This article is from April 2012 and may contain outdated material.
Download PDF
For cataract patients with regular astigmatism, toric IOLs provide the potential for better uncorrected visual acuity than they have ever had. For surgeons, though, toric lenses pose a challenge because even small errors in an IOL’s position may significantly affect the patient’s uncorrected visual acuity—more so than they would with a spherical IOL. “For every one degree of error in a toric IOL’s rotational alignment, there is a 3.3 percent decrease in the correction of astigmatism. So if a toric IOL is misaligned by 10 degrees, that’s a 33 percent loss of the toric correction,” said Warren E. Hill, MD, medical director of East Valley Ophthalmology in Mesa, Ariz. “And if the toric IOL is misaligned by 30 degrees, it’s as though you put in a spherical IOL—the IOL isn’t correcting any astigmatism.”
Positioning errors have the largest impact at higher cylinder powers, which became available in the United States last spring for AcrySof (Alcon) toric IOLs, said John P. Berdahl, MD, a cataract and refractive surgeon in Sioux Falls, S.D. “Now that the -T8 and -T9 AcrySof torics are coming online, it’s more important than ever for us to talk about this,” he said. “Those lenses have to be perfectly aligned, or you will have a lot of residual astigmatism in the eye.”
Experienced toric IOL surgeons say that today’s tools and techniques often enable them to keep the disappointments to a minimum. However, when a patient’s residual astigmatism is unexpectedly high, there are several postsurgical solutions to help remedy the situation.
What Went Wrong?
It is important to understand the reasons for the residual astigmatism before trying to correct it.
Top four errors. Dr. Hill said that the errors generally fall into one of four categories:
- Preop measurement errors
- Incorrect marking of reference points on the cornea
- Incorrect placement of the IOL
- Failure to take into account the impact of surgically induced astigmatism.
Other causes. Dr. Berdahl said residual astigmatism can also be caused by incorrect IOL power at the corneal plane (reported with the AcrySof toric), 1 by the patient’s posterior corneal curvature, or by measurement variability. “You might have lined up the IOL axis exactly where you intended to put it, but that didn’t turn out to be the right place because K readings, for instance, don’t always agree,” he said. “The topography might not line up exactly with the K from a manual keratometer or with the K from an optical biometer.”
Intangibles. Finally, there are the intangible factors that can’t always be controlled, said Y. Ralph Chu, MD, a cataract and refractive surgeon in Bloomington, Minn. “There’s an art to implanting a toric IOL. It’s an inexact science. Sometimes, no matter how good your mathematical model, you’re still going to have residual astigmatism.” Dr. Chu is an adjunct associate professor of ophthalmology at the University of Minnesota, Minneapolis.
 |
To rotate or not. After toric IOL implantation, a surgeon can use the Toric Results Analyzer ( www.astigmatismfix.com) to determine whether going back into the eye and rotating the lens would decrease residual astigmatism.
|
Option 1: Rotate the IOL
Regardless of the reason for the residual astigmatism, the first step in deciding how to resolve it is using the slit lamp to evaluate the IOL’s position, Dr. Chu said. “I look at the position in relation to my targeted axis. If it looks like there has been a significant lens rotation, then I go in and rotate it into the correct orientation,” he said.
But the physician should first confirm that a second surgery is justified by the potential visual gain, Dr. Berdahl said. “I want to treat at least 0.5 D of astigmatism by rotating the lens. I would also want this to get the patient’s astigmatism down to below 0.5 D,” he said.
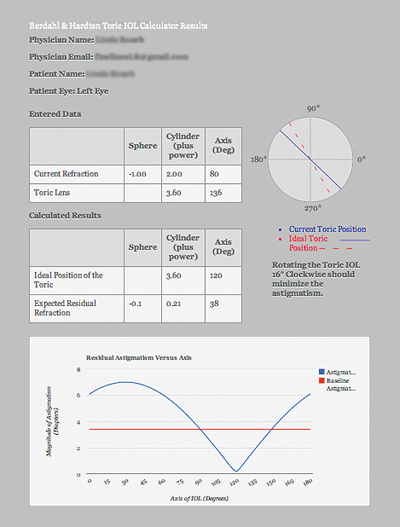
An online calculator helps. Instead of doing their own vector analysis, surgeons can turn to the Toric Results Analyzer, a Web-based tool created by Dr. Berdahl and veteran cataract and refractive surgeon, David R. Hardten, MD, of Minneapolis. (Visit www.astigmatismfix.com.)
