My father, Claes Henrik Dohlman, is a Swedish-born ophthalmologist and a founder of the cornea subspecialty.
For more than 60 years he has been affiliated with the Department of Ophthalmology at Harvard Medical School, and for 15 of those years served as department chair and chief of ophthalmology at the Massachusetts Eye and Ear Infirmary. Prior to becoming chair, he established the world’s first cornea service, something that today is ubiquitous among U.S. eye departments. He is well known for his contributions to corneal biochemistry (1950s), surgical practice (1960s), teaching and administration (1970 and 1980s) and the development of a practical artificial cornea and its postoperative management (since the early 1990s) – with over 15,000 devices implanted worldwide.
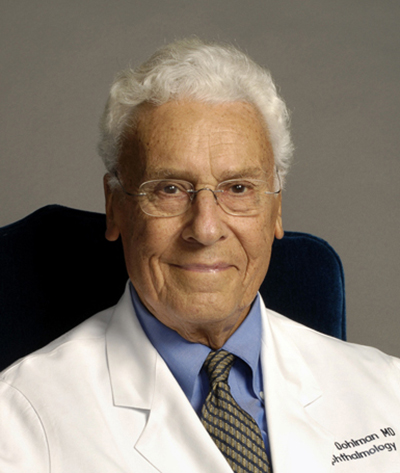
Claus H. Dohlman, MD, PhD
My father performed surgery well into his ninth decade, and at 97, he continues to train young scientists, develop new technologies and produce innovative treatments for the most hopeless cases of corneal impairment. Most recently, his efforts to prevent complications led to the identification of a novel mechanism of glaucoma. His innovations have restored vision to thousands, and revenues from these inventions have gone entirely to support new research and education.
My father is particularly proud of the individuals he has trained and mentored over the past six decades. These include more than 200 cornea fellows (clinical and research), nearly half of whom are now full professors. But how did he get his start? Who mentored the mentor? His path to a legendary career in ophthalmic science included work with some legendary academic researchers including Erik Jorpes, MD, Edward Maumenee, MD, Jonas Friedenwald, MD, Charles Schepens, MD, and Endre Balazs, MD, to name a few.
The following reminiscences come from occasional conversations with my father at home, and highlight three physician-scientists who had a unique impact on his professional growth and development.
First: Gösta Dohlman
My father’s father (“Farfar” in Swedish), Gösta Dohlman, was professor and chair of ENT at University of Lund. He had gained early recognition for his research discoveries working with Robert Bárány at Uppsala University in the 1920s.

In 1939, my father at 17, with my grandfather and his whippet “Jack”.
As my father describes, “we were most likely discussing one of many middling report cards from school!”
Bárány had previously received the Nobel Prize in 1914 for his work on the vestibular apparatus. My Farfar was his only doctoral student “Medicine Doktor”, working on fluid flow in the semicircular canals and its influence on the cupula. Although he published just four papers on the topic, the impact of his discoveries earned him a professorship at University of Lund. It was not without some setbacks along the way, however. As my father recalls, “When I was 3 or 4 years old, I wanted to pet the rabbits that he had been working on in the laboratory. He had operated on them for hours and experimented with them for months. I took it upon myself to open their cages so they could enjoy a bit of the outdoors, and they quickly hopped away into the countryside,” putting an end to the experiments.
My father enrolled in medical school in 1943, with his own father as one of the professors. While in medical school at Lund, he was drawn to biochemistry and was chosen to be a teaching assistant setting up experiments for the medical students and administering examinations.
“Back then it took seven or eight years to get an MD, and consisted of often needless accumulation of trivial knowledge. My career path was greatly influenced by my good friends since grade school Arvid Carlsson (who later won the Nobel Prize for the discovery of dopamine) and David Ingvar (who went on to become a prominent clinical neurophysiologist). Both were heading for medicine from the very start,” he recollected.
“After medical school, for my residency, my father suggested I should be an ENT surgeon (as he was), but it was the only time I dared to object. I had several friends in the ophthalmology department, and I found the eye to be a particularly interesting organ, with neurology in the back, transparent connective tissue in the front and the optics of the lens. I approached Professor Sven Larsson, who was very popular among the students. He agreed with some enthusiasm and I started in 1950.
“However, soon after I started Larsson had a heart attack, which according to my friends was so severe they had never seen anybody survive one like it. After that, he promised to be ‘the laziest professor in Sweden,” and he kept that promise! But that was fine with us because we took care of the work ourselves. At that time there were only four salaried positions in the department, and in our spare time we could do some research in the basement, on corneal edema, which eventually became one of my strongest lines of investigation.
