Download PDF
This past year, Leon W. Herndon Jr., MD, spent countless hours on Zoom calls discussing what the twin crises of COVID-19 and racial injustice laid bare—the glaring disparities in eye care delivery and research among underrepresented minority groups.
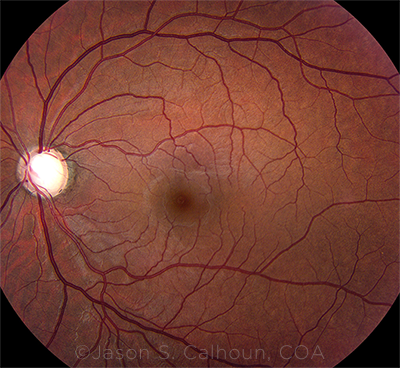
Glaucoma specialists like Dr. Herndon are well aware of the social determinants of health. After all, research has shown that primary open-angle glaucoma (POAG) is six times more prevalent among Blacks than in age-matched Whites, with Blacks exhibiting more severe disease that is resistant to intervention and results in higher rates of blindness.1
Toll on Patients’ Vision
While the genetic underpinnings of glaucoma continue to be studied, the relationship between socioeconomic status, ethnicity, access to eye care, and reduced quality of life also play a role in glaucoma development and disease severity. And in a March 2021 keynote talk to the International Agency for the Prevention of Blindness, Dr. Herndon noted that this web of intersecting factors is taking a direct toll on patients’ vision.
“I am not a social sciences researcher, but I have lived my entire life witnessing inequities in health care,” said Dr. Herndon, at Duke University Eye Center in Durham, North Carolina. “There is so much information that many ophthalmologists are not aware of. If we as a profession are to make an impact, we must be aware of the problems, educate ourselves, and be open to change.”
 |
|
OUTSIZED IMPACT. The likelihood of developing POAG—and experiencing its complications—is higher in Black patients.
|
One Step Forward, Two Steps Back?
Three decades ago, when Eydie Miller-Ellis, MD, was a resident at the University of Pennsylvania in Philadelphia, she became interested in glaucoma after witnessing patient after patient fall through the cracks of the health care system.
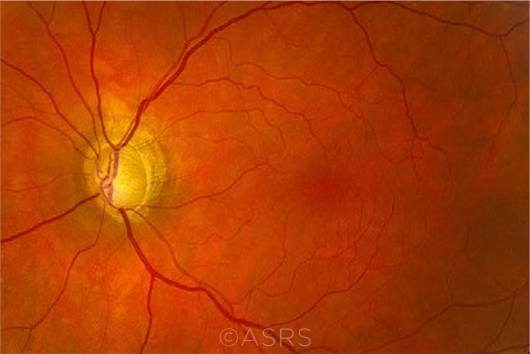
“A lack of follow-up, marginal patient education, and low treatment compliance was resulting in needless vision loss in individuals with glaucoma,” Dr. Miller-Ellis said. “Glaucoma is the No. 1 cause of preventable blindness, disproportionately affecting individuals of African descent—and glaucoma runs in my family. I thought glaucoma is where I could make the biggest difference.”
Ongoing economic fallout. Thirty years later, while Dr. Miller-Ellis has seen great progress in treatment, disparities in glaucoma care have actually become worse, as even more patients are not able to access—or have become lost in—the health care system, or have needed to sacrifice their health in general because of a lack of a societal safety net.
Role of insurance coverage. “While the Affordable Care Act has tried to close the coverage gaps, extensive access challenges still exist,” Dr. Miller-Ellis said. “Patients in underserved communities are less able to navigate the current insurance system, which prevents them from receiving the health care they need.”
For example, the insurance authorization process for medications and procedures often places barriers between the physician and their glaucoma patients. “In some offices, the situation is so difficult that the staff give up trying, and the patient suffers,” Dr. Miller-Ellis said.
She also argues in favor of universal, basic health care insurance: “Individuals should not have to choose between paying rent and paying for their health care and medications.”
