Download PDF
Early one morning, Olivia Tibro* was getting ready for work when she noticed something unusual. While applying eye shadow, the 44-year-old discovered a bump on her right upper eyelid. The bump was not red or painful, and she decided to switch from contact lenses to eyeglasses and just observe it, hoping it would go away.
Two months later, with the bump still there, she decided to have it looked at and was referred to our oculoplastic service.
We Get a Look
Ms. Tibro’s first visit was enigmatic.
Medical history. Her medical history was significant for hyperthyroidism, which had been diagnosed eight months previously. She had undergone radioiodine ablation and was subsequently hypothyroid. The rest of her medical history was noncontributory.
Vision exam. At the time of her first visit to our clinic, she had a corrected visual acuity of 20/20 in her right eye and 20/25 in her left eye. Her pupils were equal, round, reactive to light, and without relative afferent pupillary defect. Motility was full bilaterally and orthophoric.
On slit-lamp exam, all findings in both eyes were normal.
The bump. The only abnormality noted was the palpable mass in the right lacrimal fossa; it could be pushed back into the fossa with gentle pressure.
Differential Diagnosis
The differential diagnosis for an orbital mass is broad and can be divided into infectious and noninfectious etiologies.
Infectious etiology. In the case of Ms. Tibro, infection was considered less likely given the lack of fever, local erythema, or tenderness. We therefore focused on noninfectious etiologies.
Noninfectious etiology. Given Ms.Tibro’s history of hyperthyroidism, Graves disease was high on our differential. The broad differential also included sarcoidosis and Sjögren syndrome. The acute onset also raised concern for lymphoma, pleomorphic adenoma, and other neoplasms.
Workup. In general, the initial workup for an orbital mass includes imaging techniques and serological analysis. One approach includes orbital computed tomography (CT) in axial, coronal, and parasagittal views with contrast. Magnetic resonance imaging (MRI) provides important soft tissue detail.
Serological tests that may be helpful include erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), complete blood count (CBC), antinuclear antibody (ANA), angiotensin-converting enzyme (ACE), antineutrophil cytoplasmic antibodies (cANCA), lactate dehydrogenase (LDH), and immunoglobulin (IgG4/IgG) levels.
X-ray or CT of the chest may be indicated if sarcoidosis is highly suspected.
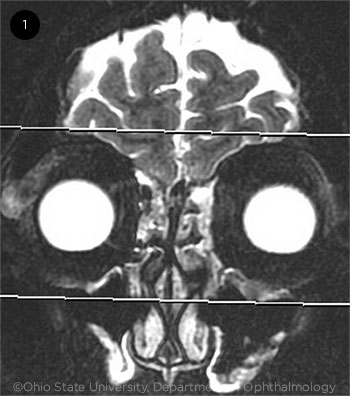 |
T2-WEIGHTED MRI ORBITS. Note the asymmetric right lacrimal gland enlargement measuring 1.0 × 2.2 cm in the axial short- and long-axis dimension. The left lacrimal gland appears normal and measures 0.4 × 1.3 cm at the same level.
|
Pinning It Down
We ordered an MRI to further characterize the lesion. The MRI revealed an enlarged right lacrimal gland with no evidence of surrounding inflammatory change or discrete nodules (Fig. 1). Other radiological findings included symmetric enlargement of the palatine tonsils and a mildly enlarged left level IIa lymph node.
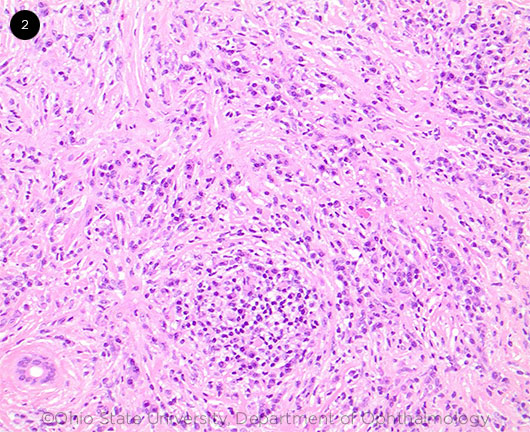
To obtain a definitive diagnosis, we biopsied the lacrimal gland and submitted the sample for histopathological evaluation. Hematoxylin and eosin (H&E) staining revealed dense lymphoid infiltrates of the glandular tissue, predominantly of small, mature lymphocytes (Fig. 2). Small germinal centers were noted with aggregates of CD138+ plasma cells. Additional features included scattered foci of fibrosis interspersed with plasma cells, rare histiocytes, and rare eosinophils.
IgG4 stain revealed several foci of more than 100 IgG4-positive plasma cells per high power field. There were focal areas where the IgG4/IgG ratio was >40%. Final tissue diagnosis of IgG4–related ocular disease (IgG4-ROD) was concluded based on plasma cell density in high-power fields and IgG4/IgG ratios.
