Download PDF
Stem cell– and gene-based therapies in ophthalmology are back in the news. In February, researchers published the first evidence of medium- to long-term safety, graft survival, and biological activity of tissue derived from human embryonic stem cells (hESCs).1 In April, scientists in Korea reported that they had successfully injected hESC-derived retinal support cells into the eyes of 4 patients with macular conditions, including age-related macular degeneration (AMD).2 And in May, another research team published long-term results of gene therapy in Leber congenital amaurosis (LCA).3
A Game-Changing Era
Gene therapy and stem cell therapy are overlapping areas of biomedical research with similar therapeutic goals. In gene therapy, a specific gene is delivered via a viral vector; in stem cell therapy, whole cells are infused or transplanted into a patient. Both approaches are being investigated for the treatment of inherited and acquired diseases.
Explosive growth. “This is a really exciting time for gene therapy in ophthalmology,” said Jean Bennett, MD, PhD, at the University of Pennsylvania Perelman School of Medicine in Philadelphia. Interest in the field is growing very fast, she said, with at least 2 dozen groups of researchers worldwide having generated proof of concept.
The eye as an ideal target. Many ophthalmologists consider the eye to be an optimum target organ for gene therapy because of its relative accessibility and compact size. Moreover, the eye is considered an immune-privileged site, in that cells implanted there are less likely to be rejected than they might be in other parts of the body.
Wide scope. And the potential applications within ophthalmology are broad: “AMD, glaucoma, and other inherited diseases—and some nonhereditary diseases—may be candidates for gene and stem cell therapy,” said Elliott H. Sohn, MD, at the University of Iowa in Iowa City. In fact, the Stem Cell Ophthalmology Treatment Study (SCOTS) is expected to study patients with a number of retinal and optic nerve diseases—not only AMD but also myopic macular degeneration, hereditary retinopathies such as retinitis pigmentosa (RP) and Stargardt disease, and optic nerve diseases such as optic atrophy and optic neuritis.4
In discussing these diseases, Dr. Sohn noted that gene therapy can be applied in a variety of ways. “For instance, it can replace a defective gene for inherited retinal disorders like retinitis pigmentosa and LCA, or it can provide key proteins needed to restore vision in more common diseases like AMD.” There are also data to suggest that stem cells could play a supportive role in replacing non-neuronal cells that have died, said J. Timothy Stout, MD, PhD, MBA, at Baylor College of Medicine in Houston.
Here’s an update on leading research targets and some recent study findings (for more information, see www.clinicaltrials.gov).
|
Web Extra: Clinical Update
|
 |
Research Target: LCA
Gene therapy. The first approval of gene therapy in the United States is most likely to involve an intervention for a very rare form of LCA due to RPE65 mutations, Dr. Bennett said. If and when that use of gene therapy is approved, it may be followed by a green light for its use in other inherited and acquired forms of retinal disease, she added.
LCA can be caused by one or more of 19 different genes, and it affects about 1 in 80,000 individuals. The onset of symptoms typically begins in infancy. More than 200 patients with LCA have participated in gene therapy trials since 2007.
One of the ongoing clinical trials for LCA—a phase 3 study at The Children’s Hospital of Philadelphia—requires only a single subretinal injection. This trial has 29 patients enrolled in the United States and other countries, and study data are now being tabulated for submission to the FDA.
But as the study results published in May indicate, successful long-term benefits remain elusive. Although gene therapy initially resulted in better vision, that improvement peaked between 1 and 3 years after treatment and declined thereafter.3
Stem cell therapy. This approach “is likely to be most useful for patients who are further along in the disease process, compared to those who might benefit from gene therapy,” said Dr. Sohn. Likely candidates are those who are in their teens or older.
Research Target: AMD
Stem cell therapy. In AMD, stem cell therapy is being investigated as a way to replace damaged retinal pigment epithelium (RPE) cells and prevent disease progression and further deterioration of photoreceptors.
In the Korean study, the researchers differentiated hESCs into RPE cells and injected them into 1 eye of each of the 4 patients (2 of the patients had AMD, while the other 2 had Stargardt macular dystrophy). No adverse events associated with the cells were noted during the study. With regard to visual acuity, 1 AMD patient gained 9 letters during the year of follow-up, while the other gained 1 letter; of the Stargardt patients, 1 gained 12 letters of vision, while the other gained 19 letters.2
In another study of 33 patients, the investigational adult stem cell line CNTO 2476 was injected under the retina. After 1 year, there were improvements of 4 to 5 letters, compared with the loss of 2 letters in untreated fellow eyes. The results of this phase 1/2a clinical trial were promising enough that a phase 2b trial is now in the planning stages. All told, researchers plan to enroll 160 patients (www.clinicaltrials.gov).
