Download PDF
Is virtual reality (VR) the future of ophthalmic medical education? It may well be. VR offers residents a risk-free way to learn diagnostic and surgical skills—and it does so in a compelling, immersive, 3-D manner. VR’s potential is also expected to extend well beyond residency to midcareer surgeons who want to refine their skills or learn new procedures.
Here’s a look at two VR platforms developed specifically for ophthalmic education.
 |
|
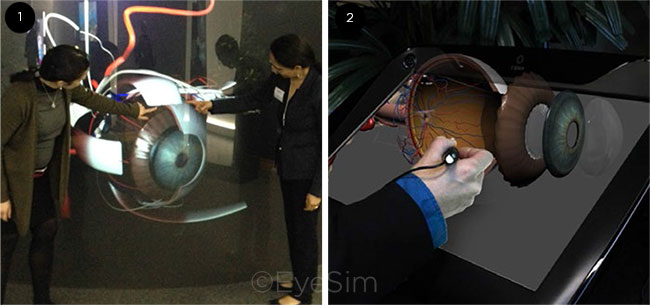
EYESIM. Images can be seen on 3-D classroom screens (1) and a large, mobile holographic display (2).
|
EyeSim: Student Immersion
For the past six years, Anuradha Khanna, MD, has been using VR simulation tools to augment traditional methods of teaching medical students and residents about ophthalmology.
“Virtual reality provides us with a medium in which we can simulate the micro and the abstract, and it allows the students the opportunity to practice and practice in a safe environment until they achieve mastery,” said Dr. Khanna, at Loyola University in Chicago.
Stereo classroom. Dr. Khanna developed the ophthalmic VR software that Loyola uses, called EyeSim (A Nu Reality). Several other medical schools and ophthalmology training programs around the country have adopted it.
Instead of wearing VR headsets, the teacher and students wear special glasses that enable them to see images displayed on a classroom screen or mobile device in three dimensions. “In a stereo classroom, we all wear 3-D glasses, and the content is interactive,” Dr. Khanna said. “If I’m taking them through the blood vessels in the eye, or through the visual pathways starting from the retina all the way to the brain, I can stop and change the angle and rotate the anatomy [and] zoom in and out.” The result is essentially a virtual dissection, she said.
Each student also can view these same anatomical images—or conduct a simulated eye exam—on a large, mobile holographic display (the “Ibench”) in a skills transfer lab, she said. Motion sensors in the 3-D glasses enable the student to rotate and zoom the images via head movement. “Or they can study independently on their smartphones or their smart tablets,” she said.
“Wow!” factor. The strategy of delivering information via the triad of a stereo classroom, a hands-on simulation skills lab, and a discussion with feedback has proved to be an effective one, Dr. Khanna said. “We are not providing information for the students, we are actually leading them toward conceptual clarity and refining their examination skills. I’ve witnessed, many times, the ‘Wow!’ factor that happens when they understand the correlation between the clinical presentation and the anatomical pathology.”
Dr. Khanna added, “You don’t have to motivate them to pick up a book or pay attention. Nobody’s on their cell phone texting or pretending to take notes during these sessions. They are immersed in the training,” she said. “And because, generally, we have limited time, I really have to almost peel them away from these simulators to move along to the next station. They’re enjoying it.”
Potential drawbacks. Despite her enthusiasm for EyeSim, Dr. Khanna said that there are both human and economic barriers to bringing a VR focus to ophthalmic education. “Faculty buy-in is slow, because faculty members commonly lack experience with VR-based teaching tools,” she said.
The technological and development costs are significant, she said. For instance, a comprehensive EyeSim system includes multiple Ibench holographic displays, stereo classroom screens, and the VR software itself. “It also is costly and time-consuming for companies to develop high-quality VR educational content. What we have available thus far is limited,” she said.
 |
|
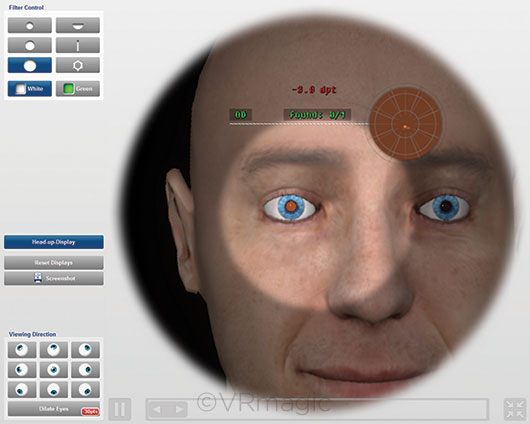
EYESI. Some residency programs require residents to complete the Eyesi cataract surgery modules before proceeding to live surgery.
|
Eyesi: Minimizing Risk to Patients
The most widely used device for performing virtual ophthalmic surgery is Eyesi Surgical (VRmagic), a system designed to train novices in cataract and vitreoretinal surgery.