Serological analysis revealed several important findings. Our patient had elevated ANA at 1:640, elevated IGG, elevated IGA, and elevated C3 and C4. Interestingly, serological IgG4 was within laboratory limits. Incidental thyroid studies revealed markedly decreased thyroid-stimulating hormone (TSH), elevated T3, and elevated free T4. Other analyses were within normal limits.
 |
|
H&E OF LACRIMAL TISSUE. Evaluation shows dense lymphoid infiltrates composed of predominantly small mature lymphocytes, increased aggregates, and small sheets of plasma cells.
|
About the Diagnosis
IgG4-related disease (IgG4-RD) is an idiopathic inflammatory condition associated with lesions appearing in various organs of the body.1 Although the etiology of these lesions is still unclear, IgG4-RD is characterized by tumor-like infiltrations of IgG4-positive plasma cells, typically with fibrotic abnormalities and elevated serum IgG4.2 However, normal values do not preclude IgG4-RD.1 Organs commonly affected include the pancreas, salivary glands, gallbladder, thyroid, and aorta—organ involvement that was previously not thought to be connected.
When the orbit is involved, this is termed IgG4-ROD. Painless eyelid swelling is the presenting symptom in many cases. Proptosis with or without diplopia is also common. The lacrimal gland is commonly involved, and patients present with painless, unilateral or bilateral periorbital swelling, proptosis, and erythema.3 When extraocular muscles are involved, the patient may present with pain, restrictive strabismus, or diplopia with the inferior rectus being the most commonly involved. In rare cases, inflammatory lesions have been reported to produce optic neuropathy via mass effect.3 One significant association with IgG4-ROD is the involvement of the thyroid, specifically IgG4 thyroiditis.4 Storiform-type fibrosis and obliterative phlebitis represent characteristics of IgG4 disease.4
Diagnostic criteria for IgG4-ROD disease include clinical examination with diffuse or localized masses in single or multiple organs, hematological examination with serum IgG4 concentration >135mg/dL, and histological examination with marked lymphocytic and plasma infiltration and fibrosis.3
While clinical features of progressive lesions involving multiple organs, elevated serum IgG, and imaging are helpful, tissue biopsy remains the gold standard for diagnosis.
About Treatment
To date, no trial has focused on IgG4-ROD treatment. As a result, clinicians typically employ empirical treatment.
Multiple treatment strategies. If patient symptoms are stable, close observation may be an option. Systemic corticosteroids are the treatment of choice for IgG4-ROD. No ideal steroid dosage has been established for IgG4-ROD; however, the dose used for IgG4-related pancreatitis is 0.6 mg/kg/day with a taper of 5 mg every one or two weeks.5 Although initial response to therapy is typically good, recurrence rates are high, and some physicians may choose to keep patients on a maintenance dose of 5 mg/day of prednisolone. Immunosuppressants are reserved for cases of recalcitrant disease. Options include rituximab.3 With improved understanding of the disease and the pathophysiology, IgG4-ROD specific treatment regiments may be devised and tested via randomized trials.
Ms. Tibro’s hyperthyroidism. Given the strong association of IgG4-ROD and IgG4 thyroiditis, it is interesting to consider whether her previous episodes of hyperthyroidism were related to IgG4 thyroiditis. If this were true, treatment for IgG4-RD disease, including systemic steroids, may have been more appropriate rather than radioiodine ablation. Future episodes of thyroiditis may respond to steroid therapy rather than therapy targeted toward the thyroid.
Ms. Tibro’s treatment. We referred Ms. Tibro for rheumatologic and endocrine evaluation and further management. The endocrine service is managing the hypothyroid symptoms. Rheumatology, with the biopsy and diagnosis in hand, is now following the patient and is prepared to initiate treatment should systemic symptoms develop. Ophthalmology continues to follow Ms. Tibro for her orbital symptoms.
This case highlights the role of ophthalmologists in diagnosis and evaluation of systemic disease. Biopsy and correct diagnosis in this instance significantly informed the decision-making of our internist colleagues, resulting in more targeted care.
___________________________
* Patient name is fictitious.
___________________________
1 Wallace Z et al. Surv Ophthalmol. 2012;57(1):26-33.
2 Karim F et al. Pediatr Rheumatol Online J. 2016;14:18.
3 Andrew N et al. Acta Ophthalmol. 2013;91(8):694-700.
4 Deshpande V. Head Neck Pathol. 2015;9(1):24-31.
5 Kamisawa T et al. Gut. 2009;58(11):1504-1507.
___________________________
Dr. Li, Dr. Kauh, and Mr. Hodson are all at the Wexner Medical Center of the Ohio State University in Columbus. Dr. Li is a third-year resident and Dr. Kauh is a clinical assistant professor in orbital plastic and reconstructive surgery at the Department of Ophthalmology and Visual Science; Mr. Hodson is a medical student at the College of Medicine. Financial disclosures: None.