By Emilee Dailey, MD, Samuel Thomsen, MD, Geetha Davis, MD, Ryan Davis, MD, Matthew Hirabayashi, and Vikram Ponnusamy
Edited By: Steven J. Gedde, MD
Download PDF
Jeffrey Jones,* a previously healthy 29-year-old man, presented with a 10-month history of progressive visual acuity decrease in his left eye, which started when his vision became hazy following an episode of presumed ocular migraine. Worried about the continuing decline in his vision, he came to us for help.
We Get a Look
When we saw him, Mr. Jones stated that objects lacked definition, but he said that he was not aware of any visual field loss. His previous medical history was unremarkable.
Upon examination, uncorrected visual acuity (VA) was 20/20 in the right eye and 20/50 in the left eye. Pupils were equal, round, and reactive to light, without a relative afferent pupillary defect. Anterior segment examination was normal bilaterally. Intraocular pressure (IOP) was 12 mm Hg in his right and left eyes. Confrontation visual fields were full to counting fingers in both eyes. Ocular movements were full and painless. External examination showed normal eyelids and eyelashes with hypoglobus of the left eye.
Funduscopic examination showed a normal optic nerve with normal cup-to-disc ratio bilaterally. The macula was normal in the right eye. In the left eye, we observed faint striae in the macular region, extending superiorly to the midperiphery. Blood vessels in both eyes appeared normal. Extended peripheral exam of the retina was normal in both eyes.
The classic mnemonic for recalling etiologies of chorioretinal striae is THIN RPE: T, tumor; H, hypotony; I, inflammation or idiopathic; N, neovascularization; R, retrobulbar mass; P, papilledema; E, extraocular hardware. With this list in mind—as well as the patient’s age, normal IOP, exam findings, and absence of prior ocular surgery—we developed a differential diagnosis that included choroidal tumor, posterior ocular inflammation, retrobulbar mass, and idiopathic etiology.
Further Investigations
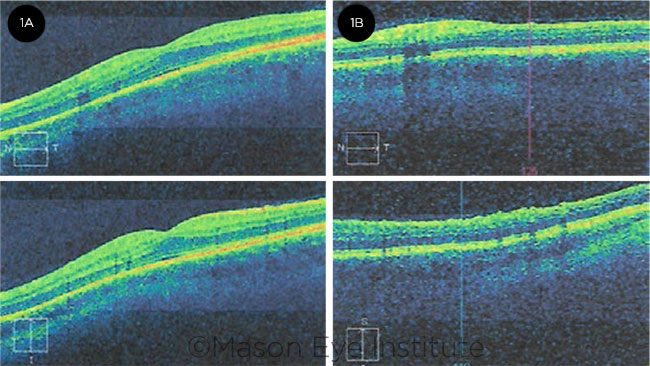
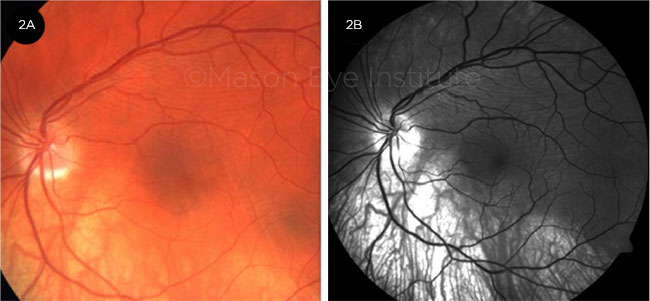
Given the patient’s blurred vision and striae, we ordered additional testing. Optical coherence tomography (OCT) images of the left eye supported our earlier funduscopic impression of macular striae superiorly (Fig. 1B). B-scan ultrasonography of the left eye showed an extraocular hyperreflective plaque in the superior temporal midperiphery. Color fundus and red-free fundus photographs of the left eye revealed retinal striae involving the central and superior macula (Fig. 2).
