By Annie Stuart, Contributing Writer, interviewing Durga Borkar, MD, Gary N. Holland, MD, and Benjamin Reiss, MD
Download PDF
During this pandemic, we are continuing to do our best to safely provide optimal care for vision-threatening conditions, regardless of a patient’s COVID-19 status, said Durga Borkar, MD, at Duke University School of Medicine in Durham, North Carolina.
But what if the patient is infected with SARS-CoV-2 and you need to perform vitreoretinal surgery? How does this change your practices?
“You want to delay as long as possible to avoid operating on someone who could be actively shedding the virus, but not so long as to produce negative visual consequences,” said Benjamin Reiss, MD, at the Retina Institute of Washington in Renton.
Both Drs. Borkar and Reiss recently performed retina procedures on patients who tested positive for SARS-CoV-2. Together with Gary N. Holland, MD—who is one of three ophthalmologists curating clinical content for the Academy’s aao.org/coronavirus web pages—they share their insights on how to balance the surgical needs of the patient with the safety of all concerned.
Factors to Consider Before Deciding on Surgery
Deciding whether or not to operate on a COVID–19 positive patient involves a multifaceted calculus: It considers not only the patient’s specific condition but also professional guidelines, institutional policies, risks to surgeon and staff, and the office workflow.
Professional guidelines. Both the Academy and the American Society of Retina Specialists (ASRS) provide general guidelines for ophthalmologists considering surgery, said Dr. Holland, at the Stein Eye Institute, University of California, in Los Angeles.
These guidelines cover everything from personal protective equipment (PPE) recommendations and risk assessments to specific protocols regarding patient care.1,2 They leave room for discretion, said both Drs. Holland and Reiss. “That’s partly because doctors must consider many specific details, such as whether or not a patient is functionally monocular,” said Dr. Reiss.
Discretion is also called for because each region and institution varies in risk level and access to PPE, equipment, beds, and staff. “Not all places can adhere to the ideal,” said Dr. Holland. “Also, there’s a lot we still don’t know, for example, whether or not procedures such as retina surgery are aerosol generating. Recommendations may need to change as we gather more information.”
Institutional policies. Because of regional and institutional differences, hospitals have developed their own additional policies for handling COVID-19 positive patients, which surgeons need to follow, said Dr. Borkar. This requires a conversation with the hospital and OR staff to determine whether a team, room, and supplies are available, said Dr. Reiss.
The patient’s condition. “Many conditions we treat in our retina subspecialty are urgent and nonelective,” said Dr. Reiss. This includes conditions such as retained lens fragments, endophthalmitis, retinal detachment, acute vitreous hemorrhage of unknown etiology, and flashes and floaters.
Dr. Borkar said that three factors help influence her decision in an urgent case: 1) The patient is systemically well enough to safely undergo surgery. 2) The patient has good visual potential. 3) It’s likely that taking the patient to the OR will provide a superior standard of care over an in-office procedure. Of course, she added, this decision is easier for physicians affiliated with an institution that has an adequate setup for taking care of a patient infected with SARS-CoV-2.
Infection risks to surgeons and staff. “We need to balance patients’ needs against the safety of health care providers,” said Dr. Holland. “As parts of the country open up and more physicians return to work,” he cautioned, “we shouldn’t be lulled into a false sense of security. Whether in the operating room or clinic, consider all patients as being potentially infected.”
Office workflow. Surgeons need to consider not only the availability of an OR but also the scheduling of exams before and after surgery in the clinic setting, Dr. Holland said. “We need to maintain social distancing and rigorous disinfection procedures between cases, so we can’t have waiting rooms full of post-op patients.”
When it’s a “no go.” Because of PPE shortages, surgeons have been delaying cases, even when the patient tests negative, said Dr. Reiss. However, the longer you wait for most retinal procedures, the worse the outcome, he said. “Epiretinal membranes and macular holes may not be emergencies, but if you wait long enough, they will likely get worse.”
 |
|
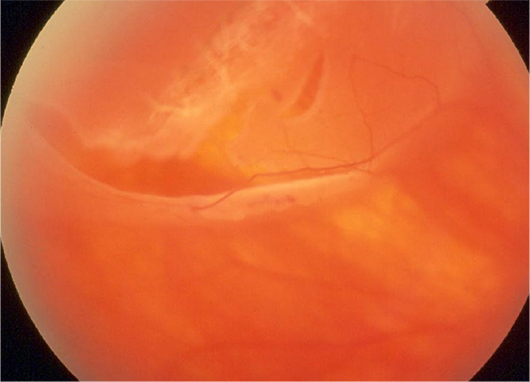
RETINAL DETACHMENT. Urgent and nonelective surgeries for conditions such as retinal detachment require extreme care in patients who are positive for COVID-19.
|
Before Surgery: Planning and Precautions
With the advent of the pandemic, presurgical planning has become pivotal and more involved.
