By Michael Mott, Contributing Writer, interviewing Jeffrey D. Henderer, MD, Robert A. Mazzoli, MD, FACS, Charles F. Pattavina, MD, Christopher J. Rapuano, MD, and Robert E. Wiggins Jr., MD, MHA
Download PDF
A dangerous trend has been percolating in emergency medicine over the past few decades. Across all specialties, fewer and fewer physicians are willing to provide on-call coverage at hospitals, both for the emergency department (ED) and for inpatient consultations. As more community hospitals face the difficulty of obtaining specialty coverage, the burden is falling on academic medical centers to care for a growing number of transferred patients.
What role does ophthalmology play in this growing crisis? “Without a doubt this problem is occurring across many specialties,” said Charles F. Pattavina, MD, at St. Joseph Hospital in Bangor, Maine. “However, in my own experience—and I’ve heard this over and over—ophthalmology coverage does seem to be the biggest problem in most places.”
What’s Behind the Trend
Dr. Pattavina is well aware of the slow decrease in call coverage over the years, given his participation in the Maine Medical Association and the American College of Emergency Physicians. “This isn’t a generational thing either,” he said. “It’s part of how ophthalmology has evolved as a profession. It’s important to know why this is occurring and how all parties involved can help reverse the trend.”
Growth of ASCs. “Simply put, we don’t need to be affiliated with a hospital anymore in order to practice ophthalmology,” said Robert A. Mazzoli, MD, FACS, a retired ophthalmologist in Steilacoom, Washington, who serves as the ophthalmic consultant to the American College of Surgeons’ National Committee on Trauma. “The boom in ambulatory surgery centers [ASCs] has changed the game. We’re in our own private practices. We all have our own ASCs or use somebody else’s to perform most of our procedures. And so we no longer require hospital privileges to either perform surgery or build a successful practice via patient referrals. As a result, we’re excused from any mandates and required participation in hospital call rosters.”
Outdated ED equipment? Unease regarding surgical equipment is also an issue, said Dr. Mazzoli. “As ophthalmologists, we’re chasing the most up-to-date technology.” But because ophthalmology has shifted away from the hospital, “there is little motivation for the hospital to equip itself with what we would consider state-of-the-art equipment.” Thus, he asked, even if the facility has “basic diagnostic and therapeutic ocular equipment, do I feel comfortable evaluating or repairing an open globe if there is no ultrasound in the ED, or the slit lamp is of poor quality and unserviced, or the microscope is 15, 20, or 30 years old? Does the OR have the right supplies, well-kept instruments, and experienced techs?”
Growth of specialization. Ophthalmology’s focus on expertise is also stifling ED call, said Jeffrey D. Henderer, MD, at the Lewis Katz School of Medicine at Temple University in Philadelphia. “Many of us have specialized in one particular aspect of ophthalmology and have become very good at that [sub]specialty. But ED call is almost by definition going to be a jumble of injuries that fall outside many ophthalmologists’ wheelhouse. For example, if an oculoplastic subspecialist is unfamiliar with globe trauma, repairing a ruptured globe might just be too far out of his or her comfort zone. By the same token, a cataract surgeon might feel ill-equipped to handle eyelid or tear duct trauma.”
 |
|
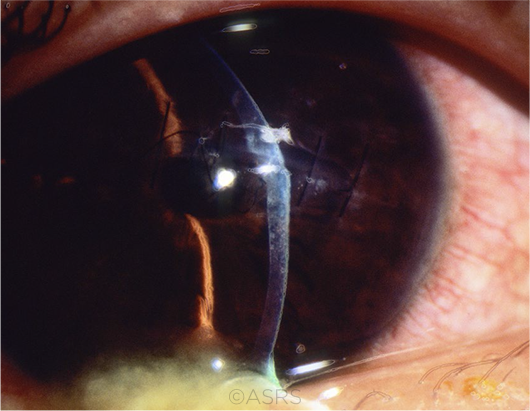
TRAUMA. When’s the last time you repaired a corneal laceration? This patient’s injury occurred during a game of basketball. This image was originally published in the ASRS Retina Image Bank. David Callanan, MD. Corneal Laceration/Repeat Trauma. Retina Image Bank. 2013; Image Number 12657. © The American Society of Retina Specialists.
