By Jeff H. Pettey, MD, with Usiwoma E. Abugo, MD, O’Rese J. Knight, MD, and Grace Sun, MD
Download PDF
Considering the profound impact of the COVID-19 pandemic on trainees, it is important to take a closer look at some of the very real effects on students, residents, and fellows that will last into the future. That is the goal of this MD Roundtable, hosted in July by Jeff H. Pettey, MD, of the John A. Moran Eye Center at the University of Utah in Salt Lake City. He was joined by Usiwoma E. Abugo, MD, of Virginia Eye Consultants and Eastern Virginia Medical School in Norfolk, as well as O’Rese J. Knight, MD, of the University of North Carolina at Chapel Hill, and Grace Sun, MD, of Weill Cornell Medical College in Manhattan.
This month, Part 1 of the discussion covers the direct effects of the pandemic on programs, as well as innovative ways of adapting. Next month, Part 2 covers clinical rotations at medical schools, fellowships and job prospects, and silver linings.
Immediate Effects
Dr. Pettey: The COVID-19 pandemic has affected all of us in many unanticipated ways. Trainees have been affected in particularly unique ways, which may differ for students, residents, and fellows. Starting with Dr. Sun, what were the immediate effects of COVID-19 on your trainees and training programs?
Dr. Sun: In my role as residency program director at Weill Cornell, we were in the U.S. epicenter of the pandemic; the bravery and courage of the residents in our program were nothing short of inspirational.
We have a group of nine residents in training, and many of them had to be redeployed to the hospital to work on the medicine floors with COVID-19 patients. In fact, all the New York City downstate programs had their residents redeployed. They no longer were in the ophthalmology clinics but rather were in the emergency room, the ICU, and on the wards. They were no longer doing cataract surgeries; they were checking oxygen saturation levels instead. They really stretched, and I couldn’t have been more impressed with their selflessness.
Dr. Knight: In terms of redeployment, at the University of North Carolina we were largely spared. One of our residents participated in planning for potential redeployment, if it became necessary, but our caseload didn’t actually rise to that level.
With regard to clinical training, our residents spend three months in their second year and six months of their third year at the Fayetteville VA Health Care Center. One resident has been stationed at the VA for much of the pandemic. The VA operating rooms are essentially shut down, except for urgent and emergent surgeries, and clinics have been significantly curtailed. We’re working now to adjust some of our rotation assignments to ensure that she and her classmates have a strong clinical and surgical training experience in spite of the pandemic.
Another aspect of our program that has been affected is the resident clinic. These clinics usually occur in the afternoon and are staffed with three or four residents, supervised by an attending. During the pandemic, we rescheduled routine visits and absorbed the resident clinic patients that needed to be seen into our attending clinics.
 |
|
VIRTUAL MENTORING. Social media connection has become especially important during the pandemic. Dr. Abugo (@MentorMeMD) offers mentoring to medical students on Twitter, Instagram, and Facebook.
|
Recruitment Issues
Dr. Pettey: For many years, ophthalmology has benefited from attracting the top medical students. How do we ensure that our profession continues to be attractive to medical students in the next 12-18 months?
Dr. Knight: The population most affected by our two-month shutdown has been our medical students, and we are concerned about the relative inaccessibility of the ophthalmology department to medical students in general, particularly those who are currently applying for match.
Regarding accessibility, prior to the pandemic most medical schools offered only a few hours or days of ophthalmology lectures in their core curriculum. Therefore, much of the medical student interest in ophthalmology is developed when they rotate through our clinics, complete research with us, or participate in community vision screenings and other service experiences. Without broad access to these opportunities—due to restrictions on clinical externships, social distancing limitations on lab space and community events, as well as imposed funding constraints—our ability to recruit medical students to ophthalmology may be diminished.