Gene therapy. Currently, several gene therapy options are in early clinical trials, administered via intravitreal or subretinal injections to suppress angiogenesis.5 The hope is that these trials can demonstrate the safety not only of the drugs but also of the procedure or the mechanism for delivery, said Dr. Stout.
With regard to the use of virus vectors, small trials—including one using RetinoStat (a lentiviral-based therapy) for neovascular AMD, for example—have treated the retina with a single subretinal injection at 3 different doses to evaluate safety and other parameters. Protein expression has been sustained for up to 12 months.5
Challenges
As with any revolutionary development in medicine, a number of key challenges remain. For example, the use of hESCs remains an area of controversy on ethical grounds.
Safety and efficacy. To date, gene therapy studies have demonstrated proof of safety and efficacy. Now researchers are looking at other areas, such as the safe delivery of viral vectors to the outer retina.6
Although stem cells themselves seem to be relatively safe and well tolerated, Dr. Stout said, efficacy is still unclear. “The use of stem cells is picking up steam, and there are a number of ways to think that stem cells might be useful. However, we don’t have a lot of good data to suggest that stem cells might be therapeutically effective because they can connect with cells of the middle retina in a useful way.”
And unanswered questions remain with regard to immunogenicity. Studies to date have not yet addressed how long stem cells last and whether or not they are immunogenic, Dr. Stout said.
Delivery issues. Dr. Stout noted that although it is very early in the research process, it is often difficult to deliver the right cells into the right space. For instance, he said, “We need to spend more time thinking about exactly how to deliver stem cells.”
Talking to patients. Because news reports on these advances often get a response from anxious patients, the experts also offered some advice.
Despite optimism that gene and stem cell therapies will continue to make great strides, Dr. Sohn emphasized that “the vast majority of these treatments are in early phase clinical trials and are not FDA approved or widely available.” The best thing patients can do now is seek care from physicians with expertise in their condition, he said. “They should see a knowledgeable provider with access to quality genotyping and genetic counseling. After the genetic diagnosis is confirmed, then they can consider the option” of participating in a relevant trial, if that is a possibility.
Despite these cautions, the experts believe that the future is bright for this area of research. As Dr. Sohn put it, “A lot of the animal experiments that we’ve done suggest that there really is a role for both stem cell and gene therapy for human ocular diseases.”
___________________________
1 Schwartz SD et al. Lancet. 2015;385(9967):509-516.
2 Song WK et al. Stem Cell Reports. 2015;4(5):860-872.
3 Bainbridge JW et al. N Engl J Med. 2015;372(20):1887-1897.
4 Mead B et al. Stem Cell Research. 2015;14:243-257.
5 Pecen PE, Kaiser PK. Curr Opin Ophthalmol. 2015;26(3):188-193.
6 Trapani I et al. Hum Gene Ther. 2015;26(4):193-200.
___________________________
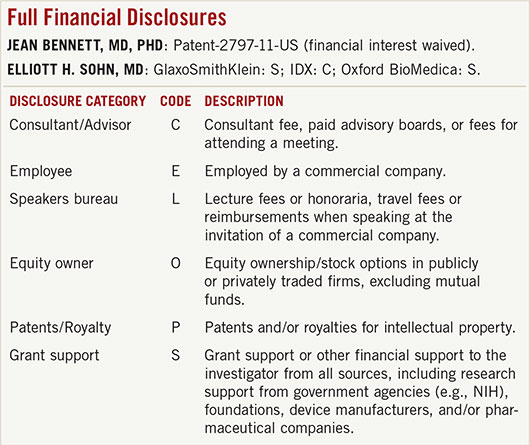
Jean Bennett, MD, PhD, is professor of ophthalmology at the University of Pennsylvania Perelman School of Medicine in Philadelphia. Relevant financial disclosures: Avalanche Biotechnologies: C; Novartis: C; Spark Therapeutics: S.
Elliott H. Sohn, MD, is assistant professor of vitreoretinal diseases and surgery at the University of Iowa in Iowa City. Relevant financial disclosures: None.
J. Timothy Stout, MD, PhD, MBA, is professor and chair of ophthalmology and director of the Cullen Eye Institute at Baylor College of Medicine in Houston. Relevant financial disclosures: AGTC: C; Oxford Biomedica: C.
For full disclosures and the disclosure key, see below.