By Alexander F. Vu, MD, and Roma P. Patel, MD, MBA
Edited By: Ingrid U. Scott, MD, MPH
Download PDF
Eddie Grover,* a 72-year-old veteran, was experiencing new onset throbbing headaches centered around his blind right eye. Twenty-five years earlier, during a car accident, he had suffered severe trauma to his right eye after being ejected from his vehicle. Despite multiple surgeries to reconstruct the orbit and eyelid position, the trauma to his optic nerve ultimately cost him the vision in his right eye.
He had learned to live with one blind eye and, for many years, experienced no significant eye pain or discomfort—but that had suddenly changed.
The Presentation
Mr. Grover walked into our ophthalmology clinic at the Veterans Affairs (VA) hospital after two weeks of ongoing pain and redness in his right eye, as well as headache. He described a dull achiness that was centered on and radiated from his right eye. Initially, this was intermittent, but it had slowly worsened and became constant. He had attempted to wait it out, and then tried lubricating the eye with artificial tears and erythromycin ointment, which he had from a prior case of conjunctivitis. The pain failed to improve. He also reported new photophobia of the left eye.
History. Mr. Grover had undergone cataract surgery in his left eye years ago but had no other major ocular history besides the trauma to his right eye. During clinic visits over the prior two years, intraocular pressure (IOP) measurements had been elevated to 50-65 mm Hg in the right eye, but, given that the eye was comfortable, he was never treated for this. He said that he had not had any recent trauma, nausea, vomiting, or changes in vision other than the two-week history of photophobia in the left eye.
His only chronic health issue, other than hypertension, was chronic shoulder and back pain from the car accident.
Initial suspicions. On history alone, we initially suspected an acute spike in IOP. We were also considering an inflammatory process (such as sympathetic ophthalmia, especially given the patient’s history of ocular trauma), an ocular surface issue (given possible exposure related to multiple lid reconstructive procedures), and the possibility of onset of a phthisic globe.
Exam. On exam, visual acuity was no light perception in the right eye and 20/25 in the left eye. His pupils were irregular at 5 mm on the right with a dense relative afferent pupillary defect, and 4 mm and reactive on the left—all unchanged from previous visits. His IOP was 58 mm Hg in the right eye and 10 mm Hg in the left. Slit-lamp biomicroscopy revealed dense scarring of the nasal cornea of the right eye that was unchanged from his prior exam.
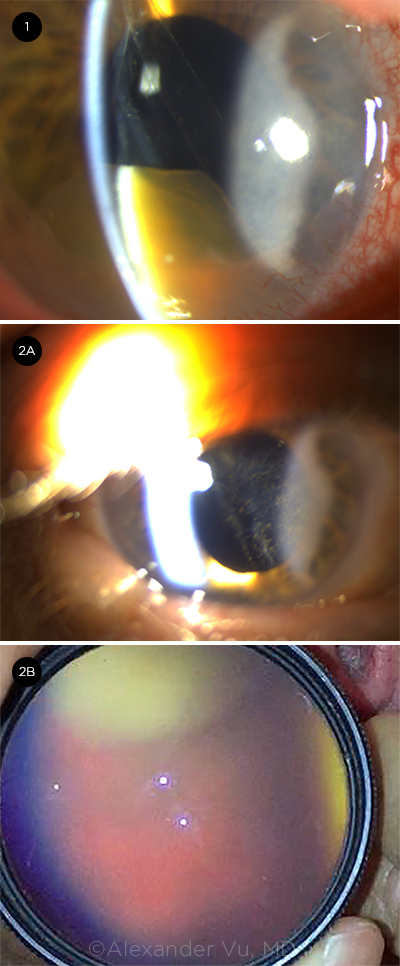
A new finding. The exam was most notable for something we saw in the right eye—a large dense hexagonal brown mass in the anterior chamber consistent with a dislocated crystalline lens nucleus (Fig. 1). It was located inferiorly with frank corneal touch, associated with dense cell and flare suggesting a secondary uveitis. The nucleus appeared to be tethered by a clear membrane consistent with a torn lens capsule that extended from behind the pupil. With this finding, we diagnosed lens luxation into the anterior chamber.
Documentation by previous eye providers had labeled Mr. Grover as aphakic in the right eye, suggesting that the lens dislocation happened years ago or around the time of the accident, with the nucleus initially falling into and resting in the vitreous cavity.
Exam of the left eye was unremarkable except for mild ocular surface staining.
Likely cause. We pondered what would cause anterior lens dislocation this late after trauma. On further questioning, Mr. Grover explained that he had started hanging upside down with an inversion table over the last couple of months to alleviate his chronic back pain. He often did it with dim lighting to help him relax.
 |
|
BEFORE AND AFTER TREATMENT. (1) When we first examined Mr. Grover, his right eye had a dense mass that could be seen in the inferior angle of the anterior chamber. The mass was suspended by a thin capsular membrane. Later, after the lens had been reposited into the posterior chamber, (2A) slit lamp showed the anterior chamber without the mass, and (2B) indirect biomicroscopy ophthalmoscopy with a 20-D lens showed the crystalline lens behind the iris.
|
Discussion
Lens luxation (or dislocation) can be associated with various processes that can weaken or damage the zonular-capsular complex.