COVID-19 testing. The hospitals that Drs. Reiss and Borkar are affiliated with have initiated routine reverse transcription polymerase chain reaction testing for anyone going to the OR, whether symptomatic or not. “For urgent cases, we use point-of-care testing and can have results in less than 30 minutes,” said Dr. Borkar.
If a case is urgent enough to be scheduled for surgery, testing for COVID-19 is a helpful tool. “For example, the surgeon and anesthesiologist can take extra steps to protect themselves.” Where abundant testing is not available, said Dr. Holland, we have to balance the ideal with the practical. “Assume that asymptomatic patients may be infected and use universal precautions with all cases,” he said. “Even as testing becomes more widespread, we need to remember that false-negative results can occur.”
Presurgical clinic visit. “Our clinic has stringent protocols for all patients,” said Dr. Reiss. In addition to minimizing contact between patients, cleaning exam rooms, and having patients wear masks, he said, the clinicians dilate or check pressures only if absolutely necessary. In some cases, telemedicine is used to minimize exposure.
Conversations about anesthesia. Because intubation and extubation are aerosol-generating procedures, said Dr. Holland, it’s critical to talk with the anesthesiologist about the use of local versus general anesthesia.
“In ophthalmology, we do a lot of cases under monitored anesthesia care, although some cases, such as urgent trauma cases where the patient is in severe pain, may require general anesthesia,” said Dr. Borkar. Making the appropriate decision preoperatively is imperative because switching midstream isn’t easy with a patient who’s positive for COVID-19, she said. “Intubation requires a coordinated effort on the part of the anesthesia team. If you’re even considering general anesthesia, the anesthesiologist may recommend going ahead with it from the outset to allow doing it in the most controlled fashion.”
If the case doesn’t warrant general anesthesia, however, avoid it to minimize the risk to the anesthesiologist, said Dr. Reiss. “For the ophthalmologist, the highest risk would then be during the preprocedure block.”
OR. Each institution has its own unique setup, said Dr. Borkar. “But at Duke, surgeons operate on COVID-19 patients in a dedicated operating room. In this setting, she said, “be sure to familiarize yourself with the available vitrectomy and visualization systems because they may be different than what you are used to.”
If you’re using an OR where eye surgeries are not normally performed, you’ll need to make a clear list before surgery of all the equipment you’ll need, said Dr. Reiss. At his hospital, everything has been removed from the OR. Only the exact supplies needed for each surgery are placed in the OR. That’s because everything in the OR is thrown away after surgery, as it is considered contaminated.
Transport and pre-op holding area. “We don’t normally have to think about logistics such as transporting the patient, but now we do,” said Dr. Borkar. “Know your institution’s special protocol for getting patients safely to the OR and where they will wait beforehand. We can’t hold them in a general pre-op area where only curtains typically separate them from other patients.” At Dr. Reiss’s institution, an OR floor and negative-pressure pre-op bay have been specifically designated for COVID-19 positive patients.
Pre-op patient prep. “Upon arrival, my patient was wearing a mask and went straight to the negative-pressure pre-op bay,” said Dr. Reiss. “Only the nurse and the anesthesiologist went into the room to prep the patient for the case. Since I had already spoken with the patient over the phone, I saved preoperative marking for the OR so I wouldn’t have to gown up and use additional PPE to enter the preoperative bay.”
Intubation, if needed. “To avoid risk of infection from aerosolization,” said Dr. Borkar, “everyone except the anesthesia team stays outside the room during intubation [and extubation], and they wait 15 minutes before going in.”3
During Surgery: Minimizing Risks
Minimalism. Have the minimum number of people in the room that’s needed to provide the best level of care, said Dr. Holland. He added that it’s now inadvisable to change out members of the surgical team while the surgery is in progress.
Dr. Borkar is at a teaching institution, and the pandemic has introduced additional challenges for fellows. “Although there’s not a ‘right’ or ‘wrong’ approach,” she said, “try to find a balance between training and expediting the case as quickly as possible.”
Don, doff, and dispose of PPE. Generally, your institution will have clear, posted instructions about handling PPE, said Dr. Borkar. Some institutions may sterilize and reuse masks, which is a practice at Dr. Reiss’s hospital.
Initial steps in the OR. “As soon as my COVID–19 positive patient was in the OR,” said Dr. Reiss, “we used an oxygen mask to cover the [patient’s] nose and mouth, instead of a nasal canula. We quickly scrubbed the eye, put the drape on, and gave propofol sedation and a retrobulbar block through the drape in case the patient coughed while sedated.” Completely covering the airway—with only the eye exposed—helped protect the team during the highest-risk part of the procedure, he said.