|
What’s at Stake
A study by the CDC found that approximately 1 in 5 unanticipated events resulting in death or serious injury in hospital EDs could be attributed to the absence of specialty services.1 “As doctors in general, it’s our obligation to care for patients and try to prevent these types of occurrences,” said Christopher J. Rapuano, MD, at Wills Eye Hospital in Philadelphia. “The public has an expectation that a certain level of quality care will be available to them any time of the day. It’s our responsibility to provide ophthalmic specialty care 24/7. We all need to share in this duty. When only a few ophthalmologists take call, it’s a huge burden on a relatively small number of physicians.”
Optometry makes inroads. If ophthalmologists continue removing themselves from emergency medicine and remain unwilling to provide care outside of their offices, be warned, said Dr. Mazzoli: Doing so is only creating a void that others will be more than happy to fill. And they have made their intentions clear. Most recently, optometry has organized alongside the University of Massachusetts Medical School to push for an ED avoidance model in which certain patients would be diverted to the care of ODs in order to avoid stretching EDs’ already strained resources.
“This is a serious situation,” said Dr. Mazzoli. “Optometrists and nonophthalmic providers are organized and ready to jump in. They see the gap in care. If a hospital can’t depend on ophthalmologists, why wouldn’t they send patients elsewhere? Why wouldn’t optometrists become the gatekeepers?”
As the American Optometric Association states, “The expanding scope of optometric practice, wide geographic distribution of optometrists, and force of health care reform have made the services of optometrists attractive to hospitals.”2 But as Dr. Pattavina pointed out, this is not the preference of hospital staff. “At St. Joseph, yes, we developed a workaround that involves ODs when MDs weren’t available—but that’s not what we want. Fortunately, a local ophthalmology group stepped up at the last minute, so we didn’t have to resort to that plan.”
Dr. Pattavina noted, “When we need help with an eye emergency, I can tell you with certainty that all of the emergency physicians want an ophthalmologist nearby rather than an optometrist.” From a practical perspective, he added, “We rarely need the consultants to [physically] come in; the vast majority of our calls are for advice or follow-up.”
Getting Back in the Game
Given the need for ophthalmology to reestablish its presence, what are some strategies to improve systems for emergency care and also reduce the ED call burden for everyone involved?
“There will be different solutions for different communities,” said Robert E. Wiggins Jr., MD, MHA, at Asheville Eye Associates in Asheville, North Carolina. “There’s really not a one-size-fits-all strategy. But any successful solution will begin and end with solid communication.”
A regional approach. At a broad level, a capabilities-based assessment can be a very useful approach to identify the needs and gaps in the delivery of care, said Dr. Rapuano.
This approach involves getting all important community stakeholders together—ophthalmologists in private practice and in academia, emergency physicians, OR staff, hospital administrators—to see what’s missing and what’s causing the problem. Is it manpower? Are patients not being seen in the correct facility? Are they going to the ED when they should be coming into the ophthalmologist’s office? Is specific equipment needed in the ED?
“This give-and-take approach is most effective when you have all of the numbers out in front of you,” said Dr. Rapuano. “So, we’ve got X number of operating rooms, X number of ophthalmologists, X number of residents, and so on. Over the past X number of years, we’ve had X number of ophthalmic emergencies and X number of ruptured globes and corneal abrasions. How can we solve the equation in a way that is fair and kind for patients, hospitals, and doctors?”
Shared call pools. Another regional strategy might be the most obvious, said Dr. Henderer, and that’s developing shared call pools among providers. “Plain and simple, we need to get more ophthalmologists in the pool—whether they are employed as part of a health system, in private practice, or residents,” said Dr. Henderer. “The more ophthalmologists involved, the less the burden on each individual.” For example, in northern Delaware, a group of about 18 ophthalmologists, many of whom are in their own separate private practices, cover call for each other on weekends. “They take call three to four weekends a year, and it’s been successful,” said Dr. Henderer.