The clinician enters three measurements (current manifest refraction, astigmatic magnitude and IOL axis) into an online form, then clicks “Calculate.” The resulting diagram shows the IOL’s target and current locations relative to the axis of astigmatism; the accompanying charts quantify the refractive effect of rotating the lens.
“If the calculator says that there is no way to get rid of a significant amount of the astigmatism by rotating the lens, or if it says that there is no way it will reduce the residual astigmatism to 0.5 D or lower, then you need to reduce the astigmatism in some other way,” Dr. Berdahl said. “You need to exchange the lens or to reshape the cornea with a laser or incisional procedure.”
Rotate early. If rotation is indicated, or if the patient needs an IOL with a different refractive power, the surgeon should act promptly, before fibrotic healing can interfere with the procedure. While Drs. Hill and Chu indicate that the rotation can take place as early as one or two weeks after surgery, Dr. Berdahl advises waiting slightly longer: “Ideally, within the first month. But not before two weeks, to be sure that the eye’s refraction has settled down after surgery.” But all three agree that, depending on how fast the patient heals, the rotation should be performed by three to six months after the initial surgery.
Surgically Induced Astigmatism
Although residual astigmatism often reflects improper alignment, it might also mean the surgeon should have compensated for surgically induced astigmatism (SIA) from the phaco incisions when placing the toric lens, said Dr. Chu. “You must know the best place to put your incision, relative to the cornea’s steepest meridian.”
Dr. Hill said, “Physicians call me and say, ‘I don’t know what’s wrong. I can’t get these toric IOLs to work.’ I tell them that they need to know what their SIA numbers are in the real world.” He urges toric IOL surgeons to learn their personal SIA number and to use it to achieve better results. He built a free tool, the SIA Calculator, to do the math and posted a Web-based version at SIA-calculator.com and a downloadable version at doctor-hill.com/physicians/download.htm. A clinical study published last year found that SIA can significantly impact the success of correcting low amounts of preop astigmatism with a toric IOL.1
1 Ernest P, Potvin R. J Cataract Refract Surg. 2011;37(4):727-732.
|
Option 2: Excimer Laser Ablation
The next best treatment is laser refractive surgery, Dr. Berdahl and Dr. Chu said. “I typically choose LASIK or PRK because I think laser procedures are more predictable than incisional surgery,” said Dr. Berdahl. His patients can choose between LASIK and PRK, whichever they prefer, with one exception. “For older patients [65 and up], I often choose PRK because they are more likely to have anterior basement membrane dystrophy, which would make LASIK less predictable,” he said.
Dr. Chu prefers PRK because it limits the surgical impact to a zone along the steepest meridian. “It’s a surface ablation, but typically over a very small area. You’re just enhancing the optical properties of the eye,” he said.
Option 3: Incisional Treatment
Limbal relaxing incisions (LRIs) remain these surgeons’ last surgical choice for treating residual astigmatism.
Drs. Chu and Berdahl said they are concerned about unpredictable refractive effects from the incisions (as well as from incisions for an alternative incisional procedure, anterior keratectomy). However, said Dr. Chu, “if the lens is in a pretty good position, and if the patient is comfortable with the idea of incisions, then I think you could use LRIs.”
Greater LRI accuracy? Dr. Hill said he sometimes uses LRIs to reduce small amounts of residual astigmatic error. But he prefers to do a lens exchange and/or rotate the lens to the correct meridian for larger amounts.
He said the predictability of the LRI procedure has been improved by pachymetry software that calculates the depth and placement of incisions based on patient age, intraocular pressure and corneal rigidity.2 The surgeon must use an adjustable diamond blade with micrometer depth markings, Dr. Hill noted.
