By Linda Roach, Contributing Writer, interviewing John S.M. Chang, MD, Soosan Jacob, MS, FRCS, DNB, Edward E. Manche, MD, and Kevin M. Miller, MD
Download PDF
Over the last decade, SMILE has become the refractive surgery of choice for treating many myopes around the globe—except in the United States. That’s because the FDA’s initial indications for the only laser that can perform the procedure (VisuMax, Carl Zeiss) restricted U.S. surgeons to correcting cylinder of –0.50 D or less.
In October 2018, however, the FDA removed this roadblock. Now, U.S. refractive surgeons can use SMILE (which stands for small incision lenticule extraction) to correct myopia from –1.00 D to –10.00 D, with astigmatism of –0.75 to –3.00 D.
That makes SMILE “much more useful, because the majority of patients who present for refractive surgery have astigmatism as well as myopia. So, you can now treat 95% of refractive errors with SMILE,” said Edward E. Manche, MD, at Stanford University in Palo Alto, California.
Impact: Cues From Asia
The impact that SMILE might eventually have on the U.S. refractive surgery landscape is best illustrated in China and other Asian countries, where myopia prevalence is high.
After a decade of VisuMax availability in China, more than 50% of the laser vision corrections there are SMILE procedures, and this number is likely to rise further, said John S.M. Chang, MD, at the Hong Kong Sanatorium & Hospital. “Researchers are now looking into customizing it, the way we do in LASIK with the excimer laser,” Dr. Chang said.
 |
|
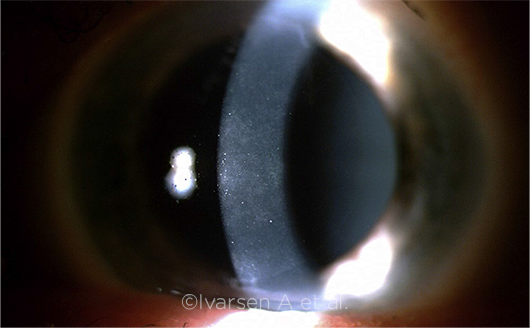
POST-OP ACUITY. Visual acuity following SMILE typically recovers after the cornea has fully healed, as it did in this patient (note initial post-op haze).
|
Procedural Overview
With SMILE, the surgeon uses a femtosecond laser to incise a lenticule of intrastromal tissue 120 μm deep in the cornea. The lenticule is then separated from the adjacent stroma and removed manually through a 2-to 4-mm tunnel incision, which changes the cornea’s shape and refractive power. Except for the small incision, the stromal fibrils and epithelium of the anterior corneal “cap” remain undisturbed, and Bowman’s layer is preserved as a continuous layer.
The lenticule’s thickness determines the amount of refractive correction from the procedure: approximately 13 to 14 μm per diopter, said Soosan Jacob, MS, FRCS, DNB, of Chennai, India. “Dissecting and removing the lenticules, some of which are quite thin, involves a learning curve. But [the procedure] is not difficult as long as you take the time to know what you’re doing,” she said.
Visual outcomes. With regard to early visual recovery, “You have a mild reduction in the ‘wow’ factor” with SMILE, Dr. Manche said. That’s because final post-op acuity usually takes several days to develop with SMILE, in contrast to the typically good visual acuity (VA) on day one with LASIK.
Longer term, several meta-analyses have found no statistically significant differences between SMILE and LASIK when VA is measured after the cornea has healed, Dr. Chang said. These include mean uncorrected distance visual acuity (UDVA); percentage of eyes losing ≥1 lines of corrected distance VA (CDVA); mean post-op refractive spherical equivalent refractive error; and post-op refraction ±1 D of target, he said.
With regard to recent prospective studies, in a study of 70 patients, outcomes observed with SMILE were similar to those seen with LASIK at both the three-and 12-month marks.1 In another study of 70 patients, visual outcomes and centration were comparable between the SMILE and LASIK eyes, although the functional optical zone was larger in SMILE eyes.2
Benefits
No LASIK flaps. SMILE eliminates flap-related complications like postoperative striae and late flap dislocations, and it results in fewer problems with dry eye in the early post-op period, Dr. Manche said. The procedure also is thought to have less of an impact on the cornea’s biomechanical strength than LASIK does, to sever fewer corneal nerves, and perhaps to reduce the risk of ectasia, especially in higher myopes, he said.3,4 However, these hypotheses have yet to be definitively confirmed.5
Better refractive predictability. SMILE also appears to offer better potential predictability of the post-op refraction, because corneal dehydration is not an issue, said Kevin M. Miller, MD, at the University of California, Los Angeles.
