Download PDF
Telemedicine has the potential to transform ophthalmology. But some challenges remain before it can fulfill its promise.
Telemedicine’s time has come. Thanks to multiple technological advances, the push for more affordable and accessible health care, and the gradual expansion of reimbursement for electronic health services, telemedicine is in the process of transforming many medical specialties, including ophthalmology. And while ophthalmologists are no strangers to telemedicine—think of the increasingly routine process of store-and-forward transmission of diabetic retinopathy images—they are still coming to terms with what it really means for clinical practice. Any major change in how physicians run their practices has the potential to be a disruptive force, and teleophthalmology is no exception. It touches on all aspects of ophthalmic practice, including training, licensure, and reimbursement.
“Successful teleophthalmology programs do exist, and that gives all of us faith that such systems are feasible,” said Michael F. Chiang, MD, at Oregon Health & Science University’s Casey Eye Institute in Portland. Yet, despite recent progress, he and other experts note that real-world operational challenges still abound.
Changes in Attitudes?
Most ophthalmologists are keenly aware that information technology (IT) “has transformed the way we communicate with each other and exchange medical information,” Dr. Chiang said. They also express “a need and a desire for teleophthalmology,” he said.
And an aging population—with a concomitant rise in diseases such as age-related macular degeneration (AMD)—plus a relatively stable supply of ophthalmologists means that demand for ophthalmic care is outpacing supply. “Our patients often have to travel very far, especially for subspecialty care,” Dr. Chiang pointed out.
Lingering unease. However, the same ophthalmologist who may readily send digital images to a trusted colleague via a smartphone may have little confidence in a formal teleophthalmology network. In a study published last year, Maria A. Woodward, MD, and her fellow researchers at the University of Michigan, Ann Arbor, surveyed their ophthalmology colleagues regarding their experience with and perceptions of teleophthalmology.1 The survey, which was conducted anonymously, revealed that while the majority of the 58 respondents said that they were willing to participate in telemedicine, they also had significant reservations about doing so. In particular, Dr. Woodward said, a substantial percentage (59%) of the respondents noted that they had “low confidence” in their ability to make decisions concerning patient care based on images alone.
Confusion about scope. Interestingly, the University of Michigan survey found that many ophthalmologists seem to define telemedicine too narrowly: Even though 71% of the respondents said that they had never used telemedicine, more than half of them also reported that they had received digital images via the Internet (phone or email) from either referring physicians or patients within the previous 3 months.
According to the American Telemedicine Association (ATA), “Formally defined, telemedicine is the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status. Telemedicine includes a growing variety of applications and services using two-way video, email, smart phones, wireless tools and other forms of telecommunications technology.”
Need for education. The fact that such confusion—even about the basic definition—still exists points to an urgent need for education. “Ophthalmologists need to know how to do teleophthalmology properly,” said Michael T. Trese, MD, who practices in Royal Oak, Mich. “They need to know about DICOM [Digital Imaging and Communications in Medicine] standards and compliance, HIPAA regulations, and hardware and software.” Dr. Trese, who also chairs the Academy’s teleophthalmology task force, is fully engaged in this educational effort (see “Telemedicine Education at AAO 2016” below). “There is a lot to be learned,” he said.
Patient perceptions. What about the flip side: What do patients think of teleophthalmology? In a separate survey, Dr. Woodward—along with Paul P. Lee, MD, JD, and their colleagues at the University of Michigan—asked precisely that question of 97 patients. Although results from earlier studies suggest that patients are open to trying new technologies,2 the Michigan researchers found a certain amount of reluctance with teleophthalmology. Specifically, patients who had multiple ocular and other medical conditions said that they were less willing to participate in telemedicine.3 The authors reported that patients who visit medical centers frequently (or otherwise have good access to care) and those with established physician relationships are less interested in telemedicine.
Telemedicine Education at AAO 2016
At October’s AAO 2016 in Chicago, make time to attend a telemedicine instruction course or Breakfast With the Experts roundtable.
- Ophthalmic Telemedicine 2016 (instruction course, Michael T. Trese, MD)
- Update on Diagnosis and Management of ROP: Pearls for ROP Screening; Introduction of Telemedicine and Use of Anti-VEGF Medications in Practice (instruction course, Nasrin N. Tehrani, MBBCh)
- How to Start a Telemedicine Program for ROP (Breakfast With the Experts roundtable, Daniel Weaver, MD)
Starting June 22, learn more online.
|
Significant Challenges
Although teleophthalmology has the potential to improve communications and patient care, is it ready for wide adoption? Some experts say not yet. Regarding retinopathy of prematurity (ROP), for example, a joint technical report prepared by the American Academy of Pediatrics (AAP), American Academy of Ophthalmology (AAO), and American Association of Certified Orthoptists (AACO) states, “The general consensus of the literature and this panel is that RDFI-TM [remote digital fundus imaging via telemedicine] does not supplant BIO [binocular indirect ophthalmoscopy] for ROP evaluation.”4
As for patients with diabetes, the Academy Preferred Practice Pattern for Diabetic Retinopathy5 says that there is value in an in-person ophthalmologic exam, and an Academy Ophthalmic Technology Assessment states that a visit to the clinic provides an opportunity to educate the patient and look for associated eye conditions.6
To build a case for teleophthalmology, according to Dr. Chiang, “The challenge is to prove not only that it works but also that you can do it in a way that is secure and safe—and that doesn’t overload physicians with information.” Following are some of the issues that come into play.