LRI calculator. Cataract surgeons interested in learning more about how to use LRIs can consult a Web-based planning tool that operates similarly to Dr. Hill’s SIA Calculator (mentioned in the box, above). The LRI Calculator performs mathematical vector analysis of topography or keratometry data the surgeon provides. The site produces an individualized diagram showing where to place incisions; it can be printed out for reference in the operating room. The website also includes an extensive “LRI Clinical Guide,” step-by-step procedural instructions and surgical pearls. (Visit www.LRICalculator.com, from AMO.)
Option 4: Glasses or Contacts
It is a truism of refractive surgery—and now of refractive cataract surgery—that patients who pay extra for a premium procedure will resist the idea of wearing eyeglasses or contact lenses after surgery. Consequently, toric IOL surgeons advise making this a last-ditch option.
Nonetheless, in a large randomized, multicenter clinical trial of the AcrySof toric IOL (n = 517), 39.1 percent of the toric IOL recipients reported some degree of spectacle dependence for distance vision at six months postop. 3 Dr. Chu advises emphasizing this possible outcome during the informed consent process. “It is important to set the right expectations for the patient before surgery. I never tell patients that we’re going to get you to zero astigmatism,” he said.
Not only are toric IOLs imperfect, but so are the ophthalmologists who implant them, added Dr. Hill. “If someone says they don’t have any problems with their astigmatic corrections, they’re being arrogant,” he said. “None of us as surgeons can get it right every time. You always have to have Plan B.”
___________________________
1 Goggin M et al. Arch Ophthalmol. 2011;129(8):1004-1008.
2 Micro Medical Devices, Calabasas, Calif. “Accurate LRI Calculator” for the PalmScan P2000 and AP2000 pachymeters. www.micromedinc.com/lri-package-2.html.
3 Holland E et al. Ophthalmology. 2010;117(11):2104-2111.
___________________________
Dr. Berdahl is a consultant to Alcon. Dr. Chu is a consultant to AMO and Bausch + Lomb. Dr. Hill is a consultant to Alcon, Carl Zeiss Meditec and Haag-Streit.
Better Keratometry Matters
Pay attention to your keratometry, Dr. Hill advises. “If you are charging patients extra for a premium IOL, you have to be sure that the preoperative measurements are correct. Automating and delegating will generally produce less than optimal results,” he said.
If manual keratometry is used, he recommends that the surgeon—rather than the technician—do the preoperative measurements. Manual keratometry allows the physician to take as much time as necessary to confidently locate the astigmatic steep and flat meridians, he said.
He also cautions against planning a toric IOL surgery based solely on the autokeratometry feature of the IOLMaster (Carl Zeiss Meditec), the most widely used optical biometer.
“For calculating the spherical power of a toric IOL, this instrument works quite well,” Dr. Hill said. But the IOLMaster lacks the overall precision required to consistently determine the steep and the flat meridians because it has just six optical sampling points on the cornea, spaced 60 degrees apart, he said. “If the steep meridian lines up with 0, 60, 150 and 180 degrees, IOLMaster may work well. But if the steep meridian is at 30, 90 or 120 degrees, the machine has to do a lot of interpolation,” Dr. Hill said.
However, Drs. Hill, Berdahl and Chu said that their recent experiences with another optical biometer, Haag-Streit’s Lenstar LS 900, suggest that this instrument does a better job, with two rings of 16 measurement points, spaced 22.5 degrees apart. The steep and the flat meridians, as well as the power difference between them, are derived from a greater number of measurement points and are measured twice.
Simultaneously, the Lenstar uses optical low-coherence reflectometry to measure corneal curvature; corneal, lens and retinal thickness; pupil and white-to-white corneal width; axial length; aqueous and anterior chamber depth; and eccentricity of the visual axis.
Researchers comparing Lenstar to other measuring instruments have reported favorable results.1,2
1 Hill W et al. J Cataract Refract Surg. 2011;37(12):2181-2187.
2 Shammas HJ, Hoffer KJ. Am J Ophthalmol. 2012;153(1):55-61.e2.
|