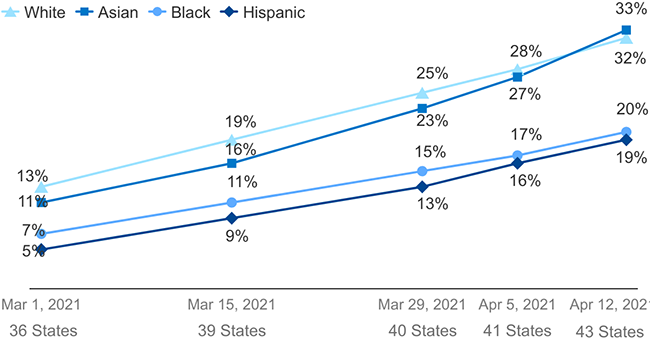
Impact of COVID. During the pandemic, Blacks and Hispanics have been more likely to visit the emergency room for—or be hospitalized with—SARS-CoV-2.2,3 And once sick, they were more likely to die of COVID than were Whites.4 The pandemic also had a significant impact on socioeconomic measures of well-being, such as employment rates (see “The Statistics Tell the Story”).
Despite the abrupt and severe impact of the pandemic, “we didn’t get this way overnight,” Dr. Herndon said. “We cannot solve these inequities without taking into consideration the structural racism rooted in our society. It is going to take a lot of awareness, education, and empathy.”
Factors That Drive Health Outcomes
|
 |
|
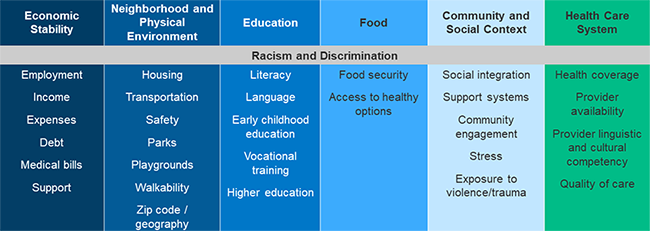
OVERLAPPING CHALLENGES. Determinants of health outcomes include myriad social and economic factors. SOURCE: Adapted from the Kaiser Family Foundation.
|
Disparities in Delivering Care
As Dr. Herndon noted, the social determinants of health have deep and complex roots.5,6 For instance, the systemic disinvestment in segregated neighborhoods has resulted in under-resourced medical facilities. In turn, this pattern of disinvestment makes it difficult to attract experienced primary care providers—which, in turn, impacts patient access to and utilization of health care.6
Who gets tested? In the age of big data, individual utilization of health care resources is becoming easier to ascertain. For example, Dr. Miller-Ellis pointed out, data can show whether a patient with a diagnosis code for glaucoma is receiving the appropriate diagnostic tests.
“Research has demonstrated that minority populations do not receive all of the testing they need, as opposed to majority populations,” Dr. Miller-Ellis said, citing study findings indicating large disparities in the receipt of glaucoma care between Medicaid enrollees and patients with commercial insurance.7 For this study, researchers followed 21,766 patients with newly diagnosed open-angle glaucoma (OAG) enrolled in Medicaid or a large U.S. managed care network. The results showed that patients with Medicaid insurance were less likely to receive glaucoma testing in the 15 months following initial diagnosis than those in the managed care program.
Additionally, nearly half (49%) of all OAG patients with Medicaid insurance had no record of any glaucoma testing in the first 15 months following the initial diagnosis, while only 1 in 5 (21%) with commercial health insurance had no record of any glaucoma testing. Moreover, the odds of receiving no glaucoma testing in patients with Medicaid coverage, when compared with those with commercial coverage, were 198% higher for Whites, 291% higher for Blacks, and 167% higher for Hispanics.
“Even within the Medicaid group, all of whom have lower socioeconomic status, Black patients with a blinding eye disease are less likely to be adequately followed than their majority population counterparts,” Dr. Miller-Ellis said.
How can compliance be encouraged? Compliance in glaucoma treatment is essential. “Yet if someone has a complicated life, it is harder to keep up with treatment maintenance,” Dr. Miller-Ellis said. “If your home situation is unstable or chaotic, it is more difficult to care for your own health issues.”
This scenario is exacerbated in women, who often are caretakers for children and aging parents. That’s because caretakers tend to neglect themselves, Dr. Miller-Ellis noted. In addition, people who are economically disadvantaged have a hierarchy of concerns, including securing food and shelter, so eye care may not even be on their list. “These factors greatly impact whether patients can return for follow-up visits,” Dr. Miller-Ellis said. “And it takes many office visits to get a glaucoma patient under control.”
Educating patients. Getting patients to buy into using daily eyedrops and sticking with their treatment plan involves health literacy and education, Dr. Miller-Ellis said. “As physicians, we are charged with having to communicate with our patients in ways they can understand. Since many of my patients are visual learners, I provide written instructions that are clear so that key directions can be easily followed.”