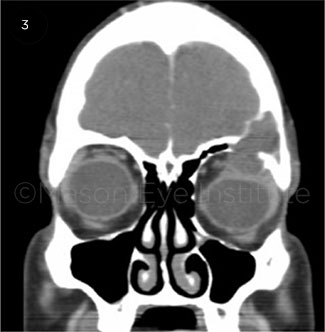
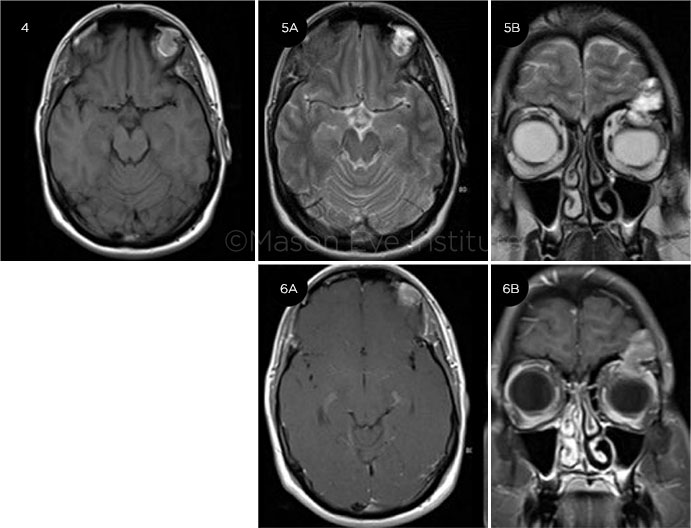
Based on these findings, we requested a computed tomography (CT) scan of the head and orbit (Fig. 3). It showed a hypodense expansive mass, measuring 1.6 × 2.9 cm, within the zygomatic process of the left frontal bone. This mass eroded through the orbital roof and extended into the orbit, causing inferior displacement and deformation of the left globe. Magnetic resonance imaging (MRI) showed a well-defined lesion that appeared hyperintense on both T1- and T2-weighted images, without significant enhancement (Figs. 4-6).
Our differential diagnosis at that time included cholesterol granuloma, mucocele, cholesteatoma, and epidermoid cyst. After further discussion between ophthalmology, otolaryngology, and neurosurgery, surgical removal was determined to be the best treatment option. Mr. Jones underwent tumor excision with orbital reconstruction. The pathology report identified the tumor as a cholesterol granuloma. At postoperative day 1 the patient felt his vision was still blurry but denied worsening. Two weeks after surgery, the patient was seen in the neurosurgery clinic and subjectively felt that his vision had improved and that he was able to read better.
 |
|
OCT. (1A) OCT image of the central macula of the right eye shows normal foveal contour. (1B) Retinal striae are visible in superior macula of the left eye.
|
 |
|
PHOTOS. (2A) Color fundus photograph and (2B) red-free fundus photograph; both images reveal retinal striae involving the central and superior macula.
|
 |
|
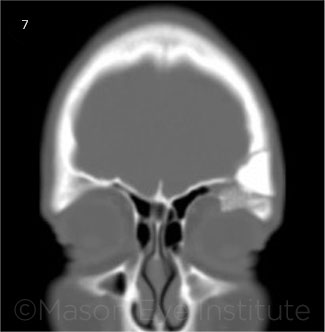
PREOP SURGERY 1. Coronal CT shows left frontal bone mass extending into the orbit with displacement and deformation of the left globe.
|
 |
|
MRI OF LEFT ORBIT. (4) Axial precontrast T1 MRI shows a focal hyperintense mass in relation to the superolateral wall. (5A) Axial precontrast T2 MRI shows a focal hyperintense mass in relation to the superolateral wall. (5B) Coronal precontrast T2 MRI shows a hyperintense mass in relation to the superolateral wall. (6A) Axial postcontrast T1 MRI shows a focal hyperintense, nonenhancing mass in relation to the superolateral wall. (6B) Coronal postcontrast T1 MRI shows a focal hyperintense, nonenhancing mass in relation to the superolateral wall.
|
Follow-up Visits
Five months after surgery, Mr. Jones returned to our ophthalmology clinic. He reported a “catching” sensation when he woke up in the morning and difficulty moving his left eye down. Uncorrected VA was 20/15 in the right eye and 20/50 in the left eye. We saw no abnormalities on exam except for mild retinal striae along the superior arcade in the left eye, consistent with the location of the excised tumor that had been indenting the globe. A CT of the head and face was ordered; it showed that the orbital roof fixation plate placed at the time of surgery was protruding into the orbit and impinging on the globe (Fig. 7). Surgery was performed and the orbital plate from the previous surgery was found to be impinging on the superior rectus and superior oblique muscles without damage to the globe. The impinging portion of the plate was removed, leaving a small defect in the roof of the orbit that was considered insignificant.