Quality of care. As the Michigan study of clinicians suggests, quality of care appears to be a leading concern of ophthalmologists. In part, it’s because teleophthalmology interferes with the classic pattern of a physician’s physical examination of and interaction with his or her patients, Dr. Chiang said. And while he acknowledged that this is a legitimate concern, he added, “There has been work done in retina showing that a diagnosis that’s made by image interpretation can be every bit as accurate as—and in some cases, more accurate than—a physical exam.” (See references 7 and 8.)
Dr. Trese agreed. “Teleophthalmology can actually be better medicine. Retinopathy of prematurity screening is a good example: Previously, the physician would draw a fundus image on a piece of paper; now we can use computer-aided systems to reduce subjectivity in ROP screening and assist physicians in making a diagnosis.” He added, “Our group has been doing store-and-forward transmission of ROP images for the past 5 years. When I showed a hospital administrator the difference between the 2 approaches, he was stunned. He asked me, ‘But ... what we’re doing is that scribbling?’”
Liability. “There are a few different legal domain areas with regard to teleophthalmology,” said Dr. Lee. “To begin with, you have standard malpractice considerations. Having the images is potentially protective. Can you prove what you saw? Were the images representative of what was actually present? How good were they?” He added, “This is where e-ROP and other good controlled studies help us, because they have found that the images are as good as the best in-person exam. That gives you a good cushion of protectivity.”
The AAP-AAO-AACO technical report discusses risk management considerations in some depth with regard to remote screening for ROP.4 “To our knowledge, there has not yet been a lawsuit related to ROP in which the patient was screened [via teleophthalmology]. The risks related to telemedicine in situations other than ROP screening and the risks of BIO screening have been tested in many cases, however.”
State licensure laws also raise liability concerns, Dr. Lee said. But the laws governing licensure are beginning to change, albeit in a piecemeal and somewhat confusing manner (see below, under “Moving Forward?”).
Image quality. “Most teleophthalmology programs fail to realize that the ungradable rate is a critical issue,” said Paolo S. Silva, MD, at the Joslin Diabetes Center’s Beetham Eye Institute in Boston. “If an image is ungradable, that encounter becomes unusable. The patient won’t benefit, and it drains resources from the program.” Furthermore, he said, “Most payers won’t pay for an ungradable image—that by itself is a big drain to the system. If you can reduce the rate of ungradable images, that will improve the financial sustainability and clinical effectiveness of the program.”
Ophthalmologists need to ask themselves, “Are there protocols for when or how to say that I don’t have enough quality information to make a diagnosis?” Dr. Chiang said. “If the image isn’t of high quality, what’s my trigger point of saying, ‘This isn’t good enough; you have to do it again.’?”
Fortunately, recent improvements in imaging technology have the capacity to reduce the rate of ungradable images. Dr. Silva and other researchers who participate in the Joslin Vision Network (JVN), a pioneering teleophthalmology program, are investigating the use of ultra-widefield (UWF) imaging. In a recent report from the JVN’s work with the Indian Health Service (IHS), nonmydriatic UWF imaging reduced the ungradable image rate by nearly 90% per patient.9 More than 20,000 patients with diabetes were imaged at 97 sites across 25 states.
“In this study, we were able to substantially decrease the number of IHS patients who needed to be referred for an eye exam, which is a considerable issue with patients who live in remote geographic areas,” Dr. Silva said. He did acknowledge that the cost of UWF imaging systems is a stumbling block for many teleophthalmology programs at this point. “Cost remains a big issue. But with large-scale programs, the cost can be spread out.”
Workflow. Even the best IT systems can be bogged down by practice workflow issues. Staff and physician training are paramount, Dr. Chiang said. “How do you train people to collect data remotely—and ensure that they can do it in a timely and high-quality way?” Physician training also comes into play, he added. “For physicians, this may be training in how you make a diagnosis remotely, versus by examining patients in the office.”