“When you do LASIK, as soon as you lift the flap the cornea beneath starts to dry out. The clock starts ticking, so you can get variable effects just from variable drying of the cornea. The drier the cornea gets for the exact same treatment, the greater the change is going to be in the cornea’s refractive power, because every laser pulse evaporates more tissue when the tissue is dry,” Dr. Miller said.
“This is actually a pretty huge issue, especially for the high corrections. When you’re doing a very high LASIK correction, you’re spending a lot of time with the flap off, and that drying effect can be very substantial on the final refractive outcome,” he said. “But you don’t have that with SMILE, because you’re making the entire cut with the cornea unexposed to the air.”
Greater patient acceptance. One of SMILE’s strengths, in Dr. Chang’s experience, is that it offers patients a better experience overall. To begin with, because there is no large corneal wound, patients do not have the foreign body sensation or excessive tearing that commonly occur in the first few hours after LASIK, nor do they experience persistent dry eye, he said.
The second advantage he sees is anecdotal: Patients have a lower “fear factor” with SMILE than with femtosecond LASIK, because of the time lag between the laser flap creation and the excimer laser ablation. With LASIK, he said, “after you do the first part—the femtosecond laser cut—you move them to the excimer, and by then the cavitation [bubbles] have gone away, so they can see your instruments moving and separating the tissue as you lift the flap. People just don’t like having a doctor come at their eyes with sharp instruments. It makes them very scared.”
But with SMILE, Dr. Chang said, “all those bubbles are still there, so they cannot see what you’re doing as you come in with your surgical instruments and remove the lenticule. They aren’t as frightened.”
Challenges
Loss of suction. As with LASIK, and especially during a surgeon’s earliest cases, there is a small risk that the laser’s applanation cone will lose suction midway through a SMILE procedure, Dr. Jacob said. If this happens, there is a definite protocol to follow, and in most—but not all—cases, the surgeon can proceed with SMILE. Some cases might need to be converted to LASIK or PRK.
Zeiss is addressing this issue through training, Dr. Miller said. “The company, and I think wisely so, won’t train you to be certified for SMILE until you’ve cut 50 flaps with the laser.” (Of note, this will pose a challenge for surgeons who primarily do PRK and wish to convert to SMILE.)
Difficulties with lenticules. Low myopic SMILE corrections are the most challenging for the surgeon, because the lenticules are thin and fragile, and the surgeon must avoid tearing them and leaving torn tissue behind, Dr. Jacob said. “You just have to keep the proper techniques for handling the lenticules in mind.”
Dr. Jacob added that surgeons “should make sure to dissect the anterior surface first, followed by the posterior surface. This prevents cap tears. And then you have to be sure to get the full lenticule out, or you can get irregular astigmatism.” She has developed several surgical tips and a series of YouTube videos about SMILE; two are available at www.youtube.com/watch?v=xSq0jEYW8GM and www.youtube.com/watch?v=K4fMhvHyi7o.
Need for retreatments. SMILE is so precise that enhancements are rarely required. For instance, Dr. Chang’s unpublished analysis of his first 444 cases at his surgical center showed that 90.1% of eyes had UDVA of 20/20 or better, and 98.7% were at least 20/25.
However, if a patient is dissatisfied and wants an enhancement, many surgeons advocate doing this with PRK, Dr. Manche said. “I’m not keen on cutting a LASIK flap on top of the SMILE cap, because then you have multiple planes of incision on the cornea. So I typically perform PRK for SMILE enhancements.” But some surgeons have reported successfully retreating undercorrected eyes by using SMILE plus LASIK, to correct as little as 0.5 D of refractive error, Dr. Chang said.
Fewer 20/20 outcomes? For now, as some research has demonstrated,6 topographically guided LASIK may be more reliable than SMILE at giving more patients a VA of at least 20/20, Dr. Chang said. He also steers those patients who have a lot of higher-order aberrations preoperatively toward LASIK, “because we know how to correct those with LASIK.”
Dr. Chang expects the VA gap to narrow when researchers develop customized SMILE algorithms. However, even if that does not happen, the small differences in VA will not dissuade an increasing number of his patients from choosing SMILE over LASIK, he said. “In my view 20/25 is still very good for our patients, because in Hong Kong and China most people don’t drive,” he said. “When you don’t drive, especially at night, 20/20 is not that important.” As a result, he said, he is comfortable with recommending either procedure.
