By Alec Chaleff, MD, MBA, Hershel Patel, MD, MS, and Swetangi Bhaleeya, Md
Edited By: Steven J. Gedde, MD
Download PDF
Becky Brown*, a 28-year-old Caucasian woman, was doing well until about 2 weeks prior to presentation, when she felt as if she had the flu, complete with headaches and joint pain. A few days later, she noted that her eyes were red, painful, and highly sensitive to light. Her vision was also becoming blurred. Very worried about her symptoms, Ms. Brown sought medical help.
We Get a Look
Prior to evaluation by our vitreoretinal service, Ms. Brown had been treated by a primary care provider with oral methylprednisolone. By the time she came to our clinic, her arthralgia had resolved with steroid treatment, but her headaches and blurred vision persisted. She did not have any other significant ocular or medical history.
Exam findings. On presentation, Ms. Brown’s visual acuity was 20/40 in the right eye and 20/80 in the left eye. Intraocular pressure was 13 mm Hg in each eye. Her pupils were equal, round, and reactive, with no afferent pupillary defect. She had full ocular motility bilaterally.
We observed conjunctival injection in both eyes. Slit-lamp exam showed fine, diffuse keratic precipitates, as well as 2+ cells and fibrin in the anterior chamber. Trace anterior vitreous cells were also noted.
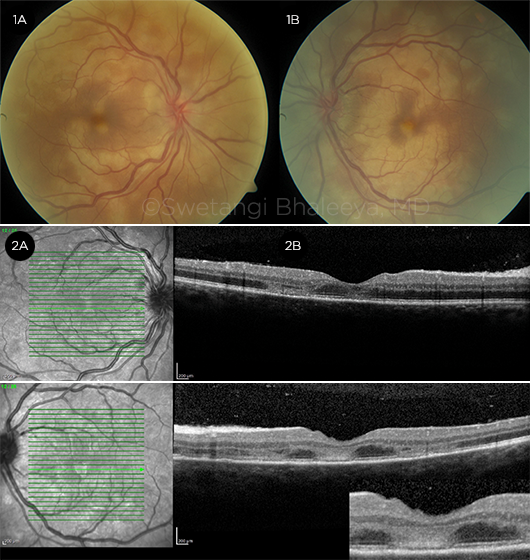
Fundus lesions. Dilated fundus exam revealed optic disc hyperemia with obscured borders. Multiple creamy, yellow-white placoid lesions were visible in the posterior pole adjacent to the superior and inferior arcades, with extension into the central macula. The lesions appeared to be at the level of deep retina and the retinal pigment epithelium (Fig. 1). The peripheral retina appeared normal.
Imaging. To augment the exam findings, we obtained the following imaging studies.
Optical coherence tomography. OCT demonstrated multiple hyperreflective discrete areas at the level of the outer nuclear layer and ellipsoid band, with attenuation of the normal retinal architecture (Fig. 2; see also Web Extra Figs. 2A-2D).
Fundus autofluorescence. FAF showed diffuse areas of hyperfluorescence corresponding to the lesions in the posterior pole and some mottled areas of hypofluorescence (see Web Extra Fig. 3).
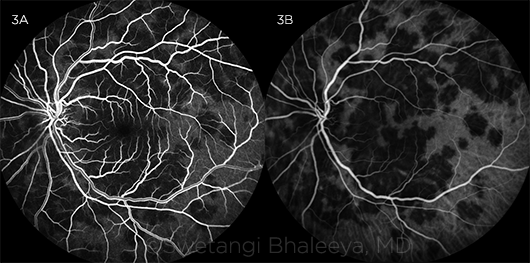
Fluorescein angiography. FA revealed hypofluorescence or blockage corresponding to areas of the lesions in the early phase, followed by hyperfluorescence in the late phase consistent with staining (Fig. 3A; see also Web Extra Fig. 4).
Indocyanine green angiography. ICGA disclosed confluent areas of hypofluorescence in the posterior pole and midperiphery in both the early and late stages. On ICGA, the lesions were found to be more numerous than what was apparent on examination or FA, especially in the midperiphery (Fig. 3B; see Web Extra Fig. 4).
 |
|
AT PRESENTATION. Fundus photos of the patient’s right (1A) and left (1B) eyes. OCT images of central macula in the right (2A) and left (2B) eyes.
|
Making the Diagnosis
Based on the history, exam, and imaging findings, our working diagnosis was acute posterior multifocal placoid pigment epitheliopathy (APMPPE). The creamy, yellow-white placoid retinal lesions we noted in Ms. Brown are characteristic funduscopic findings1; similarly, the early-phase blockage or hypofluorescence followed by diffuse late staining in the same areas are typical of APMPPE.2,3
However, her fundus appearance also raised the possibility of serpiginous choroiditis or serpiginous-like choroidopathy associated with tuberculosis. Thus, we ordered a Quantiferon-TB Gold test, which was negative, ruling out the alternative diagnosis.
