The purpose of this guide is to educate ophthalmologists on how to meet the requirements of the quality category of the Merit-Based Incentive Payment System using Medicare claims reporting. Failure to successfully participate in MIPS in 2023 will lead to a 9% penalty on all Medicare Part B payments in 2025. This translates into an average penalty amount of $25,300 for an average ophthalmologist, so participation is in your best interest. Three things to consider before reading:
- Penalty vs. bonus: This guide is focused on helping ophthalmologists in small practices (≤ 15 clinicians) report the quality category of MIPS via claims. In 2023, this will not be enough on its own to avoid a penalty or earn a bonus. If you would like to learn how to meet your larger MIPS goals, refer to the Solo and Small Practice section of the 2023 MIPS Roadmap.
- Small practice vs. large practice: In the MIPS quality category, only clinicians in small practices (≤ 15 clinicians) may submit data via claims. Clinicians in small practices can report MIPS as a group or as individuals and still use claims for quality reporting. Beginning in the 2023 performance year, CMS will only calculate a group-level quality score from Medicare Part B claims measures if the practice submits data for another performance category as a group (signaling their intent to participate as a group).
- Is claims-based reporting the best option for you or your group: The Academy recommends its IRIS® Registry for quality reporting. It is a free member benefit and is tailored to ophthalmologists. In addition, the IRIS Registry Web Portal manual reporting option does not require reporting in real time as claims-based reporting does, and there is less uncertainty as you are able to track the patients and quality measures on which you report. The IRIS Registry has QCDR measures that can only be reported through the registry and can earn up to 10 points per measure. Under claims-based reporting, CMS only confirms on remittance advice that the submission was received, but not that it was successful.
Minimum Reporting
In the 2023 performance year, the threshold to avoid a penalty is a 60-point minimum MIPS final score. All clinicians in small practices (≤ 15 clinicians) can avoid the payment penalty by fulfilling all of the following requirements:
- Practices that match either of these two criteria: multi-specialty (not just ophthalmologists and ODs) practice OR if you perform cataract surgery. Do all of the following:
- Quality category: Report on at least 6 quality measures, 1 of which must be an outcome measure.
- Small Practices without EHR:
- You must average at least 6.50 out of 10 points on all measures (assuming 50% in the cost category).
- Fully report (on at least 70% of denominator-eligible* patients AND with at least 20 patients in the denominator) for all 6 quality measures;
- Small Practices with EHR:
- You must average at least 7.33 out of 10 points on all measures (assuming an 80% in the PI category and 50% in cost).
- Fully report (on at least 70% of denominator-eligible* patients AND with at least 20 patients in the denominator) each quality measure.
- The IRIS Registry reports on 100% of denominator-eligible patients for IRIS-EHR integrated practices.
- Improvement activities category: Complete 1 high-weighted or 2 medium-weighted improvement activities for 90+ consecutive days. If group reporting, at least 50% of eligible clinicians in your group must complete the same activity(ies).
- Promoting interoperability category:
- If you have 2015 certified electronic health record technology (CEHRT), 2015 Cures Edition CEHRT, or a combination of both, complete the PI required measures and try to maximize your performance where possible.
- If you do not have a 2015 or 2015 Cures Edition certified EHR, small practices are now automatically excluded from the PI category unless they report 2022 PI data to CMS.
- Practices that meet both of these two criteria: Follow these steps if you are in an eyecare only practice that does not perform cataract surgery, your cost category score should be reweighted to the quality category. Do all of the following:
- Quality category: Report on at least 6 quality measures, 1 of which must be an outcome measure.
- Small Practices without EHR:
- Fully report (on at least 70% of denominator-eligible* patients AND with at least 20 patients in the denominator) for all 6 quality measures;
- You must average at least 4 out of 10 points on all measures.
- Small Practices with EHR:
- Fully report (on at least 70% of denominator-eligible* patients AND with at least 20 patients in the denominator) each quality measure.
- The IRIS Registry reports on 100% of denominator-eligible patients for IRIS-EHR integrated practices.
- You must average at least 5.6 out of 10 points on all measures (assuming a PI score of 80%).
- Improvement activities category: Complete 1 high-weighted or 2 medium-weighted improvement activities for 90+ consecutive days. If group reporting, at least 50% of eligible clinicians in your group must complete the same activity(ies).
- Promoting interoperability category:
- If you have 2015 certified electronic health record technology (CEHRT), 2015 Cures Edition CEHRT, or a combination of both, complete the PI required measures and try to maximize your performance where possible.
- If you do not have a 2015 or 2015 Cures Edition certified EHR, small practices are now automatically excluded from the PI category unless they report 2022 PI data to CMS.
*For example, for the diabetic retinopathy measures, “denominator-eligible patients” means all patients between the ages of 18 and 75 years with diabetes.
Find the Right Measures
- Visit the MIPS Quality Reporting page on the Academy website. Visit the page on the Academy website. Here, you will see the quality requirements for MIPS.
- Review the measures. Visit the CMS MIPS quality measures page to review the available claims measures. In the performance year field use the drop down menu to select “2022”. Then scroll down to the search field and use the collection type drop down to filter the measures to “Medicare Part B claims measures”. Here you will be able to peruse the available claims measures and download the specifications of the ones you are interested in reporting.
Your measure score depends on two components: the numerator and the denominator.
- Denominator: To include a patient in the denominator, the case must meet three criteria:
- Patient characteristics: Defined in the "Description" section.
- Diagnosis codes (ICD-10-CM): Codes located in “Diagnosis Codes.”
- Procedure codes (CPT or HCPCS): Codes located in “CPT Codes.”
The quality measure may also have exclusions for the denominator.
