Download PDF
Premature births are on the rise in the United States now that “younger and younger babies can survive,” said Kimberly A. Drenser, MD, PhD, who practices in Royal Oak, Mich. Nonetheless, the incidence of retinopathy of prematurity (ROP) has remained stable at about 15,000 cases annually—a huge credit, she said, to the management of the premature infant.
What has increased in recent years is controversy over the best way to manage ROP, a leading cause of blindness in premature children.1 Here is an overview of the pros and cons—and some nagging questions—associated with laser photoablation, the gold standard of treatment, and anti-VEGF therapy, the leading contender.
Laser Photoablation: A Well-Worn Path
In laser photoablation, scars are created in the peripheral retina to stop abnormal vessel growth.
Pro: Effective. “We know that laser treatment decreases the risk of unfavorable outcomes, mainly of retinal detachment, in 91% of children,” said Dr. Drenser. If a retinal detachment does occur following laser, early surgical intervention has a 90% success rate and is easier to perform than it is after anti-VEGF therapy, she added.
Pro: Predictable and stable. In the majority of cases, there is prompt regression after laser, usually within the first week, Dr. Drenser said. “If you’re not seeing that, you need to look carefully for a skipped lesion in the periphery, which will require more treatment, and watch for tractional retinal detachment at about the due date to 2 weeks after the due date [postmenstrual age of 40-42 weeks]. If you get to 50 weeks’ postmenstrual age without a complication, it will not happen with laser.”
Ophthalmologists know that visual and retinal structural findings tend to remain stable over time with no significant long-term complications, added Michael F. Chiang, MD, at Oregon Health & Science University in Portland.
Concern: Risks of anesthesia. Although Dr. Chiang uses IV sedation when performing laser for ROP, national surveys of ophthalmologists show that the majority use general anesthesia. “This is more invasive, and it can be a risk for babies who are very sick and small,” he said. However, Dr. Drenser said that this risk is less of a concern among pediatric anesthesiologists, who are comfortable with the modern techniques used with high-risk infants.
Concern: Visual fields. Testing has shown that permanent laser burns don’t affect central vision, but they do affect peripheral vision, said Dr. Chiang. “However,” said Graham E. Quinn, MD, MSCE, “we don’t have good data on whether visual fields are really that different with laser than they are with anti-VEGF therapy, since there are no reports, to my knowledge, of visual fields assessed after anti-VEGF treatment.” Dr. Quinn is at the University of Pennsylvania in Philadelphia.
Concern: Myopia. Some studies have reported that the babies who have had laser are highly myopic on average, said Dr. Chiang. For instance, BEAT-ROP found very high myopia in 51% with laser versus 4% with bevacizumab.2
Researchers in Denmark, however, report different results from those of American studies.3 They followed children for 4 years in the following groups: 1) Full-term infants, 2) premature infants with no ROP, 3) premature infants with ROP that regressed, and 4) those with ROP requiring laser. The only significant difference for refraction and visual acuity was found between full-term and premature infants, although there was a worsening of myopia in children who had ROP. “From this study, it appears that the greatest predictor of decreased vision and myopia is prematurity itself,” said Dr. Drenser.
Concern: Macula at risk? Potential laser ablation of the macula is a common concern, particularly in younger eyes with more disease posteriorly, said Dr. Drenser. With serial photography, her group showed that the posterior pole grows independently and in addition to the overall growth of the eye itself. “You don’t actually see laser scarring in the macula after about 3 months postlaser treatment.”
Anti-VEGF Therapy: The Road Less Traveled
Since the introduction of anti-VEGF therapy for ROP,4 ophthalmologists have debated whether its use is premature. “Our group was one of the first to start an anti-VEGF clinical trial, BLOCK-ROP,” said Dr. Drenser. “Our initial safety phase involved using anti-VEGF for those who had failed laser. After a year, we’d enrolled only 1 child from 11 centers in the United States, so we closed the study and concluded that laser works.”
Pro: Less trauma, faster response. Anti-VEGF injections are easier on the babies, said Dr. Quinn. “They can be done under topical, don’t require much sedation, if any, and take minutes instead of 30 to 40 minutes per eye to perform,” he said. “They also have an amazingly fast response—within 3 to 4 days—faster than what you see with laser.”
Concern: Follow-up challenges. One disadvantage of anti-VEGF therapy is that the disease often recurs weeks to months later, sometimes aggressively, putting babies at risk for retinal detachment, said Dr. Chiang. For this reason, the Ophthalmic Mutual Insurance Company decided to make the recommendation in the 2012 AAP/AAO/AAPOS Policy Statement a requirement: Infants treated for ROP with anti-VEGF drugs should be monitored weekly postinjection until there is full vascularization in close proximity to the ora serrata for 360 degrees.5 At this stage, babies may be at 60 to 70 weeks’ postmenstrual age, said Dr. Quinn, a point in time when examinations on an infant who is now active and strong become increasingly difficult.
When Dr. Chiang offers anti-VEGF treatment, he tells parents, “You must bring your baby back every 1 to 2 weeks for at least the next few months. If you are not willing or able to do that, we won’t do the injection.”
Concern: Systemic circulation. Multiple studies—mostly out of Japan—have reported that the systemic level of circulating VEGF, which is important to development, is suppressed for up to 8 weeks or longer after bevacizumab treatment in neonates, said Dr. Drenser.
Dr. Quinn suggested a way for ophthalmologists, neonatologists, pediatricians, and neurodevelopmental specialists to think about this issue: Laser has only a local effect, while anti-VEGF therapy potentially affects the entire body. “We really don’t know the long-term consequences,” he said. “And that’s what I worry about when we tell vessels to stop growing in the eye. We may be affecting vessel growth in the brain, kidneys, and lungs, and that is a big deal.” For example, Dr. Drenser said, treatment with bevacizumab can cause a worsening of bronchopulmonary dysplasia.
