By Annie Stuart, Contributing Writer, interviewing Marjan Farid, MD, Nicole R. Fram, MD, and Lucy Q. Shen, MD
Download PDF
Aqueous misdirection related to ocular surgery is, most often, a postoperative phenomenon. Although intraoperative instances are considered rare, most busy cataract surgeons will experience this phenomenon a few times during their career, said Marjan Farid, MD, at the University of California in Irvine. When it does manifest during surgery, it can be confused with another alarming condition: suprachoroidal hemorrhage. “We don’t see aqueous misdirection very often, so it can take us by surprise. You have to keep it in the back of your mind, be vigilant, and do what you can to prevent or treat it,” said Lucy Q. Shen, MD, at Massachusetts Eye and Ear in Boston.
Armed with an understanding of the condition and awareness of risk factors, the surgeon can take steps pre-, intra-, and postoperatively to manage this potentially vision-threatening entity.
What Is Aqueous Misdirection?
Traditionally, the term aqueous misdirection describes a postoperative condition in which aqueous humor accumulates in the vitreous cavity, causing high IOP and uniform shallowing of the anterior chamber. It is also called malignant glaucoma.1
Irrigation misdirection. Similarly, intraoperative disruption of fluidic homeostasis can cause fluid from the anterior chamber to misdirect posteriorly, resulting in a shallow anterior chamber and elevated IOP. After ruling out a suprachoroidal hemorrhage, one can only assume that this is caused by infusion or irrigation misdirection, said Nicole R. Fram, MD, who practices in Los Angeles. This occurrence has also been referred to in the literature as acute intraoperative rock-hard eye syndrome.2 But some surgeons consider it a type of aqueous misdirection, said Dr. Shen.
 |
|
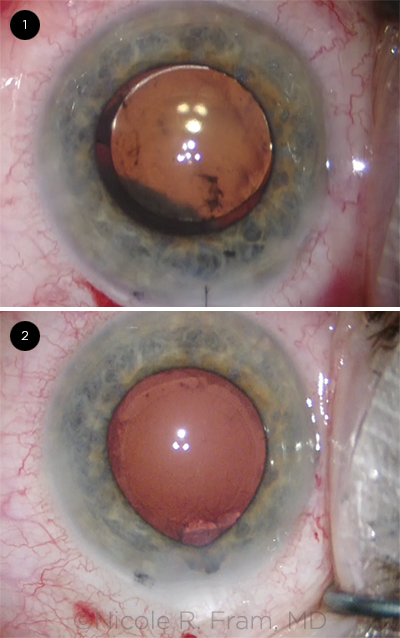
WHICH IS WHICH? (1) The shadow in the red reflex indicates a suprachoroidal hemorrhage. (2) Iris prolapse and anterior chamber shallowing, indicating aqueous misdirection.
|
Who Is at Risk?
Eyes at greater risk both intraoperatively and postoperatively include those with shorter axial length or angle closure, where the outflow pathway is narrow or already compromised, said Dr. Farid.
“Problems with the zonular apparatus may cause aqueous to travel back through the zonules and get trapped in the vitreous cavity,” said Dr. Farid. Eyes with compromised zonules tend to be those with pseudoexfoliation or uveitis, as well as those that have undergone laser iridotomy, vitrectomy, trabeculectomy, or insertion of a glaucoma drainage device, said Dr. Fram.
Notably, aqueous misdirection during a previous surgery confers increased risk for the fellow eye.1
The exact underlying mechanism of aqueous misdirection is unclear, but it is thought to involve an abnormal relationship between the ciliary processes, lens, anterior vitreous, and possibly choroid, causing aqueous to divert into the vitreous cavity.1
Preventive Steps
Careful planning for anterior segment surgery includes the following steps, said Dr. Shen.
Position the head. Before the patient is draped for surgery, make sure the head is positioned above the body. This can be done by inclining the torso slightly so that the patient is resting in a very elongated Z-shape. This positioning can decrease the risk of posterior pressure from the weight of the body, which is particularly important if the patient has a large body habitus, said Dr. Shen.