- Numerator: The numerator is based on Quality Data Codes (QDCs) which are organized into one of four categories.
- Denominator exclusion: Patient is ineligible to be measured. Patient is not included in the numerator nor the denominator.
- Performance met: Include patient in numerator and denominator
- Denominator exception: Patient is eligible to be measured, but there is a medical reason for not performing the numerator criteria. Do not include patient in numerator nor denominator.
- Performance not met: Include patient in denominator, but not in the numerator.
Report the Measures
Once you have chosen the measures needed to meet the minimum MIPS reporting requirements, follow these steps to report by claims.
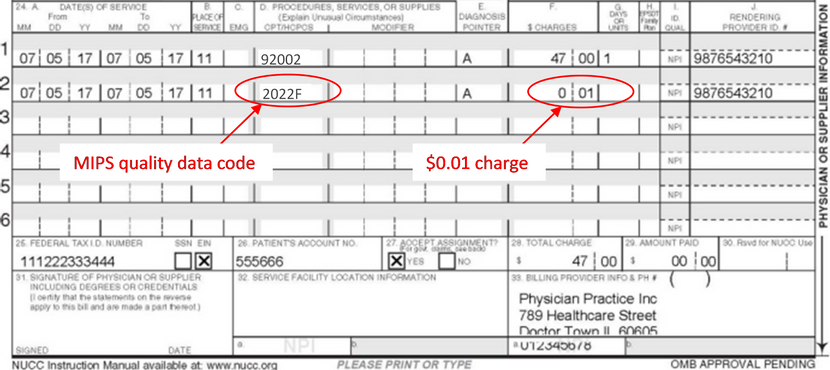
- Report on quality measures on a regular CMS 1500 Medicare Part B Claim.
- Identify a patient encounter that is relevant to your selected quality measure (or vice versa) and add the QDC to the “Procedures, Services, and Supplies” section of the Claim form. Follow these three steps for correct coding.
- Submit the quality data code as its own line item.
- Include a value of $0.01 under the “$ Charge” section.
- Use the right QDCs! Some of these may have changed for 2022 MIPS. Do not use old PQRS or old MIPS QDCs.
This sample CMS 1500 form shows how to correctly report the quality category for a patient seen for an office visit. The clinician is reporting on quality measure ID 117 (Diabetes: Eye Exam), using QDC 2022F.
What your Remittance Means
- N620 denial code: tells you that the QDC(s) are valid for the 2022 MIPS performance period, but it doesn’t mean the QDC(s) were reported correctly for the intended measure or that you met the measure requirements.
- CO 246 N620 code: If you bill a $0.00 QDC line item, you’ll get the N620 code. If you bill a $0.01 QDC line item, you’ll get the CO 246 N620 code. The CO 246 code indicates that it is a non-payable claim for required reporting only.
What to Do if your Claim is Denied
- If a claim is denied, the QDC is not accepted.
- When resubmitting a corrected claim, include the QDC.
- Once the claim has been paid, the QDC can't be changed or added if missing.
Note: Medicare does not provide quality reporting status reports during a performance year.
Scoring
Clinicians in small practices (≤ 15 clinicians) will receive 3 out of 10 points for each quality measure reported on at least 1 patient (up to 6 measures, maximum). To score more than 3 points for each quality measure, additional criteria must be met.
- Performance Period: Quality reporting must be done for a full calendar year within the 2022 performance year.
- Data Completeness: For each measure, the clinician must report on at least 70% of all Medicare Part B denominator-eligible patients seen during the performance year (this number is the data completeness numerator for the measure).
- For example, for the Diabetic Retinopathy measures, the denominator-eligible patients are all patients between the ages of 18 and 75 years with diabetes. The data completeness numerator is 70% of the denominator-eligible patients.
- Case Minimum: For any quality measure, at least 20 patients must be included in the denominator.
Performance Rate
Apart from the 3 base points for participation, CMS bases the additional 7 out of 10 points on your performance rate, which the agency calculates based on the following formula:
Performance Met
______________________________
Data Completeness Numerator - Denominator Exclusion - Denominator Exception
- CMS compares this performance-rate percentage to a benchmark. Each measure has an individual benchmark based on collective performance.
- Your points earned, out of 10, depends on the decile in which your performance rate falls. Note: Since clinicians in small practices receive a base score of 3 points per measure, the first three deciles are pooled into Decile 3.
- See the measure specification for performance required for each measure in order to earn more than 3 points.
| Decile Range |
Category Points
|
| Decile 3 |
3-3.9 |
| Decile 4 |
4-4.9 |
| Decile 5 |
5-5.9 |
| Decile 6 |
6-6.9 |
| Decile 7 |
7-7.9 |
| Decile 8 |
8-8.9 |
| Decile 9 |
9-9.9 |
| Decile 10 |
10 |
Claims Measures Available for Ophthalmologists
- Measure 1: Diabetes: Hemoglobin A1c Poor Control
- Measure 110 (NQF 0041): Preventive Care and Screening: Influenza Immunization
- Measure 111: Pneumonia Vaccination Status for Older Adults
- Measure 117: Diabetes: Eye Exam
- Measure 128: Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-up Plan
- Measure 130: Documentation of Current Medications in the Medical Record
- Measure 141: Primary Open-Angle Glaucoma (POAG): Reduction of Intraocular Pressure (IOP) by 15 Percent or Documentation of a Plan of Care
- Measure 226: Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- Measure 236 (NQF 0018): Controlling High Blood Pressure
- Measure 317: Preventive Care and Screening: Screening for High Blood Pressure and Follow-Up Documented
- Measure 397: Melanoma Reporting
Visit the QPP website to review measure specifications.
Review the CMS MIPS 2022 Part B Claims Reporting Quick Start Guide for more information.