Download PDF
Note: In the initial version of this article, EyeNet incorrectly identified clemastine fumarate as Claritin. The article has been amended to address this error.
Multiple sclerosis (MS) is a degenerative inflammatory disease of the central nervous system (CNS) involving destruction of myelin and progressive neuroaxonal loss. Treatments capable of remyelination are a major unmet need for patients with the disease. However, researchers at the University of California, San Francisco (UCSF), may have taken a step toward filling that need using the visual system and the antihistamine clemastine fumarate.1
The study. For this double-blind randomized trial, known as ReBUILD, investigators included 50 patients with relapsing MS and chronic demyelinating optic neuropathy. Patients were randomized into 2 groups: The first received oral clemastine fumarate twice daily for 3 months and then placebo for 2 months, while the second received the placebo for 3 months and the active treatment for 2 months.
The primary outcome measure was shortening of P100 latency delay on full-field visual-evoked potentials. “Visual sensory dysfunction is the first symptom in up to 40% of patients with MS, and injury to the optic nerve is extraordinarily common,” said Ari J. Green, MD, at the UCSF Multiple Sclerosis Center. “It made sense for us to choose the visual pathway for investigation, especially because of the precision of clinical tests available for assessment.”
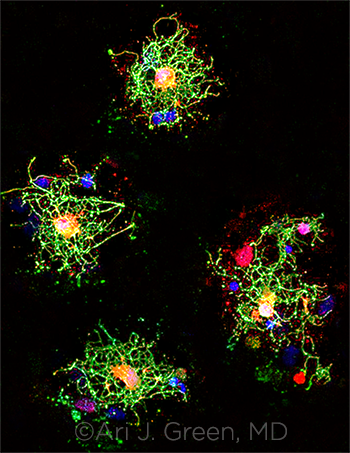 |
OLIGODENDROCYTES. Clemastine fumarate can stimulate differentiation of oligodendrocytes (shown here). From the lab of Jonah R. Chan, PhD.
|
Possible remyelination? Patients in both groups experienced a reduction in latency delay while on the antihistamine treatment, demonstrating that the drug has a possible remyelinating effect, even after prolonged damage to the CNS.
To Dr. Green, this represents what he termed “a major breakthrough” for drug-induced repair in a chronic neurodegenerative condition. “To our knowledge, this is the first time that a drug has reversed the deficits caused by MS. We aren’t saying it’s a cure, but this is a step toward that direction.”
Importance to ophthalmologists. For Dr. Green, the ReBUILD study demonstrates the value of ophthalmology in treating MS, as there’s also preliminary evidence from the trial suggesting that drug-induced remyelination might extend to improved low-contrast letter acuity in patients with MS. But that might only be the beginning.
“We’ve been taught in the past that the retina and optic nerve are incapable of self-repair; however, we need to develop a more nuanced view acknowledging that there is some capacity for regeneration,” he said. Thus, he said, as clinicians wait for other promising treatments, including stem cell therapy, to bear fruit, “we should harness the eye’s own natural regenerative abilities, utilizing the processes that biology already provides us and manipulating them via specific medications.”
—Mike Mott
___________________________
1 Green AJ et al. Lancet. 2017;390(10111):2481-2489.
___________________________
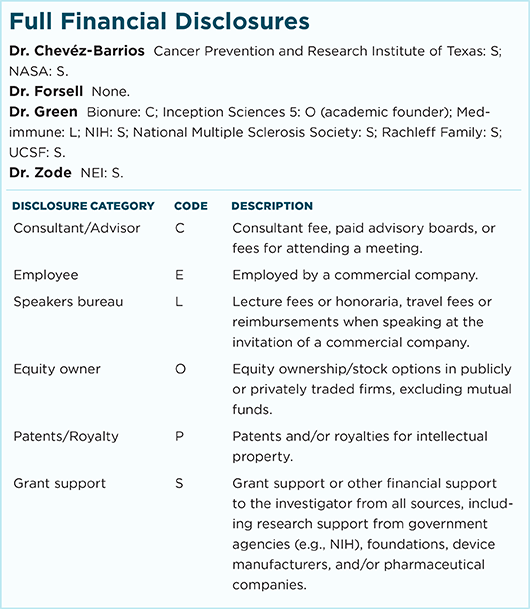
Relevant financial disclosures—Dr. Green: NIH: S; National Multiple Sclerosis Society: S; Rachleff Family: S; UCSF: S.
For full disclosures and disclosure key, see below.
More from this month’s News in Review