More than 300 Eyesi Surgical simulators are in use around the world, with more than 100 of them in the United States. VRmagic also sells separate simulators that allow users to practice direct and indirect ophthalmoscopy. A new device, Eyesi Slitlamp, was unveiled at AAO 2018 in Chicago and is expected to be commercially available this year.
In Eyesi’s cataract surgery version, the student looks through what appears to be a surgical microscope and manipulates handpieces to move attached instruments around “inside” the 3-D virtual anterior chamber seen in the oculars. In reality, the instruments are moving about in a hollow model of a reclining head. The system automatically generates a numerical assessment of how the student did on each step of the procedure, on a scale of 0-100; students and teachers can use the figures to track improvement over time.
Surgical training begins here. R. Michael Siatkowski, MD, at the Dean McGee Eye Institute in Oklahoma City, said ophthalmology residents at McGee are required to complete the Eyesi cataract surgery modules before proceeding to live surgery. “This has really revolutionized surgical education for residents, as opposed to the old method of ‘see one, do one, teach one,’” Dr. Siatkowski said.
“We have anecdotally seen evidence that our residents are much more prepared to perform cataract surgery as a result of having completed these VR-based techniques. It allows the residents to begin to learn at a higher level in more complex situations when they’re doing real surgery,” he said. “And I think that most program directors with an Eyesi simulator would agree that it results in better patient care as well.”
Risk-free. Andrew T. Melson, MD, a Dean McGee neuro-ophthalmology fellow who was chief resident there last year, said he was grateful that, during his first year of residency, he could learn to navigate the intraocular landscape in a virtual setting where the consequences were also virtual.
“I’ve spent probably the better part of 50 to 100 hours on a virtual reality surgical simulator, and I can attest to the fact that it has made me a better, more confident beginning surgeon,” Dr. Melson said. “In a field where one wrong move during surgery can lead to blindness, the use of this type of technology to develop skills in a realistic environment shouldn’t be underappreciated,” he added.
Paradigm shift. The Eyesi training module for making a capsulorrhexis is particularly well-designed and helpful to students, Dr. Melson said.
“I’ve heard from several attendings that historically the capsulorrhexis was one of the most difficult parts of the surgery to teach—the step that they would save for later down the road, once the resident was well-versed in intraocular surgery,” he said. “But with Eyesi training, it’s oftentimes one of the easiest and most comfortable aspects of the procedure for residents. I’ve heard several attendings who have been very impressed with how quickly people become proficient at that step. That’s been a huge paradigm shift.”
A recruiting tool? Most medical students have little or no exposure to ophthalmology in their regular curriculum, Dr. Siatkowski said. But they react enthusiastically when, as happens at Dean McGee, they are given the opportunity to do tasks or perform virtual eye surgery with the Eyesi, Dr. Melson said. “I think it actually serves pretty well as a recruitment tool,” he said.
Disadvantages. The drawbacks of Eyesi lie chiefly in what is missing from the simulator and in its cost, Dr. Siatkowski said.
The tactile/proprioceptive feedback, though impressive, is still not identical to in vivo surgery, so users have an incomplete experience of what it feels like to, for instance, make a clear-corneal incision, deal with various degrees of tissue elasticity, or manipulate a lens, he said.
The device is expensive: about $170,000 for the cataract surgery version, and an additional $80,000 with vitreoretinal capabilities added.
“We still have further to go to make it more realistic and real-world. And, eventually, the cost has got to come down to make these more accessible to learners worldwide,” Dr. Siatkowski said. “When those things happen, then the tool will also become useful for helping the established surgeon learn new techniques, as well as for measuring and assuring continued surgical competence among physicians who have completed training.”
___________________________
Meet the Experts
Anuradha Khanna, MD Professor of ophthalmology and vice chair of education at Loyola University’s Department of Ophthalmology in Chicago. Financial disclosures: A Nu Reality: O; EON Reality: C.
Andrew T. Melson, MD Neuro-ophthalmology fellow at the Dean McGee Eye Institute in Oklahoma City. Financial disclosures: None.
R. Michael Siatkowski, MD David W. Parke II, MD, Professor of Ophthalmology, David Ross Boyd Professor, vice chair for Academic Affairs, and director of the Residency Program at the Dean McGee Eye Institute in Oklahoma City. Financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.