“In 1952, I had eight months before my next appointment and thought I should break out and see something new. I asked Ernst Bárány (the ophthalmologist son of Róbert Bárány) who was brilliant, and worked on glaucoma, about what to do. In retrospect I should have applied to work with him, but I was fixated on the cornea because of some histochemical interest I had. I wanted to go the U.S. and asked Bárány ‘Who should I go to?’ He recommended Jonas Friedenwald at Johns Hopkins University in Baltimore. I wrote to him, and he agreed to take me on at a salary of $250 a month.
“Before traveling we had been instructed to go to the U.S. consulate in Gothenburg to get a student visa. The man at the desk looked at our application and said, ‘A student visa? Oh no Dr. Dohlman, take this. It is a green card, it is much better.’ This happened in 1952, and then again in 1958. In those days, there was a severe bias against the Eastern and Southern Europeans, so there were generous allotments to other countries including Sweden. The consulate had stacks of green cards with nobody to take them, so they were happy to give them to us.”
Second: Jonas Friedenwald
“We sailed (in 1952) on the Queen Mary from Southampton, England to New York City through a February storm. We lived in Baltimore for a year and a half in a bungalow, a shack really, up on Joppa Road.
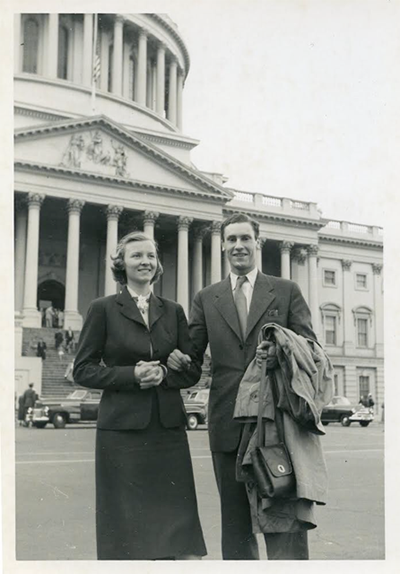
In 1952, my parents Carin and Claes touring the U.S. Capitol during a fellowship year at the Wilmer Institute at Johns Hopkins Hospital.
“Friedenwald suggested that I work out a histochemical method for organic sulfatases (which act on keratan sulfate, chondroitin sulfate, and other glycosaminoglycans) in the eye. He had done some experiments with lead precipitation, using heparin as a substrate that bound to proteoglycans. Proteoglycans were important in the cornea and also in the kidney. So I worked on that for a year but could not get any free sulfate to prove that the assay worked. I then realized this was a histochemical artifact and that I was staining lead phosphate and not lead sulfate. So, I was measuring the wrong enzyme! It took me a year to find this pitfall in histochemistry. I was a bit disappointed at the time, but it was very educational and set my own ambitions for the future.
“Friedenwald was an unusual man, a brilliant, but shy and introverted scholar. Despite his prominence, he was never promoted beyond associate professor and had a salary of only $4,000. He had a private practice with his father in the morning, research at the Wilmer Institute in the afternoons, and in the evenings he was home reading. His laboratory was miserable by modern standards, but he himself was quite an inspiration, and it was a very educational time for me. It was an entirely new world that opened up.
“After that, I went up to Boston for 8 months in 1953 and worked at the old Retina Foundation (now Schepens Eye Research Institute) with Endre Balazs (who later purified and commercialized the natural lubricant hyaluronic acid) on the biochemistry of the cornea, I learned a bit and had a good paper there. Charles Schepens encouraged me to balance patient care and research. Then I thought it was time to go home with (third child) Ebba coming and continue my career there in Sweden.”
Back home, my father continued his residency in ophthalmology, but had the opportunity to also continue his research on the metabolism of corneal proteoglycans. During that time, in 1956, he was drafted to serve as a medical officer to Oskar-Fredriksborg, a coastal artillery station outside of Stockholm, which he often described as “a dilapidated fortress, with a few rusty cannons, at the entrance of the Stockholm archipelago.” As my father tells it, the famous German Field Marshal Moltke is said to have smiled only twice in his life. First when his mother in-law died and again when he surveyed the Swedish defenses at Oskar-Fredriksborg!
Third: Erik Jorpes
“At Oskar-Fredriksborg there were two physicians on duty, with nothing to do, so we divided the days, 24 hours on and 24 hours off. I traveled into town on a boat and worked for 24 hours at a stretch in Erik Jorpes’ biochemistry department at the Karolinska Institute. After a long day in the lab I returned to the fort and slept on the job. This was the time when 35S radioisotopes had just arrived, and I realized what had previously taken years could now be done in minutes. One time in the laboratory I was centrifuging samples at 3 in the morning and got so sleepy I thought I should take a rest. There was only one sofa in the entire institution and that was in Jorpes’ inner sanctum, in his office. You can imagine what happened next. I woke up the next morning with Jorpes’ icy blue eyes staring down at me. But he thought in his skewed mind that this was a sign of devotion to science and came back to that incident repeatedly in promoting me.”