I’m concerned that, while students continue rotating through the core clinical rotations, the number of students seeking clinical ophthalmology rotations, and participating in research or community outreach events, may decline due to a general lack of exposure. I wonder if, in the year or two following the pandemic, we’ll see a dip in demand for ophthalmology residency positions. The only thing we can do is focus on how we are interacting with medical students. There’s been some talk of developing more virtual platforms and other ways to engage students. Depending on how long it takes for us to claw out of this shutdown phase, I think we’ll need to seriously consider those methods of interacting with students to attract them to the field.
Medical Student Resources on AAO.org
The Academy, in collaboration with AUPO’s Medical Student Educators Council, offers educational resources for medical students at aao.org/medical-students.
- Basic Ophthalmology. To help medical students continue their ophthalmic studies during the COVID-19 pandemic, the Academy is providing a three-chapter excerpt from Basic Ophthalmology, a key text for primary care residents and physicians.
- Guide to the Bedside Ophthalmic Exam. This presentation reviews basic ophthalmic physical exam maneuvers. In addition, real examples of both normal and abnormal exam findings are demonstrated. This is targeted to graduating medical students and primary care practitioners.
- Interactive Medical Student Cases. A primer for medical students who want to broaden their knowledge of eye disease diagnosis and treatment.
- Recorded webinars. Recordings of several webinars that were conducted for medical students (and others) include:
- 2020 Advice for the Ophthalmology Residency Match Season
- Ophthalmology Learning During COVID for Medical Students, Residents, and Educators (includes a PDF handout with a 10-day educational program for medical students)
- A three-part series in which ophthalmologists discuss opportunities available within the field and how to prepare for match
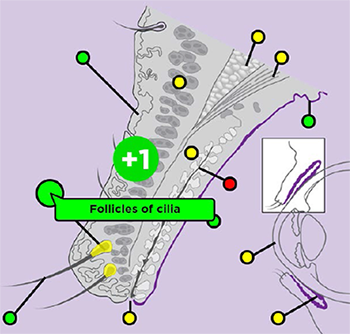
- Interactive figures. Interactive figures for medical students illustrate key concepts of eye anatomy and related functions and structures. (See image above.)
- Other resources. The medical student section of the Academy website also features information about the practice of ophthalmology, resources for medical student educators, details about the ophthalmology match process and residency structure, and a link to the Minority Ophthalmology Mentoring program.
|
E-Learning
Dr. Pettey: COVID has accelerated our entry into the virtual learning space and in many ways increased our connectedness, as we look to the future. Could you comment on e-learning and any other innovations that you think are here to stay that have put us in a better position moving forward?
Dr. Abugo: Absolutely. I have an extensive social media mentorship platform that encourages students to reach out to me via @MentorMeMD on Instagram, Twitter, and Facebook. A medical student reached out recently through Twitter, expressing concern about his away elective rotation being canceled. From this and similar conversations, what we’re seeing is an overwhelming feeling of lost opportunity. During my own away elective rotation I was able to get hands-on experience, and I got my research projects done. I also was able to attain my letters of recommendation through away elective rotations. This has been a huge area of concern for medical students, especially those who are applying in this cycle.
The challenges of the pandemic have given us a unique opportunity, as ophthalmologists, to reevaluate the way we educate our medical students. In the past few months, we’ve seen incredible examples of this, from many programs across the United States. They are stepping up to the plate and transitioning to more of a virtual educational platform. For instance, we have had access to webinars that are available through Wills Eye Hospital and the Department of Ophthalmology at Harvard; they offer new ophthalmology conferences and resident lecture series. Mass Eye and Ear has their glaucoma rounds. Bascom Palmer and Wilmer Eye also offer e-learning opportunities, to name just a few.
And of course, the Academy has a plethora of resources for medical students who have been struggling to find their way recently. The Academy hosted a helpful webinar on how ophthalmologists are responding during COVID, looking at what medical students, residents, and educators should be doing during this time. (See “Medical Student Resources on AAO.org,” above.) There are many innovations and resources birthed during this period in response to what ophthalmologists are seeing from our medical students.