Face protection. Know ahead of time what your institution’s face-protection protocol is for operating on COVID-19 patients, advised Dr. Borkar. “We wear an N95 mask and an overlying face shield. Standard face shields don’t work for ophthalmic surgery because you can’t get your face close enough to the microscope.” A couple of alternatives are surgical masks with a partial face shield attached or swim or chemistry goggles, she said.
Although he’d worn an N95 in the past, Dr. Reiss was test fitted again before operating on his patient. “In addition to a low-profile eye shield, I wore a surgical mask over the N95 in the OR, but I don’t do this on a routine basis unless there’s a known high-risk exposure.”
Although the ASRS has recommended N95 masks for retina surgeons, if available, the need to use an N95 mask for all types of surgery has not been proven, said Dr. Holland, and there may not be an adequate supply for every case at every institution. “Wearing a surgical mask over the N95 mask helps keep it clean so the N95 can be reused,” he said.
Gowns and gloves. Although gowning and gloving guidelines are also specific to each institution, it’s common to wear a thicker gown than usual and to double glove, not normally done for eye surgery unless there’s a higher infection risk from a needle stick, said Dr. Borkar. “Double gloving also allows you to remove the top pair at the end without touching anything and have a clean pair underneath to remove other PPE,” she said.
Feet coverings. “Many of us take our shoes off to put our feet on the microscope and vitrectomy pedals when we’re operating, but that’s probably not the best idea around COVID–19 positive patients,” said Dr. Borkar. “Either consider wearing foot covers over your socks, or wear really thin-soled shoes.”
Longer-acting gas. For a superior retinal break, Dr. Reiss would normally use a shorter-acting gas. Instead, he and his colleagues recommend using C3F8 gas. This decreases the risk of an undetectable detachment while the patient quarantines for 14 days—not returning for the post-op visit until the end of week 2.
After Surgery: Continued Caution
Again, each institution will have its own processes, but these are a few things to consider.
Post-op recovery. “It is good to get a social worker involved, if that resource is available,” said Dr. Borkar. That’s because an urgent retinal condition is now complicated by infection with SARS-CoV-2. These are some of the biggest questions you might need help answering: Where will the patient go after surgery? Does the patient live alone? Will the patient need to be admitted? What are the quarantine restrictions once the patient is discharged, and how will the patient return for follow-up?
Post-op visit. At Dr. Reiss’s facility, the hospital arranged for the patient to return the following morning to the negative-pressure bay for the post-op visit for an eye pressure check and a quick exam. “Otherwise, the patient would have come back to our clinic where we really don’t have the best setup to protect our staff or other patients from being exposed.”
In some cases, however, you can’t avoid seeing the patient postoperatively in the office, said Dr. Borkar. She advises considering steps like these to lower risks and reduce the use of PPE:
- Have the attending surgeon do the whole post-op check from start to finish, without the participation of staff and trainees.
- Have affected patients call you when they arrive in the parking lot. Meet and walk them through a side entrance, if possible, where they can go directly into an area that is more sequestered.
- See the patient at the very end of the day, which allows environmental services to thoroughly clean afterward before any other patients are seen in the area.
Telehealth. What if patients can’t get back to the office for appointments? They might have low acuity in both eyes and not be able to drive. And if they are being asked to quarantine from their family members, they can’t get a ride. “This may be where telehealth can come in, especially for uncomplicated retinal detachment follow-up in the early postoperative period,” said Dr. Borkar. “Whether the patient is COVID-19 positive or negative, we still want to minimize how much they are coming in for office visits during this pandemic.”
A Positive Mindset
In closing, Dr. Reiss advises not treating COVID–19 positive patients differently overall. “If you take appropriate precautions, you can still take care of them,” he said, adding that he felt completely safe during his procedure. “Don’t shy away from treating these patients.”
___________________________
1 aao.org/headline/special-considerations-ophthalmic-surgery-during-c. Accessed on May 30, 2020.
2 asrs.org/advocacy/updates. Then scroll to “ASRS Issues Best Practices Update for PPE During Vitreoretinal Surgery.” (Log in required.)
3 Chandra A et al. Eye (Lond). Published online May 12, 2020.
___________________________
Dr. Borkar is a vitreoretinal surgeon and assistant professor of ophthalmology at Duke University School of Medicine in Durham, N.C. Relevant financial disclosures: None.
Dr. Holland is director of the Ocular Inflammatory Disease Center at the UCLA Stein Eye Institute at the University of California in Los Angeles. Relevant financial disclosures: None.
Dr. Reiss is a vitreoretinal surgeon at the Retina Institute of Washington in Renton, Wash. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Borkar Genentech: C.
Dr. Holland None.
Dr. Reiss None.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|