“Jorpes was a political radical, having grown up on the island of Åland, between Sweden and Finland in very poor circumstances, which marked him for life. He was a medical student in Helsinki in 1917, and when the Russian Revolution started, he became the leader (with Kuusinen) of the Finnish Communist party, rising up against the government. He was at the front of the barricades of Hälsingfors, fearless, in a very bloody and serious revolution. But the Germans were called in and crushed the rebellion, making short shrift of the communists.
“Jorpes fled to Russia and found himself sitting in a muddy border village waiting for his great return as president of Finland, which didn’t occur. With a death sentence on his head, he smuggled himself across the border and made it to Sweden. He went up to the faculty of the Karolinska Institute and announced his grand return. After some hesitation, he was allowed to start as a lab technician but quickly rose through the ranks to become Chair of department. He clarified the structure of heparin, worked on insulin, made a lot of money and became a capitalist (Jorpes studied the preparation of insulin at the Connaught Laboratories in Toronto, under the guidance of the Nobel-winning biochemists Frederick Banting and John Macleod. After returning, he launched the production of insulin by the Swedish pharmaceutical company Vitrum).
“The royalties made him wealthy, but rather than keep the money for himself, he supported his department. To think if they had caught him, he would have arrived in Sweden ‘a head shorter’. But he made it, and as far as I know he continued to have a death sentence on his head, which not many department chairs have (!).
“My interest in proteoglycans continued as a PhD student at Lund, working in Jorpes’ Biochemistry Department at Karolinska and later with Professors Lennart Rodén, Harry Boström, Sven Gardell and Torvard Laurent as preceptors. Rodén helped me the most in practical terms. He later moved to Alabama in the U.S.
“Laurent was a physical chemist of the highest caliber, and a friend from my time in Boston. Boström was a clinician interested in the metabolism of proteoglycans and later became Professor of Internal Medicine and Dean at University of Uppsala. Working in the evenings back in Lund, sometimes in Sune Bergström’s lab, I later found the sulfatases by using chemical isotopes instead of crude histochemical techniques. Bergström was mostly interested in prostaglandins, for which he later won the Nobel Prize, but I was not part of that team, and he showed no interest in me.”
After that, my father returned to doing translational research in Stockholm and finalizing his thesis, which was presented at University of Lund in 1958. That same year there was a career-changing opportunity; he was recruited back to Boston at the invitation of Balazs, Schepens and Edwin Dunphy, then chief of ophthalmology at Mass Eye and Ear. This move would prove permanent. He took a faculty position at Harvard Medical School, first as an instructor (1961), then assistant professor (1968), associate professor (1969), professor (1973), chair (1974-1989) and professor emeritus (1993).
For 16 years my parents lived in suburban Arlington, first with three children. Soon after, there were six. Those were magical years living on Pleasant Street in a converted carriage house by Spy Pond, and they were followed by 45 years in Weston. Most summers we had family reunions at our ancestral family home at a small farm in Sweden. In 2019, the family gathered there to honor Mamma Carin, who died at age 91 from complications of Parkinson’s disease.
What did my father learn from his three most influential mentors? As he puts it, “They advised me to focus, focus and focus, respectively — although I didn’t always follow their advice.” Nevertheless, my father’s career accelerated after 1958, and there have been many laurels along the way, including the Friedenwald Award (1971), Castroviejo Medal (1981), ASCRS Ophthalmology Hall of Fame (2004), Laureate Award of the American Academy of Ophthalmology (2007), Helen Keller Award (2010) and the Gullstrand Medal (2012) which is given once per decade by the Swedish Medical Society.
At the age of 96, he was conferred an honorary doctorate and delivered the commencement address at the University of Montreal. He could well hold the record as the oldest graduation speaker in history! He has continued to champion academic medicine and has authored almost 400 articles, including more than 60 after turning 90.

In 2002, celebrating my father’s 80th birthday, at our family’s summer home in Sweden.
Most important is his legacy of mentorship. It is important to remember that the many residents and fellows who trained with my father are also part of an eclectic scientific family tree, one that includes the senior Professor Dohlman, Friedenwald, Jorpes and many others who have helped to shape the discipline of ophthalmology.
Editor’s Note: Henrik Dohlman, PhD, is Claes H. Dohlman’s fourth child and is the Sanford Steelman Distinguished Professor and chair of pharmacology at the University of North Carolina. We are grateful to him and to our History of Ophthalmology editor, Daniel M. Albert, MD, MS, and his editorial assistant, Ms. Jane Shull, for contributing this article to Scope.