Download PDF
One Friday afternoon, after 2 days of gradually increasing pain, redness, and blurry vision in her right eye, Meryl McGuire,* the 62-year-old director of her county’s beautification department, decided to see her optometrist.
Initial Office Visit
Ms. McGuire described the vision in her right eye as being “greased over,” and she felt as if the eye was swollen. She reported having pain in that eye as well as intermittent severe headaches concentrated around it.
History. The patient’s ocular history was significant for chronic low-grade iritis in the right eye, which had been stable for many years, and uncomplicated cataract surgery in both eyes a few years ago. Her medical history was significant for diabetes mellitus, which was under good control.
Findings from the first exam. When examined at her optometrist’s office, Ms. McGuire had visual acuity of 20/30 in the right eye and 20/20 in the left. There was no relative afferent pupillary defect. Confrontation visual fields were full in both eyes, and motility was intact. She had 3+ conjunctival injection in the right eye. Intraocular pressure (IOP) was 50 mm Hg in the right eye and 20 mm Hg in the left.
Her optometrist noted neovascularization of the iris in the right eye and, suspecting neovascular glaucoma, emergently referred the patient to us.
We Get a Look
Ms. McGuire told us that she had never experienced such symptoms before this episode. In addition to her concerns about visual loss and increasing eye pain, she was worried about the possibility of needing an intraocular injection or laser treatment for neovascular glaucoma.
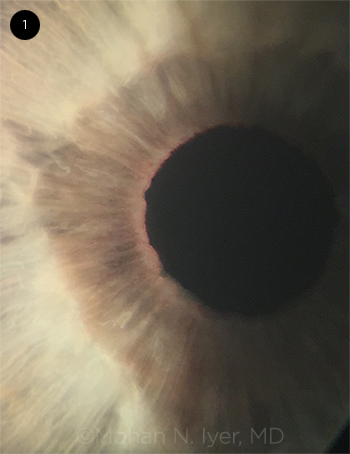
In our examination, we noted vessels on the iris (Fig. 1). Gonioscopy revealed microhyphema, grade III-IV angles, and fine blood vessels in the angle. No iris nodules or transillumination defects were apparent. We also found 4+ cells in the anterior chamber, which appeared to comprise both red blood cells and white blood cells. Corneal examination revealed fine keratic precipitates.
Dilated fundus exam of both eyes revealed optic nerves with a cup-disc ratio of 0.4, normal macula, vessels, and periphery. There was no evidence of retinal vascular attenuation, hemorrhages, neovascularization, or chorioretinal scars in either eye.
 |
|
EXAM FINDING. Iris vessels were noted at the pupillary margin in the right eye.
|
Making the Diagnosis
The presence of abnormal vessels on the iris and in the iridocorneal angles, together with increased IOP, was certainly suggestive of neovascular glaucoma. Neovascularization of the iris and angle typically develops as a result of elevated levels of vascular endothelial growth factor from retinal ischemia.1 The ischemia can be caused by many conditions; the most common include diabetic retinopathy, retinal vascular occlusion, and carotid artery occlusive disease. Given the patient’s normal fundus exam, we considered uveitis to be the most likely cause of the neovascularization.
A second look. However, when we stepped back and looked again at our patient, we noted that her right iris had a lighter color than the left (Fig. 2). When we mentioned this, Ms. McGuire recalled that she had been noted to have different-colored eyes, depending on the ambient light, for most of her adult life. With this information, we arrived at a diagnosis of Fuchs heterochromic iridocyclitis (FHI), as she had some of the hallmarks of this condition, including fine keratic precipitates, iris heterochromia, prior cataract, and fine vessels on the iris surface and in the iridocorneal angle.
We contacted her optometrist and learned that she had indeed been diagnosed with FHI approximately 10 years ago. During that time, she had undergone a laboratory workup for uveitis, which was negative.
 |
|
ON SECOND LOOK. Iris heterochromia, with the lighter-colored (bluer) iris in the affected right eye. The difference is more noticeable when viewed in daylight (top) than in the lighting of the exam room (bottom).
|
Discussion
FHI accounts for 1% to 3% of all uveitides; the actual prevalence may be higher, as it often goes undiagnosed. It is commonly diagnosed in the third to fourth decades of life, and there is no racial or sex predilection.
