By Krishna Priya Kalyam, MD, Javier Fernandez-Vega, MD, Flora Levin, MD, Eric Baylin, MD, and J. Javier Servat, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Surgical intervention by dacryocystorhinostomy (DCR) is the mainstay treatment for epiphora resulting from nasolacrimal duct obstruction. The goal of this surgery is to reestablish lacrimal outflow by creating a bypass into the nasal cavity. Initially, DCR was performed as an external procedure, leaving patients with a scar in the medial canthal area and lower eyelid.
Over the past few decades, several advances in technology have enabled us to perform this procedure endoscopically to provide better cosmesis. Compared with external DCR, an endoscopic approach allows the surgeon to better navigate anatomic variations that might lead to failure of the surgery, such as a deviated nasal septum or an enlarged middle turbinate.
More recently, minimally invasive techniques like transcanalicular laser-assisted endoscopic DCR have gained popularity. Currently, this procedure is performed with an incision-free technique that avoids visible scarring, requires shorter operating time, produces less bleeding—and is easier to learn—than other DCR methods. Overall, the success rate of laser-assisted endoscopic DCR in relieving epiphora is reported to be between 60 and 90 percent.
This review will present an overview of patient selection, surgical technique, and recommendations for postoperative care.
Patient Selection
Examination. All patients should have preoperative nasolacrimal duct probing and irrigation to confirm nasolacrimal duct obstruction distal to the common canaliculus. Canaliculitis, canalicular scarring, and inflammatory membranes over the punctum should be documented if present. The surgeon should also perform an endoscopic nasal examination to assess for a deviated septum, intranasal masses, or a hypertrophic middle turbinate. A deviated nasal septum can make laser-assisted endoscopic surgery difficult, and a septoplasty (usually performed by ENT) may be indicated if the area is constricted.
Indications. The procedure is usually performed in patients who are concerned about external scarring and want a minimally invasive procedure. In addition, it is advantageous for patients who have bleeding disorders or must remain on anticoagulation medication.
Contraindications. Transcanalicular endoscopic DCR is contraindicated in patients who have lacrimal or nasal sinus neoplasia. Relative contraindications include dacryolithiasis, canalicular obstruction, and canaliculitis. In addition, caution is needed in patients with altered nasal anatomy. Imaging studies are recommended to evaluate such patients to determine the nasal bony anatomy prior to surgery in selected cases.
 |
|
EQUIPMENT. (1) 600-μm semirigid fiberoptic probe for laser delivery.
|
Benefits
Advantages of transcanalicular laser-assisted endoscopic DCR compared with conventional external DCR include the following: 1) minimal or no postoperative ecchymosis and edema, 2) less surgical manipulation of medial canthal tissues and lacrimal pump, 3) no scarring on the skin, 4) minimal bleeding, and 5) faster recovery time.
In comparison with nonlaser endoscopic techniques, transcanalicular laser-assisted endoscopic DCR has the advantage of minimal bleeding and requires less complex endoscopic surgical skills. The decreased operative bleeding is particularly advantageous for elderly patients who must remain anticoagulated or for those with bleeding disorders.
 |
|
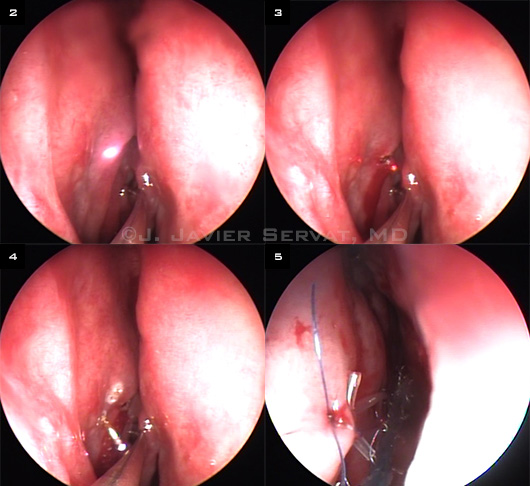
INSIDE VIEW OF THE SURGERY. (2) The aiming beam is visualized transmucosally in the nasal cavity with the endoscope. (3) The laser probe is used to create an osteotomy. (4) A #0 Bowman probe is visualized intranasally. (5) Silicone stents (Crawford tubes) are sutured to the lateral nasal mucosa with 6-0 Vicryl.
|
Equipment
An endoscopic tower with a rigid endoscope is required. A number of different lasers have been used to perform transcanalicular endoscopic DCR, including argon, erbium (Er):YAG, neodymium (Nd):YAG, and, most recently, the diode laser. All of these lasers are delivered via a 400- to 600-μm semirigid fiberoptic probe (Fig. 1). At our institution, we use the Intermedic Multidiode S15 OFT laser.