Elevate the speculum. Another way to lessen posterior pressure is to elevate the lid speculum a little, said Dr. Shen. “Put a couple of 4 × 4 gauzes underneath the speculum to reduce the pressure to the orbit and, consequently, the pressure on the globe.”
Minimize manipulation. When doing cataract surgery, the surgeon should minimize manipulation and get in and out as quickly as possible, said Dr. Farid. Also, creating a longer tunnel for the corneal incision helps to prevent iris prolapse and provides a tighter seal to help manage the situation, she said.
Inject viscoelastic. Dr. Farid recommends using a heavy cohesive viscoelastic in the anterior chamber to keep it formed throughout the case. In patients at risk for aqueous misdirection or suprachoroidal hemorrhage, Dr. Fram injects viscoelastic or balanced salt solution (BSS) every time she comes out of the eye to maintain a constant eye pressure and avoid abrupt IOP fluctuations.
Dr. Shen performs the same maneuver. “The idea is to prevent the posterior lens capsule from ever touching the cornea during the case,” she said.
Be gentle with inflation. If you inject BSS too forcefully, said Dr. Shen, it can be directed toward the vitreous and can result in irrigation misdirection. “Be gentle and watch the anterior chamber when inflating, so you don’t push too much fluid into the posterior part of the eye.”
Be watchful. Following phacoemulsification, Dr. Shen sometimes performs endoscopic cyclophotocoagulation to reduce IOP in patients with angle-closure glaucoma. “Even with this step, the patient is still at risk for intraoperative aqueous misdirection,” she said. Again, ensure that you have adequate viscoelastic to maintain anterior chamber depth, she said.
Considerations for fellow-eye surgery. In one case of fellow-eye surgery, Dr. Fram chose not to perform femtosecond laser because she wanted to avoid IOP fluctuation from suction and release. “And I did surgery under general anesthesia with paralysis to avoid any possibility of posterior pressure,” she said.
Dr. Shen advises considering the use of atropine at the beginning of the case and lining up a retina team in case a vitrectomy is needed.
Tube or Trab Surgeries: Trickier Cases
Certain procedures, such as a penetrating glaucoma surgery, are more challenging because of the inflammation that is often associated with aqueous misdirection, said Dr. Shen. Here’s what to remember in cases like these.
Reduce risks. In addition to keeping the anterior chamber deep during the surgery and at the end of the case, use preservative-free Kenalog for tube cases, said Dr. Shen. “Add a drop of atropine at the end of the case.”
Is it misdirection or overfiltration? “With postoperative aqueous misdirection, the pressure is usually high, and with overfiltration, the pressure is usually low and there are choroidal effusions on the dilated fundus exam,” said Dr. Shen. However, she noted that following tube placement, aqueous misdirection can have a normal or low IOP, because the tube continues to drain aqueous from the anterior chamber and the eye pressure measured by applanation of the cornea is not elevated.
In this case, there are some other differentiators: “First, with aqueous misdirection, there is no choroidal effusion because the pressure that is pushing the lens-iris diaphragm forward is also pushing the retina and choroid back,” said Dr. Shen. “Second, reinflation of the anterior chamber with viscoelastics is much more difficult: You need to exert significant pressure to inject the viscoelastics in the eye, and often much of the viscoelastic comes out of the paracentesis. The anterior chamber flattens again in one to two days. With overfiltration, by contrast, it is very easy to reinflate the anterior chamber and keep it deep, even in the presence of choroidal effusions.”
Don’t wait too long. Even when IOP is not high, advised Dr. Shen, treatment of aqueous misdirection is still urgent. “Because the lens is right up against the endothelial cells on the back of the cornea, they are at risk of failing,” she said. If aqueous misdirection cannot be managed medically or with a laser, consider pars plana vitrectomy combined with iridectomy and zonulotomy.
|
Intraoperative Strategies
It is important to recognize aqueous misdirection when it occurs during cataract surgery, to rule out suprachoroidal hemorrhage as the cause of positive posterior pressure and hardening of the globe, and to have a directed plan of action for its management, said Dr. Farid.