Dedicated regional centers? Another option would be to establish regional centers that would be dedicated to the care of eye trauma. Under this model, ophthalmologists would share call at a single location where everything necessary to provide optimal care is available.
In addition to this central facility, Dr. Mazzoli said, “a regional system would identify facilities of varying capabilities that would be resources for both the EDs and responding ophthalmologists. In that way, a regionally designated facility could act as the initial advice center for the EDs, which could call that facility—similar to calling a regionally designated poison control center.” Additionally, he said, “an ophthalmologist in a poorly served location could call the more sophisticated regional facility for specific advice as well as to establish early communications for transfer, if needed.” This sets up a tiered system of capabilities that could be designated in a manner similar to the way the American College of Surgeons has designated Level 1 trauma centers, he said.
Telemedicine. Evaluating patients remotely offers another option for serving on call. “At Temple University, we have a HIPAA-compliant texting service (TigerConnect) through which we can take photographs and video of patients and share with residents, faculty, and ED staff,” said Dr. Henderer.
The immediate transfer of knowledge is a major benefit. “For example, in a case of major trauma, an ED resident or physician sends me external photos and ultrasound video so I can quickly evaluate and relay what steps they have to perform right now and what can wait until an ophthalmologist arrives.”
Military ophthalmology. Surgeons in the U.S. Armed Forces are interested in providing more trauma care during peacetime to increase their readiness for treating war-related injuries. Could this be a win-win solution for both community hospitals and military ophthalmologists? “It’s certainly holds promise,” said Dr. Mazzoli. “And it’s a situation that currently only exists at the Brooke Army Medical Center in San Antonio, where military surgeons are providing care to the community at large. Can that model be expanded across the country? Yes, but it will take national legislation.”
Academy Resources on Trauma Care
Trauma care shouldn’t give you pause, said Dr. Henderer. “When I first joined Temple University, I hadn’t repaired a ruptured globe in more than 10 years. Like anything else we do, repairing a globe is a skill that can be learned and taught.” And the Academy is updating selected member benefits with easily accessible primers on the most common conditions you’ll encounter in the hospital ED.
- The Wills Eye Manual. For more than two decades, this resource has offered authoritative guidance for treating ocular disorders in hospital and emergency settings. It’s now available online on the Ophthalmic News & Education (ONE) Network at aao.org/the-wills-eye-manual and will be added to the Academy’s Clinical Education app in the future.
- On-demand videos. For surgical cases that are especially complicated, members can search the ONE Network for how-to videos relating to emergency care.
- Help in a hurry. The Academy is exploring an “on call” feature to help ophthalmologists when they need it the most. At the push of a button, the above emergency-related resources would become immediately available on the Clinical Education app for easy, on-the-go browsing.
- Compensation survey. For results of the survey of fair market value for call compensation, go to aao.org/practice-management/analytics#survey.
|
Negotiating ED Call
Traditionally, many ophthalmologists have provided uncompensated call coverage. But any time spent away from private practice to take ED call could have an impact on practice profitability, which is of concern in today’s era of decreasing reimbursements and current economic pressures. As a result, an increasing number of ophthalmologists are negotiating with hospitals for emergency coverage compensation.
“Traditionally, most of us haven’t been in a very good bargaining position with hospitals,” said Dr. Wiggins. “They have the size, the resources, and the data. But that’s no longer the case. The Academy is now providing members with access to the results of a recent survey assessing fair market value for call compensation across medicine. You can view what hospitals are currently paying ophthalmologists relative to other specialists as well as other important benchmarking data points to arm yourself with as you enter negotiations.”3
But as Dr. Henderer pointed out, many hospitals have a fraught relationship with paying for call, so prepare yourself for an uphill battle. “They would rather not pay for what they are used to getting for free. But it’s really a matter of letting the hospital know that your own practice requires revenue generation and that any time away from your practice isn’t cost-effective unless you get reimbursed for it.” Thus, you’ll need to collect your own data. A good starting point for any negotiation is knowing what your fixed costs are and how much compensation you require to cover these costs if you’re out of the office.