Dr. Trese added that you need to have personnel who are dedicated to setting up good workflow and following through. “There’s a lot of paperwork, a lot of time devoted to dealing with payers to get them to pay attention to telemedicine functions.” As the joint AAP-AAO-AACO technical report notes, “Protocols should clearly delineate workflow and roles/responsibilities.”4
Finally, Dr. Chiang noted, the time burden on physicians needs to be taken into account. “How do we design teleophthalmology systems to be sensitive to basic workflow issues affecting physicians? Do you have physicians review images at the end of the day? Or do you set aside ‘time outs’ at certain times of the day? These are all questions that need to be thought through.”
Security. Last year, in a nightmare scenario, a laptop was stolen from a faculty member at UCLA Health in Los Angeles. More than 1,200 patients had to be notified.10 And the Ophthalmic Mutual Insurance Company (OMIC) cites the case of an ophthalmic practice that had to notify hundreds of patients after a physician’s smartphone was compromised in a data breach.11
Although these cases didn’t necessarily involve telemedicine, they serve as a reminder that all the basics of data encryption, password protection, and adherence to federal regulations—including HIPAA-compliant backup and archiving—need to be in place with all devices, from workstations to mobile devices. “Networks have to be used properly,” said Dr. Trese. “Say you use a smartphone to send an image to a colleague, but you don’t send it via a properly protected email system. It’s then sent back—again, without being properly vetted. This type of circumstance is problematic and could backfire.”
Dr. Chiang also flagged another potential problem that can occur with laptops and smartphones: “It’s important to store only the minimum amount of data that you need on a laptop or smartphone. As soon as you can, upload it to the official medical record, so that it stays off of your mobile device and so that you can officially document the care that you’re providing. Ophthalmologists often don’t do this.” In addition to taking commonsense precautions, it’s important to stay compliant with current regulatory and technology standards, such as HIPAA and DICOM. (For more information, see “Resources” below.)
Moving Forward?
Despite these challenges, progress is occurring in several key areas, although clarity is hard to come by. “Everything is in flux right now,” Dr. Trese cautioned. “It’s almost as though you need to check on it every 3 months.”
Licensure. Teleophthalmology programs like the JVN have a built-in advantage when it comes to licensure, said Dr. Silva. In addition to its work with the IHS, the JVN has worked in the past with the U.S. Department of Defense and the Veterans Health Administration. “Because these are federal programs, you just need a single license to operate in all states. Otherwise, you’re bound by state licensure laws,” he said.
“In most cases, you have to be licensed in the state in which the patient resides,” said Dr. Lee. “However, there are some state medical board rulings that are exceptions, so you have to go on a state-by-state basis.” Last year, in a development that may move this forward, the Federation of State Medical Boards introduced the Interstate Medical Licensure Compact. This creates an expedited process for eligible physicians to apply for licensure in states that adopt the compact. To date, 12 states have passed the compact, and 14 states have bills pending. (To check the status of your state and view bill language, see www.licenseportability.org.)
Other proposed laws, including the TELE-MED Act of 2015 (at time of press, still stalled in committee), have targeted licensure issues in an attempt to remove barriers to telemedicine. But uniform standards are unlikely to be adopted quickly or smoothly. The ATA’s 2016 report on the status of physician licensure for telemedicine bluntly cites “a mix of strides and stagnation” in this arena.12
Financing and reimbursement. Financial sustainability can be a challenge, particularly for programs that are not university based or are not part of a federal program such as the IHS or Department of Defense and thus do not have a large patient population. In addition, billing and coding can present problems.
Payers vary significantly in their reimbursement policies, such as which services are covered and how the services should be billed. As the ATA puts it, providers “may encounter a patchwork of arbitrary insurance requirements and disparate payment streams that do not allow them to fully take advantage of telemedicine.”13
As with licensure, however, some movement has occurred on this front. For instance, last year, a number of states enacted laws that required commercial insurers to cover telemedicine services, and similar bills are in development in other states. More legislation is anticipated, driven primarily by the promise of cost savings.
What about coverage for telemedicine under Medicare and Medicaid? The Centers for Medicare & Medicaid Services (CMS) is considering expansion of coverage for telemedicine, although, as Dr. Trese put it, “CMS is trying to decide if telemedicine is going to cost them money or save them money.”
Dr. Trese cautioned, however, that ophthalmology isn’t always considered in federal and state legislation on reimbursement issues. “The last document I saw for a proposed federal law didn’t even address store-and-forward transmission, even though it’s the most common telemedicine application in ophthalmology.”
Looking Ahead
Research. Although the bulk of teleophthalmology research has involved ROP and diabetic retinopathy, researchers are investigating its use in other areas, as well. For instance, several research teams are evaluating the application of telemedicine algorithms to screening for glaucoma and AMD.
Dr. Woodward is among those who are investigating the use of teleophthalmology in screening for diseases of the anterior segment, such as corneal ulcers, cataracts, and ocular surface tumors. “We [ophthalmologists] can’t be everywhere. How do we screen in ERs and in the community? How can we reach rural and indigent populations?”