In 1906, the Austrian ophthalmologist Ernst Fuchs described the first large series of patients with chronic, typically unilateral inflammation and cataract affecting the lighter-colored eye. Dr. Fuchs hypothesized that the normal development of uveal pigmentation was inhibited, leading to iris heterochromia, followed by a low-grade inflammation.
Possible etiologies. Since then, several theories regarding the etiology have been proposed, including heredity; adrenergic denervation; infection by Toxoplasma gondii, rubella virus, or herpes simplex virus; immunologic response; and ocular trauma.2 Although many associations have been made, the exact etiology of FHI has not been confirmed and may well be multifactorial; therefore, the diagnosis of FHI is based on clinical findings.
Characteristics. Classic clinical findings of FHI include iris heterochromia and atrophy; fine, stellate, keratic precipitates; vitreous floaters, cells, or debris; fine vessels on the iris surface and in the angle; cataract; and low-grade iridocyclitis. The degree of heterochromia can be variable, but it is an important feature. The differential diagnosis for iris heterochromia includes congenital Horner syndrome, Waardenburg syndrome, diffuse iris melanoma, oculodermal melanosis, and herpes simplex uveitis.
Secondary and related conditions. FHI is often associated with secondary cataract and glaucoma. In most cases, the glaucoma is associated with an open angle and is thought to occur as a result of chronic inflammation. Other factors contributing to increased IOP include anterior synechiae formation, abnormal angle vessels, trabecular scarring, corticosteroid-induced ocular hypertension, and hyphema.
It is sometimes difficult to clinically distinguish FHI with secondary glaucoma from Posner-Schlossman syndrome, a condition characterized by recurrent glaucomatocyclitic crises and the occasional finding of iris heterochromia. However, the glaucoma associated with Posner-Schlossman syndrome is thought to be related to trabeculitis and responds rapidly to low-dose topical steroid treatment, while the glaucoma in FHI is typically unresponsive to topical steroid therapy.
Hyphema. It is unclear whether the vessels on the iris and in the iridocorneal angle are truly neovascular or simply abnormal iris vasculature, but they can bleed easily. Amsler’s sign (a hyphema that occurs when the vessels in the angle are disturbed during paracentesis) may be present in FHI. Hyphema has also been reported after gonioscopy, applanation tonometry, mydriasis, and even spontaneously or—more likely—from minor trauma associated with eye rubbing.
In contrast to typical anterior uveitis, symptoms of pain, photophobia, and redness are usually absent in FHI. In Ms. McGuire’s case, we hypothesized that intraocular bleeding led to the marked increase in IOP and associated ocular pain and congestion.
Our Patient’s Course
We instilled glaucoma drops in Ms. McGuire’s right eye and noted that the IOP started trending down. We prescribed dorzolamide-timolol and brimonidine 0.2% drops and, given the presence of microhyphema, a tapering course of topical steroid eyedrops.
When Ms. McGuire returned for follow-up 3 days later, her IOP had decreased to 19 mm Hg in the right eye, and the inflammation and conjunctival injection had improved. She was happy to report that her vision was better and the eye pain and redness had resolved—and she was particularly relieved to know that she did not require an intraocular injection or laser.
___________________________
* Patient name is fictitious.
___________________________
1 Sivak-Callcott JA et al. Ophthalmology. 2001;108(10):1767-1778.
2 Jones NP. Surv Ophthalmol. 1993;37(4):253-272.
___________________________
Ms. Le is a premedical student and a recent graduate of the University of Georgia. Dr. Iyer is in private practice at Athens Retina Center, Athens, Ga., and affiliated with the Augusta University/University of Georgia Medical Partnership. Relevant financial disclosures: None
More at the Meeting
Test your diagnostic skills at these case-study symposia:
“Diagnose This” Live (Sym60). When: Saturday, Nov. 11, 2:00-4:00 p.m. Where: Room 275. Access: Free.
Grand Rounds: Cases and Experts From Across the Nation (Sym15) . When: Sunday, Nov. 12, 2:00-3:15 p.m. Where: La Nouvelle Orleans C. Access: Free.
|