Choosing treatment. Issues of compliance also may prompt a clinician to recommend surgery instead of medication. “I advocate early intervention with laser trabeculoplasty or incisional glaucoma surgery to lessen the long-term challenges with medication compliance,” Dr. Miller-Ellis said.
 |
|
TOLL ON VISION. The likelihood of glaucoma complications is higher in minority populations.
|
Disparities in Research
One of the major burdens facing marginalized people with debilitating eye conditions is the lack of relevant research.
Who gets studied? Glaucoma serves as a key example of this, as most research has been conducted in Whites. This leads to huge gaps in understanding and clinical care, Dr. Herndon said. He quoted Liu et al.: “To tackle the elevated burden of eye disease facing marginalized communities, we need to promise and fulfill our commitment to increase racial and ethnic inclusion in clinical trials. Without addressing this important issue, we risk perpetuating rather than resolving current health disparities.”8
Focus on genetics. Janey L. Wiggs, MD, PhD, at Harvard Medical School in Boston, noted that the majority of genetic studies in glaucoma have been in Whites who are of European ancestry. “When you think about the translatability of genetic information from glaucoma research to clinical care, the patients who are going to benefit the most from genetic studies are White because of the nature of the data.”
She added, “Historically, information from genetic investigation of individuals of African ancestry has been missed, which limits the diagnostic and therapeutic applications. To help gain more insight into glaucoma, we need more research on large populations of African ancestry, and this is a crucial step for the field.”
Dr. Wiggs noted that these disparities are seen throughout medicine, as many genetic studies have primarily been conducted in White populations. She cited the use of polygenic risk scores derived from genome-wide association studies (GWASs) to assess disease risk. “These risk scores are beginning to be used in diseases with complex inheritance such as glaucoma for risk stratification and treatment consideration.”
“However,” she added, “currently these polygenic risk scores have been primarily tested using White patients. This is because the studies that generated the scores were mainly performed in Caucasian individuals. We cannot yet predict if these scores have any relevant predictability in African ancestry populations, and we need more research to determine whether these scores are transferable to individuals of African ancestry.”
Promising shift in direction. Research inequities are beginning to be addressed, however, as efforts by the following research groups indicate:
Genetics of Glaucoma in People of African Descent Consortium. This group performed a GWAS of African-ancestry populations for POAG.9 The study discovered a genetic variant in the APBB2 gene associated with a higher risk of POAG, and the genetic association was discovered only in individuals of African ancestry.
International Glaucoma Genetics Consortium. This group recently published a study showing that many glaucoma genetic risk factors have similar effects on disease risk in people of European Caucasian, African, and Asian ancestry.10
“This study, which identified risk loci contributing to the development of POAG across ethnic groups, is an advance over prior POAG GWAS studies that have mainly focused on individuals from a single ancestry group,” Dr. Wiggs said. “However, it is important to note that further research in ethnic groups not currently well represented in genetic research is needed.”
University of Pennsylvania. Penn researchers have been investigating the genetics of glaucoma in Blacks through the POAAGG (Primary Open-Angle African American Glaucoma Genetics) study.11 “Our study has recruited more than 10,200 African Americans from the city of Philadelphia,” Dr. Miller-Ellis said.
Community outreach was an essential part of this study. The researchers partnered with community leaders to spread the word about the study and glaucoma risk. “We also offered free glaucoma screenings at our institute,” Dr. Miller-Ellis said. “These efforts allowed us to collect full phenotypic information on more than 90% of glaucoma patients.”
In addition, Penn researchers performed a GWAS on cases and controls in this population, as well as whole-exome sequencing in collaboration with Regeneron Genetics Center. “Thus far, we have identified a novel variant on chromosome 11 near the TRIM66 gene,12 as well as several genes associated with POAG-related quantitative traits,” she said. “These results confirm that POAG is a heterogeneous disease characterized by distinct phenotypes. Our long-term goals are to define the genetic subtypes of POAG and to develop more targeted diagnostic and therapeutic interventions for this most affected population.”