Mr. Jones was seen in the ophthalmology clinic two days postoperatively. He no longer felt the “catching” sensation and was able to move his left eye without difficulty. On dilated fundus exam, mild retinal striae were still present, and VA of the left eye was 20/50. The patient was scheduled to return in six months but was lost to follow-up.
Four years have passed since the revision. We contacted him recently, and he reported a VA of 20/30 in his left eye during a recent eye exam.
 |
|
PREOP SURGERY 2. Coronal CT shows the fixation plate extending into the bony orbit and impinging on the superior surface of the left globe.
|
Discussion
Cholesterol granuloma is a rare diagnosis that has been reported in several anatomic locations. The most common of these sites are the middle ear, mastoid antrum, and petrous apex.1 Less frequent locations include the frontal bone, zygoma, paranasal sinuses, breast, peritoneum, testes, and lung. When a cholesterol granuloma forms in the orbital region, it occurs most often within the lacrimal region of the frontal bone. It is unknown why this region is most commonly affected.
Pathogenesis. The etiology of orbital cholesterol granulomas is currently unknown, but several hypotheses have been proposed. The most-accepted hypothesis is that an unabsorbed hematoma from an episode of mucosal bleeding in the frontal sinus leads to deposition of cholesterol crystals, causing a foreign body chronic inflammatory response.2 Although the inciting event is unclear, trauma could be a trigger.
Imaging. Both CT and MRI are helpful in diagnosing a cholesterol granuloma. A noncalcifying lesion that is isodense with brain, round with a smooth outline, and located in the superolateral bony orbit is typically seen on CT. On MRI, cholesterol granulomas show bright signal intensity on both T1- and T2-weighted images due to the presence of hemoglobin breakdown products around the cholesterol crystals.3 Both of these findings were used to describe the mass in our case, and even before surgical removal, cholesterol granuloma was considered to be the most likely diagnosis.
Treatment/histology. The definitive treatment for a cholesterol granuloma is drainage and total removal of the granulomatous tissue. Although recurrence is rare, curettage of any residual granulomatous material adhering to the bone and periosteum is necessary to further reduce the chance of recurrence.4 Once removed, the lesion should be sent to pathology for a histologic diagnosis, which classically shows foreign body giant cells surrounding cholesterol clefts, chronic inflammatory infiltrate, and hemorrhagic products—all of which are characteristics of a cholesterol granuloma.
Patient’s course. When Mr. Jones was seen in our ophthalmology clinic after his final surgery, we assumed that his vision had not improved because of the continued striae in the presence of the implant. When we communicated with him four years later, he stated that the VA in his left eye was 20/30. Based on that information, we speculated that the striae resolved after revision surgery, resulting in an improvement in vision. However, it remains unclear why his vision did not improve to 20/20 following revision. Unfortunately, we have no records of the patient’s baseline VA before presentation, which might have helped explain his outcome.
___________________________
* Patient name is fictitious.
___________________________
1 Royer MC, Pensak ML. Curr Opin Otolaryngol Head Neck Surg. 2007;15(5):319-322.
2 Selva D et al. Clin Exp Ophthalmol. 2003;31(1):78-82.
3 Dubrulle F et al. Radiology. 2006;238(2):604-610.
4 Hoa M et al. J Laryngol Otol. 2013;127(4):339-348.
___________________________
Dr. Dailey is a PGY1 resident who will begin ophthalmology residency at the University of Alabama at Birmingham, Callahan Eye Hospital, in July 2019. Dr. Thomsen is a PGY4 ophthalmology resident, and Dr. G. Davis is the residency program director and an assistant professor of clinical ophthalmology; both are at the Mason Eye Institute at the University of Missouri Hospital, Columbia. Dr. R. Davis is an assistant professor of clinical radiology at the University of Missouri Hospital in Columbia. Mr. Hirabayashi and Mr. Ponnusamy are medical students at the University of Missouri School of Medicine in Columbia. Financial disclosures: None.