VEGF is also necessary for development of nerve tissues, including the retina. “In low doses, it is neurogenic as well as neuroprotective,” she said. “In addition to inhibiting pathological neovascularization, anti-VEGF therapy risks blocking normal angiogenesis and neurogenesis.”
Data from the Canadian Neonatal Network and Canadian Neonatal Follow-Up Network databases recently showed6 that babies treated with bevacizumab were comparable to those who’d had laser in terms of cognitive and verbal development at 18 months. However, they experienced a 3.3 times greater likelihood of significant motor delay, said Dr. Quinn. “Although the study wasn’t randomized, these results are concerning.”
Without the benefit of well-controlled clinical trials, said Dr. Drenser, physicians are largely relying upon anecdotal data. Nothing definitive has yet been shown with regard to systemic side effects, said Dr. Chiang. “The most rigorous published study [BEAT-ROP] reported 5 deaths in the bevacizumab group and 2 in the laser group,” he said, “but the study was underpowered to determine statistical significance.”
Concern: Visual changes. Until recently, Dr. Quinn’s worries were mostly limited to systemic risks. Then a group in Rome asked him to collaborate on a project including review of fluorescein angiography in babies with ROP. Images revealed persistent posterior pole abnormalities and peripheral leakage and vascular abnormalities in bevacizumab-treated eyes. This was much more common than in laser-treated eyes.7
Concern: Treatment protocols. Much more study is needed to determine the optimal drug for treatment as well as dosage and timing for best results. Dr. Quinn is participating in a dose-response trial of bevacizumab through the Pediatric Eye Disease Investigator Group.
Although this drug has received the most attention, others may work as well or better, Dr. Chiang added. For instance, ranibizumab, which is also being tested, may theoretically have less systemic risk due to a shorter half-life and lower levels of systemic absorption, he said.
What About Combination Therapy?
There’s another option for severe disease: laser plus anti-VEGF injections. Theoretically, this could address both VEGF circulating in the vitreous and VEGF generated in the peripheral avascular retina, said Dr. Chiang. “First, the anti-VEGF drug might neutralize the VEGF that’s floating in the vitreous. Then, the laser could stop the production of VEGF in the retina.” But there’s a downside, as laser disrupts the blood-retina barrier, which could allow more of the anti-VEGF drug to circulate systemically, he said.
Currently, Dr. Chiang uses laser if significant recurrence takes place after anti-VEGF therapy. “We generally don’t need to laser as much of the retina as we otherwise would have without anti-VEGF treatment.”
Although Dr. Quinn still considers laser the gold standard, he is receptive to the idea of combinations. “The way to go may be to first block abnormal vascularization with Avastin and then use laser to ablate the peripheral retina after vascularization has proceeded further out,” he said. “Then parents might not need to continue follow-up to age 70 weeks’ postmenstrual age.” However, he noted, “This concept still needs testing.”
Educate Parents!
One last critical point: When speaking with parents about the options, said Dr. Quinn, don’t just tell them what is happening at the moment; give them a broader perspective. “Tell them, ‘Here is what I don’t know about each type of treatment.’ Once you’ve done this, you can help make a reasoned clinical recommendation based on the baby’s condition.”
___________________________
1 Gilbert C. Early Hum Dev. 2008;84(2):77-82.
2 Geloneck MM et al. JAMA Ophthalmol. 2014;132(11):1327-1333.
3 Fledelius HC et al. Acta Ophthalmol. 2015;93(4):330-338.
4 Klufas MA, Chan RV. J Pediatr Ophthalmol Strabismus. 2015;52(2):77-84.
5 OMIC: ROP Supplemental Questionnaire. Accessed July 20, 2015.
6 Morin J et al. Abstract 4323 presented at: Association for Research in Vision and Ophthalmology Annual Meeting; May 6, 2015; Denver.
7 Lepore D et al. Ophthalmology. 2014;121(11):2212-2219.
___________________________
Dr. Dunn is professor of ophthalmology at Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and director of the uveitis unit of the retina division at Wills Eye Hospital. Relevant financial disclosures: None.
Dr. Nguyen is McGaw Professor of Ophthalmology, department chairman, and inaugural director of Truhlsen Eye Institute, at the University of Nebraska Medical Center, in Omaha. Relevant financial disclosures: AbbVie Pharmaceuticals: S; Bausch & Lomb Surgical: C; Genentech: S; Heidelberg Engineering: S; Lux Biosciences: S; Optos: S; Regeneron: S; Sanofi Fovea: S; Santen: C,S; Xoma: C.
Dr. Yeh is associate professor of ophthalmology, and director of the section of uveitis and vasculitis, section of vitreoretinal surgery & diseases, at Emory Eye Center, Emory University, Atlanta. Relevant financial disclosures: None.
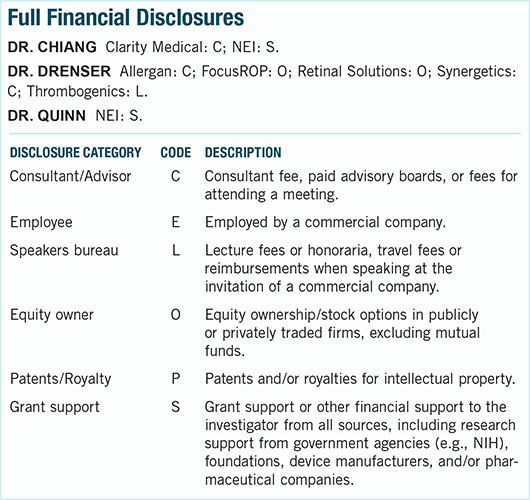
For full disclosures and the disclosure key, see below.