Causes. Lens luxation most commonly results from trauma, as in Mr. Grover’s case. It can also occur secondary to connective tissue disease (e.g., Marfan syndrome, homocystinuria, and Weill Marchesani syndrome),1 pseudoexfoliation, myopia, or inflammation.2
Lens in the anterior chamber. Lens luxation into the anterior chamber is rare compared with lens luxation into the posterior segment. In sighted eyes, luxation into the anterior chamber is generally considered an emergency, as crystalline lenses in the anterior chamber can cause corneal decompensation, inflammation, and severe glaucoma.3,4
Management. Management is surgical, and it often requires anterior vitrectomy and lensectomy. Since the advent of phacoemulsification, ophthalmologists have been able to achieve successful management even with small incisions. Viscodissection can aid in separating the crystalline lens from the cornea in cases with lens-corneal touch. Implantation of an IOL during the initial surgery or in a staged manner can be considered, though the implant may need to be sutured if the capsular scaffold is compromised.1
A case has also been made for more conservative management, using topical agents and supine posturing to reposit the lens behind the iris. This can allow for a pars plana approach, which may be able to prevent further damage to an already stressed corneal endothelium.5 However, because anterior lens luxation is rare, there aren’t sufficient studies to determine whether this would lead to better or worse visual outcomes.
Morning Rounds: 2020 in Review
Tackle this year’s medical mysteries.
- The Case of the Eye Shadow Bump The 48-year-old noticed a bump on her eyelid while applying makeup. It wasn’t red or painful, but it also wouldn’t go away (January EyeNet).
- “Doctor, My Son’s Eye Is Swollen!” The 4-year-old had a mild cough and intermittent ear pain but otherwise seemed healthy. However, when he also developed swelling around his right eye, his parents took him to see a pediatrician. Before long, he was in the emergency department (March EyeNet).
- A Case of Corneal Crystals The 75-year-old wondered if cataracts were to blame for her deteriorating vision and increased glare when driving at night (April EyeNet).
- The Case of a Teen With Nyctalopia The 15-year-old, with a history of cystic fibrosis, had been experiencing progressive decreased vision and difficulty with night vision for three years (May EyeNet).
- The Case of Retinal Spots With Blurred Vision The 75-year-old was referred to us with a diagnosis of presumed ocular histoplasmosis syndrome (June EyeNet).
- The Case of the Droopy Eyelid and Frozen Globe One month after being diagnosed with herpes zoster ophthalmicus, the 84-year-old was suffering intractable pain (August EyeNet).
- The Case of a Bulging Eye and Double Vision His right eye, which had started “bulging” a month previously, had ductional deficits in all directions (September EyeNet).
- “My Son Was Wrestling With His Brothers—and Now His Eye Is Swollen!” An active 5-year-old enjoyed wrestling with his older brothers. When his parents noticed that his right eye looked swollen, they initially assumed that it had occurred during horseplay (October EyeNet).
- First an Nd:YAG Capsulotomy, Then an Inflamed Eye The capsulotomy didn’t halt the 73-year-old’s decline in visual acuity (November EyeNet).
|
Hmm, Can We Push It Back?
In Mr. Grover’s case, given his lack of visual function in the affected eye, we opted to try a conservative approach. We decided that we would resort to surgery only if conservative measures failed to improve his symptoms.
Our conservative approach. We administered topical mydriatic eyedrops to facilitate repositioning of the lens behind the iris. We had the patient perform a multitude of head and body maneuvers, with the goal of moving the lens away from the cornea. Neither supine nor inverted head positioning was able to dislodge the lens from the inferior angle. However, with the use of a topical anesthetic and repeated tapping, rolling, and manipulation with a cotton-tipped applicator, we were able to press the lens through the dilated pupil while Mr. Grover lay supine (Fig. 2). The inflammation was controlled with an extended course of topical steroids. The IOP in the right eye remained around 50 mm Hg throughout six months of follow-up, but this was his baseline and there was no associated pain.
After full recovery from the uveitis and repositioning of the lens, the patient wanted to resume hanging upside down with an inversion table in order to relieve his chronic back pain. He was cautioned to use the inversion table in a brightly lit room and was provided a prescription of pilocarpine to use on an as-needed basis prior to these exercises.
___________________________
*Patient name is fictitious.
___________________________
1 Chung JL et al. Korean J Ophthalmol. 2007;21(4):255-260.
2 Soh YQ et al. EyeNet. 2017;21(10):37-39.
3 Choi DY et al. J Cataract Refract Surg. 2004;30(3):718-721.
4 Kawashima M et al. Cornea. 2007;26(4):487-489.
5 Shah AN, O’Brart DP. Clin Exp Optom. 2011;94(4):380-382.
___________________________
Dr. Vu is a third-year ophthalmology resident at the University of California Davis Eye Center. Dr. Patel is assistant professor at UC Davis Eye Center and chief of Eye Care at Sacramento VA. Financial disclosures: None.