Perceptions. Overall, Dr. Woodward said, “I do think attitudes [about teleophthalmology] are changing among ophthalmologists. You can think of it along the lines of the stages of adaptation—you have the innovators, followed by the early adopters, then by the early majority, and so on.” While there may be some reluctance to embrace telemedicine, she said, “I think most ophthalmologists understand that this is headed their way and they need to be prepared.”
Along with more solid research and forward movement on the legislative and reimbursement fronts, some creative thinking may be required as well. As Dr. Chiang said, “Physicians have been pressured to see more patients in less time than ever before. Sometimes, I look at telemedicine and think, How can we come up with novel ways to extend our connections with patients? How can we leverage technology to connect well with patients even if we’re not right next to them?”
___________________________
1 Woodward MA et al. Telemed J E Health. 2015;21(4):271-273.
2 Aleo CL et al. Telemed J E Health. 2014;20(10):887-892.
3 Hansen S et al. “Attitudes Towards Telemedicine in Ophthalmology.” Presented at: ARVO; May 5, 2016; Seattle, Wash.
4 Fierson WM et al. Pediatrics. 2015;135(1):e238-e254.
5 American Academy of Ophthalmology, Retina/Vitreous Panel. Preferred Practice Pattern Guidelines. Diabetic Retinopathy. 2016.
6 Williams GA et al. Ophthalmology. 2004;111(5):1055-1062. Reviewed for currency in 2015.
7 Moss SE et al. Ophthalmology. 1985;92(1):62-67.
8 Scott KE et al. Ophthalmology. 2008;115(7):1222-1228.
9 Silva PS et al. Ophthalmology. Published online March 1, 2016.
10 www.uclahealth.org/news/ucla-health-notifying-patients-of-stolen-laptop-containing-personal-health-information. Accessed April 11, 2016.
11 www.omic.com/hipaa-proofing-your-smart-phone-or-mobile-device. Accessed April 11, 2016.
12 Thomas L, Capistrant G. State Telemedicine Gaps Analysis: Physician Practice Standards & Licensure. American Telemedicine Association. 2016. Accessed April 11, 2016.
13 Thomas L, Capistrant G. State Telemedicine Gaps Analysis: Coverage & Reimbursement. American Telemedicine Association. 2016. Accessed April 11, 2016.
Meet the Experts
Michael F. Chiang, MD Professor of ophthalmology and medical informatics and clinical epidemiology at Oregon Health & Science University’s Casey Eye Institute in Portland. Relevant financial disclosures: Clarity Medical Systems: unpaid member of the Scientific Advisory Board; NIH: S; Novartis: S.
Paul P. Lee, MD, JD Professor and chair of ophthalmology and visual sciences and director of the W.K. Kellogg Eye Center at the University of Michigan, Ann Arbor. Relevant financial disclosures: None.
Paolo S. Silva, MD Assistant professor of ophthalmology at Harvard Medical School and staff ophthalmologist and assistant chief of telemedicine at the Joslin Diabetes Center’s Beetham Eye Institute in Boston. Relevant financial disclosures: None.
Michael T. Trese, MD In practice with Associated Retinal Consultants and chief of pediatric and adult vitreoretinal surgery at William Beaumont Hospital in Royal Oak, Mich., and chair of the Academy’s teleophthalmology task force. Relevant financial disclosures: FocusROP: C,O.
Maria A. Woodward, MD Assistant professor of ophthalmology and visual sciences at the University of Michigan, Ann Arbor. Relevant financial disclosures: Intelligent Retinal Imaging Systems: C; NEI: S.
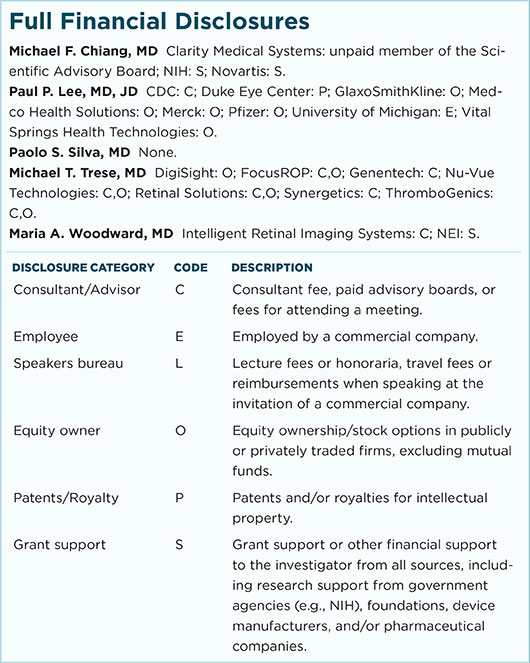
For full disclosures and the disclosure key, see below.
|