Watch for signs. “When strange things start happening during surgery—the iris keeps prolapsing, wound is leaking, eye pressure is going up, and anterior chamber is shallowing—you may not believe it at first,” said Dr. Farid. “Then it finally clicks in: This is aqueous misdirection.” In addition to these signs, the sclera feels very hard, added Dr. Shen, hence the term, acute intraoperative rock-hard eye syndrome.
Rule out other problems. Both a retrobulbar block—which increases the volume behind the globe and produces posterior pressure behind the eye—and a choroidal hemorrhage can mimic aqueous misdirection.
Suprachoroidal hemorrhage. To help confirm the diagnosis, look for a good red reflex, said Dr. Farid. If there is a darker reflex or a shadow on the red reflex (Fig. 1), that is indicative of a hemorrhage. The presence of pain also suggests hemorrhage. Those at higher risk for hemorrhage are patients who are older, have systemic hypertension, or are taking anticoagulation drugs or undergoing large-incision surgery, said Dr. Fram.
IFIS. Also, don’t confuse aqueous misdirection with intraoperative floppy iris syndrome (IFIS), in which only the iris comes out of the wound, said Dr. Shen. “The entire lens-iris diaphragm is pushed anteriorly in aqueous misdirection.”
The first question to ask yourself when the iris is prolapsing is whether the eye is soft or hard, said Dr. Fram. “If the eye is soft, it might be IFIS or poor wound construction,” she said. “If the eye is hard, it might also be IFIS; however, the bulging posterior capsule and movement of the entire lens-diaphragm complex should alert the surgeon to irrigation misdirection.”
Wait and come back. The surgeon can stop and use an indirect ophthalmoscope to evaluate whether a suprachoroidal hemorrhage is present and can assess the patient for pain, added Dr. Fram. If you suspect, or can’t confirm the absence of, a hemorrhage or large choroidal effusion—especially when the patient has no risk factors for zonulopathy or pseudoexfoliation syndrome—close the eye and come back, preferably after one week, she said, adding, “If it is a suprachoroidal hemorrhage and the surgeon places the trocar in the suprachoroidal space, the consequences can be devastating.”
Keep the patient comfortable—and pause. If you suspect aqueous misdirection, first make sure the patient is comfortable, said Dr. Shen. To help prevent any tensing or squeezing, use sedation if needed, and double-check that the speculum is not applying pressure. “At this point, I would ask the nurse to give atropine—if atropine was not given at the beginning of the case,” she said. “Just by waiting a bit, sometimes misdirection caused by irrigation will reverse itself.”
Equilibrate the chambers. A variety of maneuvers may help equalize pressure in the eye.
Use an air bubble. If you are using a very heavy viscoelastic to re-form the anterior chamber, said Dr. Farid, you can put an air bubble in the anterior chamber to push things back. “Then, stop for five to 10 minutes to allow decompression to occur before finishing the case.”
Drain fluid. You can use a needle to drain BSS that has traveled behind the capsule, said Dr. Shen. “To avoid touching the posterior capsule, measure 3.5 mm behind the limbus and visualize the needle as you enter behind the capsule.” She recommends starting with a 30-gauge needle and 1 cc syringe but suggests taking the plunger out so the pressure will equilibrate.
“The vitreous is not causing the problem intraoperatively, so technically you don’t need a vitrectomy with a large-bore needle,” said Dr. Shen. “All you need is to remove some of the misdirected fluid.”
Do a vitrectomy. Both Dr. Fram and Dr. Farid, however, would consider a pars plana vitrectomy after ruling out a suprachoroidal hemorrhage. “Aim toward the optic nerve with the trocar about 3.5 mm posterior to the limbus,” said Dr. Fram. In rare cases, where the anterior chamber is completely shallow, said Dr. Farid, you may make a small sclerotomy about 3 mm posterior to the limbus and use a small-gauge vitrector to perform a one- to two-second core vitrectomy. This will break the anterior hyaloid face and immediately release the trapped fluid.
Give mannitol. If the IOP is still over 30 mm Hg despite maneuvers, you can give mannitol at 1 g/kg, said Dr. Fram. “However, if IOP is normal, we want to avoid abrupt changes in pressure, which can cause more shearing of the choroidal vessels in the setting of suprachoroidal hemorrhage.” It’s important to be aware that mannitol can cause systemic complications, such as congestive heart failure or intracranial hemorrhage in at-risk patients, she said.