Financial barriers. The cost of acquiring a VisuMax femtosecond laser (more than $500,000) is the primary barrier that refractive surgeons face when considering SMILE. In most practices, this is passed on to patients as a premium price for the surgery.
But Drs. Manche and Miller said they want patients to choose their corneal refractive surgery based on weighing the pros and cons of each procedure, not on the price tag. Thus, the fee for laser vision correction at their centers is the same for PRK, LASIK, and SMILE.
The Road Ahead
Correcting hyperopia. So far, myopia and astigmatism are the only approved uses of the VisuMax laser for SMILE procedures. But a few groups are experimenting with correcting hyperopia by extracting stromal lenticules that have a central dimple, Dr. Chang said. For instance, earlier this year, Reinstein et al. published their three-month results from hyperopic SMILE in 82 eyes. For the 36 eyes targeted for emmetropia, UDVA was 20/40 or better in 89%.7
Transplanting the lenticules. Rather than tossing away the stromal tissue extracted during SMILE, Dr. Jacob and her colleagues have been exploring ways to transplant the lenticules onto damaged corneas, to jump-start healing of conditions such as corneal ulcers, she said. The lenticules also can be reshaped and implanted as corneal inlays for alleviating presbyopia.8
The Bottom Line
Any refractive surgery has pluses and minuses, but in the case of SMILE, the research supports giving it a place in refractive surgery.
“I tell patients that the visual acuity with SMILE is not quite as good as after custom LASIK, so if you really want the best possible VA results, then you should have LASIK. But I add that SMILE gives you fewer dry eye problems and is more comfortable,” Dr. Chang said.
Overall, Dr. Manche said, “I think SMILE is an incredibly safe procedure. I don’t think there are any glaring deficiencies with this technology. There are a few caveats to note. But there’s no deal stopper in any of this.”
___________________________
1 Ang M et al. Ophthalmology. Published online Sept. 12, 2019.
2 Damgaard IB et al. J Refract Surg. 2019;35(4):230-237.
3 Lau YT. Ophthalmol Ther. 2019;8(3):373-386.
4 Guo H et al. BMC Ophthalmol. 2019;19(1):167.
5 Khamar P et al. J Refract Surg. 2019;35(5):324-332.
6 Kanellopoulos AJ. J Refract Surg. 2017;33(5):306-312.
7 Reinstein DZ et al. J Refract Surg. 2019;35(1):24-30.
8 Jacob S et al. J Refract Surg. 2017;33(4):224-229.
___________________________
Dr. Chang is director of refractive surgery at the Hong Kong Sanatorium & Hospital; clinical associate professor of ophthalmology at Hong Kong University; and clinical associate professor of ophthalmology at the Chinese University of Hong Kong. He is also president of the International Society of Refractive Surgery. Relevant financial disclosures: Carl Zeiss: L.
Dr. Jacob is director and chief of Dr. Agarwal’s Refractive and Cornea Foundation and senior consultant in the cataract and glaucoma services at Dr. Agarwal’s Group of Eye Hospitals in Chennai, India. Relevant financial disclosures: None.
Dr. Manche is director of cornea and refractive surgery and director of research, cornea, and refractive surgery at the Byers Eye Institute and professor of ophthalmology at Stanford University in Palo Alto, Calif. Relevant financial disclosures: Carl Zeiss: C,S.
Dr. Miller is the Kolokotrones Chair in Ophthalmology and chief of cataract and refractive surgery at the Stein Eye Institute at the University of California, Los Angeles. Relevant financial disclosures: Alcon: C; ianTech/Zeiss: C; Johnson & Johnson: C.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Chang Alcon: L; Carl Zeiss: L; Johnson & Johnson: L.
Dr. Jacob Morcher: P.
Dr. Manche Alcon: S; Allergan: S; Avedro: C,S; Best Doctors: C; Carl Zeiss: C,S; Clarity Vision Technologies: C,O; Guidepoint: C; Johnson & Johnson: C,S; Ocular Therapeutix: S; Presbia: S; RxSight: O; Shire: C; Vacu-Site: O,P.
Dr. Miller Alcon: C; Bausch + Lomb: O; ianTech/Zeiss: C; Johnson & Johnson: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|