The Statistics Tell the Story
Evidence of social and health inequities to consider:
Median household assets. In 2011, these figures were $110,500 for White, $7,683 for Hispanic, and $6,314 for Black households.1
Unemployment. In March 2020, the unemployment rate was 6.8% among Blacks, 6% among Hispanics, and 3.9% among Whites. The next month, these percentages skyrocketed to 16.7% for Blacks, 18.9% for Hispanics, and 14.1% for Whites. By March 2021, these rates improved to 9.6% for Blacks, 7.9% for Hispanics, and 5.4% for Whites.2
Life expectancy at birth. In 2014, Whites could expect to live to age 79, versus age 82 for Hispanics and 74 for Blacks.1 But the pandemic could be expected to reduce U.S. life expectancy in 2020 by 0.68 years for Whites, 2.10 years for Blacks, and 3.05 years for Hispanics.3
Heart disease and mortality. In 2014, the age-adjusted mortality related to heart disease—the No. 1 cause of death in the United States—per 100,000 population was 166 for Whites, 116 for Hispanics, and 206 for Blacks.1
___________________________
1 Bailey ZD et al. Lancet. 2017;389:1453-1463.
2 U.S. Bureau of Labor Statistics. Current Population Survey. www.bls.gov/cps. Accessed April 15, 2021.
3 Andrasfay T, Goldman N. Proc Natl Acad Sci. 2021;118(5):e2014746118.
|
COVID-19 Vaccination Rates
|
 |
|
WHO’S VACCINATED? Estimate of vaccination rates by ethnicity, from March 1 to April 12, 2021, based on publicly available data on state websites. SOURCE: Adapted from the Kaiser Family Foundation.
|
An Often-Overlooked Factor
Dr. Herndon noted that a key factor contributing to health care disparities is the lack of diversity in the physician workforce. (EyeNet will cover this topic later this year.)
“There is strong evidence that communication in racially discordant medical interactions is usually less productive and positive in content and tone than in racially concordant interactions,” Dr. Herndon said. “A variety of studies have shown that racial discordance leads to less relationship building, less health information exchange, and less treatment planning.”
This discordance can be traced to the low percentage of members of minority groups in the physician workforce, Dr. Herndon noted. For instance, he said, “In 2015, only 2.5% of practicing ophthalmologists were Black. Our numbers are not improving, yet for the health of the patient it is essential that providers reflect the community they serve.”
To address these inequities, ophthalmology as a profession must focus on creating a pipeline of underrepresented minority groups to enter the field. Role models are a key component of these efforts. Dr. Herndon recalled his own experience as a medical student when he reached out to Dr. Miller-Ellis, who was at the University of North Carolina, Chapel Hill, at the time.
“Here was someone who looked like me doing ophthalmology,” Dr. Herndon said. “Dr. Miller-Ellis was such an inspiration and gave me the confidence to pursue a career in ophthalmology. We need more role models who can inspire young medical students of color to pursue the field of ophthalmology.” (See “Academy Resources.”)
27 Measures of Health Care by Ethnicity
|
 |
|
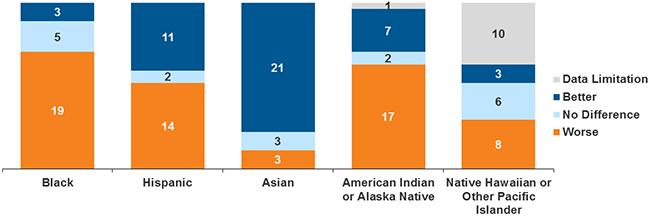
INSURANCE COVERAGE. This chart shows how well members of different ethnic groups fared, compared to Whites, after the ACA was implemented. Areas assessed included access to care, diagnosis rates, and health outcomes. SOURCE: Adapted from the Kaiser Family Foundation.
|
Moving Forward
Dr. Miller-Ellis noted that the University of Pennsylvania, under the leadership of Eve J. Higginbotham, SM, MD, ML, has been at the forefront of change (see “What’s in a Word?”).
“While diversity, health disparities, and inclusion have been discussed for years, the events of 2020 have put these issues at the forefront,” Dr. Miller-Ellis said. “We are finally seeing a real commitment from the government, health providers, and insurers to move these initiatives forward—working on inclusion in bench research and clinical trials while addressing disparities in health care.”
She added, “Sometimes it takes a disaster to see the holes in the safety net, and the COVID-19 pandemic showed how a lot of people—particularly those from minority communities—are falling disproportionately through those holes. However, if we as a society can address issues facing the most disadvantaged of people, it will help everyone. Diverse ideas make organizations better. We need to keep moving forward.”
What’s in a Word?
