid factor, antineutrophil cytoplasmic antibody, anti–citrullinated protein antibody, and serum angiotensin-converting enzyme levels. These investigations are particularly advised for patients who develop scleral necrosis following cataract/lens procedures.
If infectious scleritis is suspected, scleral scrapings should be sent for microbiological cultures and polymerase chain reaction. In addition, testing for tuberculosis (Mantoux test), syphilis (VDRL test or Treponema pallidum hemagglutination assay), HIV infection, hepatitis B, hepatitis C, herpes simplex, and varicella-zoster viruses should be performed.
Radiology. Radiologic investigations include chest imaging to look for evidence of tuberculosis, sarcoidosis, and granulomatosis with polyangiitis, as well as imaging of the joints for rheumatoid arthritis.
Differential Diagnosis
Infectious scleritis. The relationship between SINS and infection is not clearly understood. Although SINS and infectious scleritis are considered to be separate clinical entities, SINS can be initiated by an infection, or it can predispose to secondary infection.7
Infectious scleritis can be bacterial, fungal, viral, or parasitic, with the most common etiological agent being P. aeruginosa.8 Other organisms include varicella-zoster virus, Mycobacterium tuberculosis, M. leprae, and T. pallidum. The presence of scleral abscess and involvement of adjacent cornea is more suggestive of an infectious etiology than of noninfectious SINS.
It is critical to distinguish between infectious and immune-mediated scleritis before initiating treatment, as they are managed differently. Infectious cases are treated with topical or systemic antimicrobial agents, sometimes accompanied by debridement of necrotic tissue to reduce the load of microorganisms and aid in medication penetration.
In contrast, corticosteroids or immunosuppressants are the mainstay of therapy in immune-mediated scleritis. Because these agents worsen infectious scleritis, any infectious etiology must be ruled out before beginning treatment.
Autoimmune necrotizing scleritis. Most commonly seen in middle-aged women with rheumatologic disease, autoimmune necrotizing scleritis is associated with worsening vasculitis. Both eyes tend to be affected, although the disease may progress differently in each eye and at different rates. Rarely, it can occur without pain and injection and may lead to ocular perforation, a condition known as scleromalacia perforans. Although autoimmune necrotizing scleritis and SINS are not mutually exclusive, a history of ocular surgeries with inflammatory response around the site of the surgery favors a diagnosis of SINS.
Treatment
Medical. NSAIDs are usually not effective for SINS; thus, systemic immunosuppressive treatment in the form of corticosteroids and other immunomodulatory agents should be initiated without delay once an infective etiology has been ruled out. Systemic steroids should be started at a high dose and tapered to a maintenance dose when clinical recovery is seen.
Long-term systemic steroid therapy should be avoided because of its side effects, and steroid-sparing therapy instituted if prolonged therapy is required. These therapies include antimetabolites such as methotrexate, mycophenolate, and azathioprine; calcineurin inhibitors such as tacrolimus; cytotoxic agents such as chlorambucil and cyclophosphamide; and biologic therapies, including the tumor necrosis factor inhibitors adalimumab and infliximab. Hematological, urological, and systemic monitoring is required when the patient is on these drugs. Delay in initiating immunosuppressants is associated with a poorer visual prognosis.
Surgical. If the disease progresses despite medical therapy and in the event of an impending perforation, aggressive surgical measures may be considered to support and salvage the globe. These include excision of granulation tissue and support in the form of tissue adhesives, scleral patch grafts, amniotic membrane grafts, and conjunctiva-Tenon grafts.
___________________________
1 O’Donoghue E et al. Br J Ophthalmol. 1992;76(1):17-21.
2 Watson PG, Hayreh SS. Br J Ophthalmol. 1976;60(3):163-191.
3 Doshi RR et al. Surv Ophthalmol. 2013;58(6):620-633.
4 Morley AM, Pavesio C. Eye (Lond). 2008;22(1):162-164.
5 Madanagopalan VG et al. GMS Ophthalmol Cases. 2019;9:Doc18. Published May 29, 2019.
6 Shalaby U, Heikal MA. Am J Ophthalmol Case Rep. 2016;3:47-49.
7 Rich RM et al. Am J Ophthalmol. 2008;145(4):695-699.
8 Hsiao CH et al. Br J Ophthalmol. 1998;82(1):29-34.
___________________________
Dr. Gaonker and Dr. Yadav are ophthalmology residents, Dr. Rastogi is a director professor, and Dr. Bansal is an assistant professor of ophthalmology. All are at Guru Nanak Eye Centre, Maulana Azad Medical College, New Delhi. Financial disclosures: None.