Blink
Toxoplasma Chorioretinitis
By Patrick R. Oellers, MD, Massachusetts Eye and Ear, Harvard Medical School, Boston; and Prithvi Mruthyunjaya, MD, Byers Eye Institute, Stanford University, Palo Alto, Calif.
Photo by Ryan Imperio, CRA, OCT-C, and Sean Grout, Duke Eye Center, Durham, N.C.
Download PDF
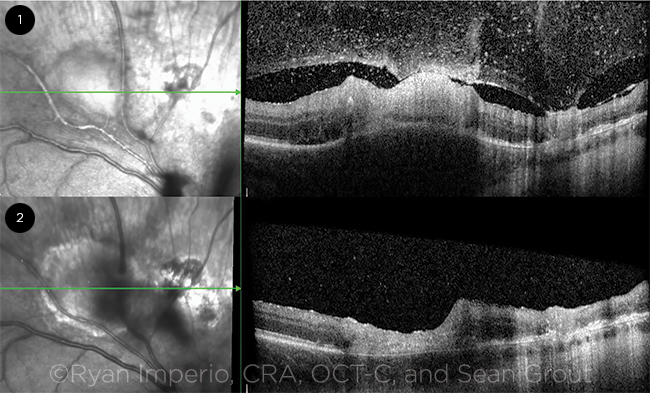
A man in his 30s presented with floaters and pain in the right eye. Examination revealed keratic precipitates (KP), 1 to 2+ anterior segment and vitreous cells, Kyrieleis’ vasculitis, and active chorioretinitis with overlying vitreous stranding next to an old, partially pigmented chorioretinal scar in the posterior pole. Corresponding enhanced-depth spectral domain optical coherence tomography (OCT) showed stippled vitreous hyperreflectivity and hyperreflective thickening of the retina with disorganization of all layers atop choroidal thickening in the area of active infection, adjacent to an area of retinal thinning with associated dense vitreoretinal adhesion (Fig. 1). Systemic workup revealed positive toxoplasmosis IgG and IgM titers. A diagnosis of recurrent toxoplasmosis chorioretinitis was made, and the patient was treated with oral sulfamethoxazole-trimethoprim and topical prednisolone acetate drops. After the patient completed a 6-week antibiotic course, examination revealed resolution of active inflammation and scar formation. Corresponding OCT demonstrated retinal thinning with loss of retinal architecture (Fig. 2).
| BLINK SUBMISSIONS: Send us your ophthalmic image and its explanation in 150-250 words. E-mail to eyenet@aao.org, fax to 415-561-8575, or mail to EyeNet Magazine, 655 Beach Street, San Francisco, CA 94109. Please note that EyeNet reserves the right to edit Blink submissions. |