 |
|
FA VS. ICGA. Left eye at presentation as seen on early-phase FA (3A) and ICGA (3B).
|
Discussion
APMPPE, one of the white dot syndromes, was first described by Gass in 1968.4 It is an acute-onset bilateral disease with characteristic findings of multiple yellow-white patches of chorioretinal inflammation in the posterior pole. The mean age of onset is 27 years, with 85% of cases occurring in patients 16 to 40 years of age.1 APMPPE is considered to be rare, and the true incidence and prevalence are unknown.1
Pathogenesis. Although the etiology of APMPPE is unclear, up to one-third of patients experience a viral prodrome before the onset of ocular symptoms. The pathogenesis is thought to be obstruction of choriocapillary lobules, possibly as an inflammatory reaction to a viral infection. Alternatively, APMPPE may be a primary disease of the retinal pigment epithelium itself.2
Systemic symptoms and complications. APMPPE is a vasculitis that is often accompanied by a viral prodrome, and systemic manifestations may include headaches, flulike symptoms, erythema nodosum, arthralgias, and myalgias.1
Neurologic symptoms such as headaches, transient aphasia, paresthesias, and muscular weakness may be associated with cerebral vasculitis and require further evaluation.1 Thomas et al. reviewed 18 patients diagnosed with APMPPE; of these, 11 patients (61%) had neurologic symptoms, with the most common being headache (9 patients).5 Stroke due to cerebral vasculitis was the most severe complication.5
Although there is no sexual predilection for APMPPE per se, the majority of cerebral vasculitis cases occur in men.6
What About Our Patient’s Headaches?
Ms. Brown’s symptoms of headaches along with ocular findings consistent with APMPPE were concerning for cerebral vasculitis, and we recommended urgent neurology consultation. She underwent extensive testing with neuroimaging, including conventional and computed tomography angiography, which did not demonstrate any evidence of cerebral vasculitis.
Further studies. Examination of her cerebrospinal fluid (CSF) showed nonspecific lymphocytic pleocytosis with normal protein and glucose levels. Polymerase chain reaction studies of the CSF found no evidence of herpes simplex virus, varicella-zoster virus, or cytomegalovirus infection.
Direct antigen testing of the CSF was also performed, and the results were negative for Haemophilus influenzae, Streptococcus pneumoniae, and Neisseria meningitidis.
In addition, the following laboratory studies were ordered as part of her neurology evaluation: rapid plasma reagin (RPR) and fluorescent treponemal antibody absorption (FTA-ABS) tests for syphilis, Quantiferon-TB Gold, and Lyme disease antibody testing. All were negative.
Treatment
APMPPE is typically a self-limited condition. No particular therapy has proved to be beneficial, although some patients with severe ocular inflammation or signs and symptoms of cerebral vasculitis are treated with systemic corticosteroids.
The chorioretinal lesions may begin to resolve in 1 to 2 weeks even without treatment.4 Visual prognosis is usually good, and patients can expect improvement in visual acuity in the long term; however, visual recovery is often incomplete.3
Our patient’s course. Ms. Brown was started on topical prednisolone acetate 6 times per day and atropine twice a day in both eyes for the anterior chamber inflammation.
Treatment with systemic corticosteroids was deferred until she completed evaluation for cerebral vasculitis, which was negative. We decided to initiate treatment with systemic steroids because of Ms. Brown’s persistent ocular inflammation and lack of visual improvement. She was treated with a course of 60 mg of oral prednisone daily for 10 days, which was then tapered weekly over 4 weeks.
Follow-up
After 1 month of treatment, Ms. Brown’s visual acuity had improved to 20/20 in the right eye and 20/40 in the left eye. Fundus exam showed pigmentary changes in area of the yellow-white placoid lesions (see Web Extra Fig. 5), which were better seen by FAF. The lesions, as seen on OCT, improved with restoration of near-normal retinal architecture (see Web Extra Fig. 6).
___________________________
*Patient name is fictitious.
___________________________
1 Kooragayala LM. http://emedicine.medscape.com/article/1225531-overview. Updated May 3, 2017. Accessed November 21, 2017.
2 American Academy of Ophthalmology. Basic and Clinical Science Course: Section 12, Retina and Vitreous. 2013-2014: pp 185-187.
3 Fiore T et al. Retina. 2009;29(7):994-1001.
4 Gass JD. Arch Ophthalmol. 1968;80(2):177-185.
5 Thomas B et al. J Ophthalmic Inflamm Infect. 2012;2(3):125-131.
6 Case D et al. J Stroke Cerebrovasc Dis. 2012;2(3):125-131.
___________________________
Dr. Chaleff is a first-year transitional resident, Dr. Patel is a second-year ophthalmology resident, and Dr. Bhaleeya is a professor of ophthalmology; all are at the University of South Florida Eye Institute, Morsani College of Medicine, in Tampa. Relevant financial disclosures: None.
Web Extra