Dr. Sun: I think we’re finding that we can still be connected through Zoom calls for didactics. My residents have had more didactics in the last three months than they’d ever had, and the faculty are more available than ever. In fact, the New York City program directors formed a group to have weekly calls to share best practices about various challenges—finding personal protective equipment at the very beginning, then sharing all of our didactics online, such that the residents at Cornell can attend Columbia and NYU didactics. We look forward to collaborating further! So there have been some pluses. We certainly took this as an opportunity, looking at what we can change for the better, pandemic or no pandemic, and one of those things is to collaborate with each other, communicate, and share resources. And I know that other parts of the country are doing the same, such as the Boston area and the Midwest.
Dr. Pettey: Increasing medical knowledge naturally lends itself to virtual teaching formats; however, clinical learning present unique challenges. What other challenges and innovations have you seen?
Dr. Sun: Surgical training has become more challenging with fewer opportunities to be in the operating room. For example, using simulation for surgical teaching is now more important than ever. Cataract conferences conducted by video have been a great way to engage and teach surgery. Tom Oetting at the University of Iowa has great resources online, as does Moran CORE, and Uday Devgan at UCLA with the Cataract Coach website. (See “Virtual Education Resources,” below.) The Academy and other ophthalmic societies have also developed additional online resources for surgical learning. (Next month, see Part 2 sidebar “AAO.org Resources for Residents and Fellows.”) We expect to integrate those resources into our residency.
Dr. Pettey: Great points, with residents’ low surgical case numbers, it is imperative to improve our trainees’ preparedness for their first live OR cases. Traditional wet lab and virtual reality simulation has become even more important.
Reverse Classroom
Dr. Pettey: For years, medical education has shifted from the traditional lecture format toward a “reverse classroom” model in which students learn and research the material ahead of a more interactive face-to-face encounter. How is the pace of that process changing during the pandemic?
Dr. Abugo: I think we can always look at the advantages that have resulted from this pandemic; I think education will be forever changed for the better. The reverse classroom is basically what we’ve been forced to do now—move the direct instruction from the group learning space to the individual learning space. This model has proved beneficial for students. It requires students to process, remember, and try to understand a topic before they listen to the professor’s prerecorded lecture. Afterward, an evaluation process takes place, along with a plan for further steps.
I think this is an incredible opportunity for us as educators, and it really speaks the language of today’s tech-savvy students. It’s useful, it’s helpful for busy students, and it allows students who are struggling to go at a slower pace. It also helps our educators to have a bit more time for themselves and to be more productive. So, yes, the pandemic is a unique challenge, but I think it’s a great challenge for educators in the future, and I’m very excited to see how we, as ophthalmologists, will respond to this.
As we’ve mentioned, many organizations are stepping up to the plate, including the Academy, the National Medical Association’s Ophthalmology Section’s Rabb-Venable program, Women in Ophthalmology, and the Association of University Professors of Ophthalmology (AUPO); these are just some examples. Although the pandemic is a big change and challenge for us, it also is an opportunity for great things for ophthalmologists.
Dr. Pettey: I couldn’t agree more. Serendipitously, the Moran Eye Center’s reverse classroom curriculum went live this year and to rave reviews.
Necessity being the mother of innovation, the COVID pandemic has pushed training programs and initiatives faster than ever before. With daunting challenges facing our colleagues in training, ophthalmology educators and programs are innovating at a faster pace than ever before.
___________________________
NEXT MONTH. Watch for Part 2 with discussion about medical school rotations, fellowships and job prospects, and some of the good that has come from the pandemic.
___________________________
Dr. Abugo is an oculoplastic surgeon at Virginia Eye Consultants and assistant professor of ophthalmology at Eastern Virginia Medical School in Norfolk. Financial disclosures: None.
Dr. Knight is assistant professor of ophthalmology and a medical student educator at the University of North Carolina at Chapel Hill. Financial disclosures: None.
Dr. Pettey is the John A. Moran Eye Center director of education and an assistant professor at the University of Utah Department of Ophthalmology and Visual Sciences in Salt Lake City. Financial disclosures: None.
Dr. Sun is residency program director and assistant professor of ophthalmology at Weill Cornell Medical College in Manhattan. Financial disclosures: None.