Dr. Higginbotham, a glaucoma specialist, has written extensively about diversity in medicine, including an article published earlier this year.1 EyeNet spoke with her about reconsidering and redefining the word “race” when addressing ethnic disparities in the delivery of eye care.
Q: What are the historic roots of America’s culture of racism?
Dr. Higginbotham: Going back to the 1600s, there was a need to bring in another group of individuals to do the hard work of developing this country and creating an agricultural system to feed the population. To justify this system, those I call “pseudoscientists” created an artificial categorization of the human population so that this group of individuals who looked different from European settlers could be considered “the other.” Individuals like Samuel Morton, who published in the first half of the 19th century, actually developed a system for describing the world’s population in a racial hierarchy so that Europeans (at the time, they were called Caucasians) were at the highest level and Africans were at the lowest level. These beliefs were reinforced by faith-based groups, politicians, and others, who deeply embedded these false assertions into societal norms.
This thinking has carried forth in the United States hundreds of years later to the 2020 murder of George Floyd. I am always reminded during those 9 minutes and 29 seconds that the police officer kneeling on George Floyd’s neck did not think of this American citizen, a devoted father and brother, as human—but rather as less than. And I immediately thought of Samuel Morton and the way his thinking has permeated through the fabric of our entire culture in the United States.
Race is a social construct, not a biological construct, but people still carry that thinking because society has been conditioned to think that way.
Q: Please explain how race is a social construct.
Dr. Higginbotham: Europeans include, for example, Italians, Austrians, and Swedes—but when they come to the United States, they are all considered White. And anyone who has brown or black skin is considered Black or African American. Yet the world is not like that.
Anthropologists report that we have more variation within populations than between populations. Consequently, “race” is an artificial, social construct that has haunted us all of these years, and it is only through education and open and frank discussion that we really understand we cannot carry this artificial construct into the biomedical sciences and health care.
In the 1990s, the American Anthropological Association said we shouldn’t use “race” as a term because the presumptions surrounding the use of the term do not align with anthropological observations. It goes against the findings that the continent of Africa, the origin of civilization, is the most diverse continent in the entire world. So how can you say that this continent of Africa is generating one single group of individuals? Our recent article in The New England Journal of Medicine1 outlines an approach for considering race in both the curriculum and the practice of medicine. For example, we should be more specific in describing the ancestry of patients and state, for instance, that this patient originates from Ethiopia, rather than simply stating Black. Ask the patient about his or her ancestry.
Currently, we find entire systems of laws and policies that have created structural racism, systems built on the pseudoscience of Morton and others. And this practice of separating groups based on phenotypic characteristics is firmly entrenched in the medical sciences, even though the human genome project did reveal that we are 99% the same—all humans globally. Yet there is still this tendency to want to divide us into four or five groups of individuals across the world. And we are not listening to the science as a community, since many physicians and scientists believe race has a biological basis, and it does not. Our health is driven far more significantly by our zip code than by genetics.
Q: How do we move past this misperception of race?
Dr. Higginbotham: When we consider glaucoma, I use the Ocular Hypertension Treatment Study (OHTS) as a way for glaucoma specialists to disconnect from this archaic thinking. The OHTS teed up five key risk factors for glaucoma, including age, cup-to-disc ratio, whether or not the visual field at baseline has patterns of decreased sensitivity, and intraocular pressure. (Also see “OHTS: 20 Years of Follow-up Data on POAG.”2)
But the key risk factor is central corneal thickness (CCT), which is our opportunity to say that African Americans and Latinx populations are certainly at higher risk. It is essential to lean into a biologically measurable risk factor and not refer to the color of people’s skin, and to use CCT as the key risk factor that helps define who will actually develop glaucoma in addition to the four other risk factors.
Q: What steps can ophthalmologists take to address eye care disparities?
Dr. Higginbotham: I believe that ancestry is a better way to think about one’s lineage in connection to a disease process rather than the continued use of “race.” The word has such an ugly set of historical roots that it keeps people thinking in the same way, and it doesn’t move our conversation forward. It contributes to provider and scientific bias.
When treating eye diseases such as glaucoma, we should talk about ancestry, about risk factors related to whether or not the individual had previous surgery, about the medications they are on—in essence, do more of a personalized approach to treatment as opposed to putting people in a bucket based on the color of their skin.