Patient Preparation
Nasal packing. Intranasal vasoconstriction and anesthesia begin with packing the nasal cavity between the middle turbinate and the lateral nasal mucosa with 1/4-inch neuropads soaked in a 4 percent cocaine solution (oxymetazoline can be used as an alternative). This packing is removed after five minutes.
Anesthesia. Local anesthetic is prepared in a 50:50 mixture of 2 percent lidocaine with 1:100,000 epinephrine and 0.5 percent bupivacaine with 1:200,000 epinephrine. Under direct visualization of the nasal mucosa through a 0-degree rigid endoscope, this anesthetic mixture is administered to the submucosa of the anterior middle turbinate and lateral nasal wall. The nasal cavity is then repacked in the same fashion for an additional five minutes.
Operative Procedures
A metallic corneoscleral shield is placed over the eye on the operative side to protect it from the laser. The packing is then removed from the nostril. The endoscope is brought into the field and inserted into the nose.
Turbinate infracture. To improve visualization, an infracture of the middle turbinate can be performed with a blunt periosteal elevator. This maneuver also helps to protect the middle turbinate from the thermal energy of the laser.
Inserting the probe. The superior and inferior lacrimal puncta are then dilated and irrigated with the same mixture of lidocaine/bupivacaine used to anesthetize the nasal mucosa.
Next, the laser fiberoptic probe is introduced through the lower punctum until a hard stop is felt. An aiming beam is turned on and visualized transmucosally in the nasal cavity with the endoscope (Fig. 2).
Laser technique. Under endoscopic guidance, the aiming beam is oriented to deliver laser energy to the nasal bone and lateral mucosa. A continuous-wave contact laser at 10 W of power is used to create an osteotomy (Fig. 3). After the first few passes, the laser power is decreased to 8 W to enlarge the osteotomy (Fig. 4).
The laser probe is then removed, and the lacrimal system is irrigated with fluorescein solution and checked for patency.
Intubation. Next, bicanalicular silicone intubation of the nasolacrimal system is performed. The length and position of the tubes are checked with the endoscope and secured into position with a 6-0 double-armed Vicryl (polyglactin 910) suture tied to nasal mucosa (Fig. 5). Some surgeons use neuropads soaked in mitomycin C at the end of the procedure, and these pads are removed in the recovery room.
Postoperative Care
Patients can go home on the same day as the procedure. They are instructed to use saline nasal spray and to avoid blowing their nose for the first week after surgery to reduce chances of intranasal bleeding. They are usually seen at one week, six weeks, and three to six months following surgery.
Stent removal. In our practice, we usually remove the silicone stent three months after surgery, at which point the sutures have been absorbed. This timing differs among surgeons, ranging from one to six months. The tube is cut and pulled out through the lower canalicular system. After the tube is removed, the lacrimal system should be irrigated to check for patency.
___________________________
1 Woog JJ et al. Ophthalmology. 2001;108(12):2369-2377.
2 Hong JE et al. Ophthalmology. 2005;112(9):1629-1633.
3 Henson RD et al. Ophthal Plast Reconstr Surg. 2007;23(2):134-137.
4 Plaza G et al. Ophthal Plast Reconstr Surg. 2007;23(3):179-182.
___________________________
Dr. Kalyam is a resident, and Dr. Levin is assistant professor, in the Department of Ophthalmology and Visual Science, Yale University, New Haven, Conn. Dr. Baylin and Dr. Servat are in practice at Oculofacial Plastic Surgeons of Georgia, in Atlanta. Dr. Fernández-Vega is in practice at the Instituto Oftalmologico Fernández-Vega, Oviedo, Spain. The authors report no related financial interests.