Download PDF
A Simple Hand Magnifier for Teleophthalmology
Teleophthalmology has never been more important than it is now. Although restrictions, such as social distancing, pose challenges, they have provided an opportunity for innovation.
In teleophthalmology, one challenge is obtaining clinically useful photos from homebound patients. With a smartphone or tablet and a hand magnifier (e.g., a reading aid or magnifying glass), patients can take magnified photos with ease.
Most phone cameras have autofocus and high-resolution capture allowing for sharp images. However, low magnification may limit the provider’s ability to provide a proper diagnosis. By placing the simple hand magnifier immediately adjacent to the camera and using the autofocus, patients can take clinically useful images.
These instructions detail the simplicity of the technique:
- Instruct patient to open the camera function of phone or tablet.
- Place the simple hand magnifier directly against camera.
- Use autofocus or tap image on screen to focus.
- Move the phone as close as possible while maintaining focus.
- Take the photo.
This technique is easiest with assistance but can be accomplished in selfie mode if circumstances require.
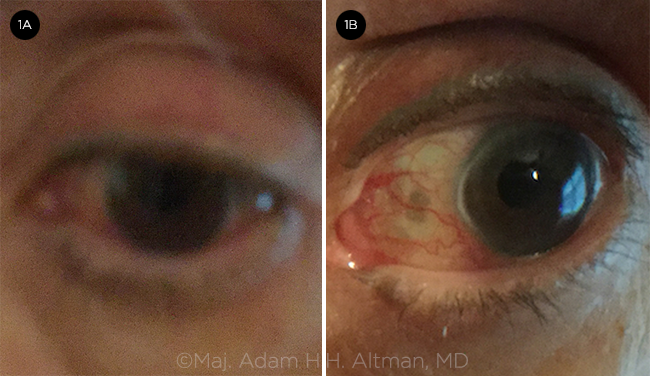 |
COMPARISON. (1A) Without and (1B) with a hand magnifier.
|
The images from the patient pictured above (Figs. 1A, 1B) demonstrate clarity of the ocular structures, which allowed for a successful teleophthalmic encounter. The patient’s husband used an iPad Air2. No additional instruction was given other than the above steps. For optimal results:
- Ask the patient to take many photos from different angles to increase the likelihood of obtaining useful images.
- Ensure adequate lighting. Instruct patient to face light source (broad, diffuse light is best) and avoid casting shadows from camera.
- Turn the brightness all the way up on the phone or computer for optimal viewing.
Simple hand magnifiers can provide sharp, magnified images that allow for accurate triage of remote patients.
Maj. Adam H.H. Altman, MD, and Maj. Gary L. Legault, MD
San Antonio Uniformed Services Health Education
Consortium, Joint Base
San Antonio
NOTE: The views expressed in this letter are those of the authors and do not necessarily reflect the official policy or position of the U.S. Departments of the Navy, Army, or Air Force; the U.S. Department of Defense; or the U.S. government.
COVID-19: A Young Ophthalmologist’s Perspective
As a young ophthalmologist (YO), I began my career mired in doubts. And just as I had started to build a practice and finally gain confidence in my skills, COVID-19 happened. In talking to my peers, I realize that most of us in the early stages of our careers are going through similar experiences.
Like my colleagues, I worry about the innumerable patients with chronic vision-threatening issues who are falling through the cracks. I think about my patients who cannot come for follow-up due to age, concurrent illnesses, and lack of social support. Many are not adept at technology and cannot participate in telemedicine. For some, I cannot help but worry about their survival prospects. I am also concerned about the safety of my staff, family, and self. Due to fear and anxiety of exposure, we are having to make the difficult decision to isolate away from aging parents, young children, and spouses. All of this is taking an emotional toll.
In addition to this, most YOs are challenged with student loans and with providing financially for young families. Those of us in employed positions are being furloughed or taking reduced pay; those on productivity-based partnership tracks may no longer be eligible to transition from associate to partner; and those who have started their own practices are struggling to stay afloat. For those in training, surgical exposure has been significantly decreased.
However, despite the uncertainty and doubt, my most overwhelming emotion is that of gratitude: gratitude for the selflessness of our colleagues on the frontlines, for health and family, for my mentors, for our Academy, and for our profession. I am privileged to have the needed skills, and I am honored to restore vision and preserve the gift of sight. We will emerge from this more thoughtful and empathetic. And for that I am grateful.
Shruti Aggarwal, MD
Katzen Eye Group
Baltimore
Emergency Care: A Fraying Social Contract
During the COVID-19 outbreak, many ophthalmologists have been delivering emergency eye care in their offices or by telemedicine. This has helped ease the strain on emergency departments (EDs).
This focus on emergency ophthalmic care brings to the fore the economic realities of rendering emergency care out of our offices and clinics. (For past discussion of this issue, see “Who’s On Call? Emergency Care Crisis Looms,” Clinical Update, December, and “Rethinking Call Duty,” Letters, March).
In the past, we accepted these emergencies at our offices as part of a social contract: We understood that patients would get better care seeing us directly at a reduced cost to society versus care in an ED. However, even prior to the COVID-19 pandemic, this social contract was being frayed by reductions in reimbursement, increased difficulty collecting on claims, and an ever-heavier regulatory burden. An emergency visit is a “known unknown.” For a nonmultispecialty ophthalmology office, a time-intensive secondary referral is sometimes required. Furthermore, because the more routine eye emergencies are seen at urgent care centers, ophthalmologists tend to get the cases that are more complex and time-consuming.
The specter of COVID-19 will slow our workflows given the need for social distancing, wearing of protective gear, and cleaning of surfaces. This exacerbates the economic strain of adding an emergency encounter to the schedule.
From an economic point of view, an emergency encounter can take twice as long as a conventional visit (even with telemedicine) and involves more risk and complexity. Therefore, reimbursement for it should be at least twice as much as for a comprehensive new patient exam. After all, eye care services rendered by ED physicians wind up costing many times more than the care rendered in an ophthalmology office for the same presenting complaint—when supply and facility costs, expensive testing such as CT scans, and out-of-network billing are taken into account. (There have been some efforts to reduce surprise out-of-network charges.)
We need to find ways to allow our specialty to accept patients with emergencies in a way that makes economic sense. These visits could be differentiated from nonemergency care with special coding and reimbursement. We should work with CMS and insurance companies to achieve these changes.
Lawrence Stone, MD
Chicago