Additionally, we need to understand our own implicit biases, to lean into practice guidelines, to reconsider the role of “race” when reading those practice guidelines, and to think instead about ancestry. We have to focus on the social determinants of health to address inequities in care and aggressively work towards diversifying our ophthalmic and biomedical workforce.
On the structural and systems level, we need to look at our policies and processes. We need to diversify the boards of companies that do work in ophthalmology and visual sciences, we need to examine our own policies within our practices and our institutions to be sure they are using a lens of equity, and we need to develop a way to measure our progress that ensures that we emphasize health equity as an aspiration for our community.
___________________________
1 Amutah C et al. N Engl J Med. 2021;384(9):872-878.
2 Kass MA et al. JAMA Ophthalmol. Published online April 15, 2021.
|
Academy Resources
For more information, see the following:
Web page. Information on health care disparities and diversity, equity, and inclusion (DEI), including two related task forces, is available at aao.org/diversity-equity-and-inclusion.
Mentoring. Three years ago, the Academy, in partnership with the American Academy of University Professors, launched the Minority Ophthalmology Mentoring program. See aao.org/minority-mentoring.
|
Further Reading
During the past year, Dr. Herndon took advantage of the COVID lockdown to read extensively. His goal, he said, was “to educate myself and to dive further into the root causes of structural racism.” He described his reading list, below, as “a good place to start to educate yourself from a historical perspective.”
- Darity WA Jr., Mullen AK. From Here to Equality: Reparations for Black Americans in the 21st Century. University of North Carolina Press; 2020.
- DiAngelo R. White Fragility: Why It’s so Hard for White People to Talk About Racism. Beacon Press; 2018.
- King ML Jr. Stride Towards Freedom: The Montgomery Story. Beacon Press; 2010.
- Tweedy D. Black Man in a White Coat: A Doctor’s Reflections on Race and Medicine. Picador; 2016.
- Zucchino D. Wilmington’s Lie: The Murderous Coup of 1898 and the Risk of White Supremacy. Grove Press; 2021.
|
___________________________
1 Racette L et al. Surv Ophthalmol. 2003;48(3):295-313.
2 Smith AR et al. MMWR. 2021;70(15):566-569.
3 Romano SD et al. MMWR. 2021;70(15):560-565.
4 Ahmad FB et al. MMWR. 2021;70(14):514-522.
5 Bailey ZD et al. Lancet. 2017;389(10077):1453-1463.
6 Bailey ZD et al. N Engl J Med. 2021;384(8):768-773.
7 Elam AR et al. Ophthalmology. 2017;124(10):1442-1448
8 Liu AJ et al. JAMA Ophthalmol. Published online Oct. 8, 2020.
9 Hauser MA et al. JAMA. 2019;322(17):1682-1691.
10 Gharahkhani P et al. Nat Commun. 2021;12(1):1258.
11 Charleson ES et al. Ophthalmology. 2015;122(4):711-720.
12 Gudiseva HV et al. www.biorxiv.org/content/10.1101/2020.02.27.968156v1.
Meet the Experts
Leon W. Herndon Jr., MD Professor of ophthalmology and chief of the glaucoma division at Duke University Eye Center in Durham, N.C. Financial disclosures: None.
Eve J. Higginbotham, SM, MD, ML Vice Dean for Inclusion and Diversity at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia. She is also a senior fellow at the Leonard Davis Institute for Health Economics and professor of ophthalmology at the University of Pennsylvania as well as Vice Chair of the Ocular Hypertension Treatment Study. Financial disclosures: NEI: S.
Eydie Miller-Ellis, MD Professor of clinical ophthalmology and Vice Chair for Faculty Affairs and Diversity for the Scheie Eye Institute at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia. She also serves as the chief of glaucoma service and director of the glaucoma fellowship program at the Scheie Eye Institute and director of glaucoma at the Philadelphia Veterans Administration Medical Center. Financial disclosures: Aerie: C; Allergan: C; NIH: S.
Janey L. Wiggs, MD, PhD Paul Austin Chandler Professor of Ophthalmology and the Vice Chair for Clinical Research in Ophthalmology at Harvard Medical School in Boston. She also directs the genetic testing laboratory at Massachusetts Eye and Ear and is codirector of the Ocular Genomics Institute and the Glaucoma Center of Excellence. Financial disclosures: Aerpio: C,S; Allergan: C; Editas: C; Maze: C; NIH: S; Regenxbio: C.
See the disclosure key at www.aao.org/eyenet/disclosures.