Get the AAO Mobile App
The new AAO Ophthalmic Education App features content from EyeWiki and the Diagnose This, News, and 1-Minute Videos areas of the ONE Network. Customize your feed and receive alerts based on your subspecialty preference.
Learn more at aao.org/education-app.
|
Postoperative Management
The likelihood of encountering aqueous misdirection increases after anterior segment surgery in at-risk patients.
Confirm the diagnosis. Confirmation of postoperative aqueous misdirection will show that the anterior chamber is shallow, the pressure is usually very high, and the lens is pushed up against the cornea, whether the patient is phakic or pseudophakic, said Dr. Shen. Dilated fundus exam or B-scan, if the view is hazy, can help rule out a choroidal effusion or hemorrhage, she added.
Although severe eye pain is uncommon postoperatively, patients may experience discomfort, redness, and decreased vision, said Dr. Fram, but aqueous misdirection is mainly a clinical diagnosis at the slit lamp. You can instill a cycloplegic eyedrop, such as atropine, in the patient’s eye to move the ciliary body back and measure anterior chamber depth and configuration with anterior segment optical coherence tomography. Ultrasound biomicroscopy can also help you look for anteriorization of the ciliary body, said Dr. Fram.
Wait and watch. If the pressure is not too high, you may be able to put an air bubble into the anterior chamber at the slit lamp and wait to see if the problem resolves, said Dr. Farid. Waiting too long is obviously not an option. If the condition persists, high IOP can damage the optic nerve, and contact between the cornea and lens or IOL may damage endothelial cells, she said.
Manage with medicine. Cycloplegics such as atropine and cyclopentolate can shift the lens-iris diaphragm posteriorly, said Dr. Shen. “Aqueous suppressants such as timolol and dorzolamide can decrease the amount of aqueous produced and lower the IOP. Also, steroid medication is helpful because aqueous misdirection is often associated with inflammation and swelling of the choroid. Frequent use of prednisolone acetate every one to two hours or use of a stronger steroid such as difluprednate can help to alleviate any inflammation and associated discomfort.”
Perform surgery. “The first step before undertaking a surgical procedure to relieve the pressure is to make sure there is no IOL-corneal touch,” said Dr. Fram. Then, she said, “You can perform an anterior chamber paracentesis and inject a cohesive viscoelastic to temporarily push the IOL complex posteriorly and away from the cornea.”
You can make an opening and communication between the iris and the vitreous through the peripheral capsule with an Nd:YAG laser, said Dr. Fram. “Or you can create this opening using a vitrector intraoperatively.” Whether you do the procedure in an office or in the OR depends upon the extent of the problem and the clarity of your view, she said.
___________________________
1 Moinul P, Hutnik C. Clin Ophthalmol. 2015;9:183-186.
2 Lau OC et al. J Cataract Refract Surg. 2014;40(5):799-804.
___________________________
Dr. Farid is clinical professor of ophthalmology; director of cornea, cataract and refractive surgery, Ocular Surface Disease Program; and vice chair of ophthalmic faculty, School of Medicine, University of California, Irvine, Calif. Relevant financial disclosures: None.
Dr. Fram is a cataract, cornea and external disease specialist at Advanced Vision Care; Clinical Instructor of Ophthalmology, Stein Eye Institute, University of California, Los Angeles. Relevant financial disclosures: None.
Dr. Shen is assistant professor of ophthalmology at Harvard Medical School; director of glaucoma fellowship at Massachusetts Eye and Ear, Boston. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Farid Allergan: C; Bio-Tissue: C; CorneaGen: C; Dompé: C; EyePoint: C; Eyevance: C; Johnson & Johnson Vision: C; Kala: C; Shire: C.
Dr. Fram Alcon: C,L; Allergan: C; Bausch + Lomb: L; CorneaGen: C,O; Johnson & Johnson: C,L; Ocular Science: C,O; RxSight: C; Zeiss: S.
Dr. Shen Allergan: C; Topcon: C,S.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|