Additional factors. There are many other variables in addition to financial compensation to keep in mind when negotiating a contract for ED call, said Dr. Rapuano. “You’ll need to know the hospital’s medical staff guidelines to determine how often call may be required, how quickly you’ll need to respond to a call, how many surgeries you will typically need to perform when on call, and whether or not you need additional malpractice coverage.”
Perhaps most importantly, you’ll also need to be familiar with the equipment and resources that will be available. “ED care is difficult enough given the late hours and urgent circumstances,” said Dr. Rapuano, “so you’ll want an operating room that you’re comfortable with for delivering a certain quality of care.” Will you have a vitrectomy machine, an indirect ophthalmoscope, a tonometer, or even a simple eye chart? Will you have dilating drops, sutures, and surgical drapes, or are these your own responsibility?
“It’s also vital to know if the hospital will have a scrub nurse available who is acquainted with ophthalmology,” Dr. Henderer added. “Being in an OR alongside someone who is unfamiliar with the anatomy of the eye or the necessary surgical instruments is a huge barrier to physician enthusiasm. In those circumstances, call can become somewhat of a DIY experience for the surgeon.”
Healing a Rift
The withdrawal of ophthalmology from ED hospital call can have implications for your practice. It can affect recredentialing from certain third-party payers or can have a negative impact on referrals and patient volume.
“But let’s not forget the potential damage on our professional reputation and our collegiality with other specialties,” said Dr. Rapuano. “If we want to set ourselves up as being the experts in the eye, our response to our colleagues asking for help can’t be ‘not tonight’ or ‘I’m an expert in the eye but not that section of the eye.’” This disconnection from the hospital-based side of clinical care is precipitating the risk of other areas of medicine looking unfavorably at ophthalmology in general, added Dr. Mazzoli. “But we can repair that rift. If we can re-evaluate our responsibility in taking call, we can rejoin the house of medicine, so to speak. We can regain the support of our fellow surgeons as they rely on us to provide ophthalmic care to all patients in need.”
___________________________
1 Krueger KJ, Halperin EC. Acad Med. 2010;85(12):1840-1844.
2 www.aoa.org/Documents/optometrists/facts-about-optometric-services-in-hospitals.pdf. Accessed Oct. 25, 2019.
3 BFMV Physician Call Coverage Burden and Compensation 2019 Survey. Available at aao.org/practice-management/analytics.
___________________________
Dr. Henderer is the Dr. Edward Hagop Bedrossian Chair of Ophthalmology at the Lewis Katz School of Medicine at Temple University in Philadelphia. Relevant financial disclosures: None.
Dr. Mazzoli is a retired U.S. Army ophthalmologist in Steilacoom, Wash. He also serves as the ophthalmic representative to the American College of Surgeons’ National Committee on Trauma. Relevant financial disclosures: None.
Dr. Pattavina is an emergency physician at St. Joseph Hospital in Bangor, Maine. He is also past president of the Maine Medical Association and a former board member of the American College of Emergency Physicians. Relevant financial disclosures: None.
Dr. Rapuano is chief of the Cornea Service at Wills Eye Hospital in Philadelphia. Relevant financial disclosures: None.
Dr. Wiggins specializes in pediatric ophthalmology and neuro-ophthalmology and serves as the physician administrator for Asheville Eye Associates in Asheville, N.C. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Henderer NEI/NIH: S.
Dr. Mazzoli None.
Dr. Pattavina None.
Dr. Rapuano Avedro: C; Bio-Tissue: C,L; GlaxoSmithKline: C; Kala: C; Novartis/Alcon: C; Rapid Pathogen Screening: O; Shire: C,L; Sun Ophthalmics: C; TearLab: C.
Dr. Wiggins OMIC: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|