Editor’s note: I asked an old friend and colleague, Steven Newman, MD to put our present COVID-19 pandemic into context. Dr. Newman, a neuro-ophthalmologist, is an extraordinary erudite man who puts most things into historical context. I knew of his passion and ability to teach. His manuscript was comprehensive and filled with tantalizing facts. This, then, is the first of a four-part series that looks at COVID-19 within the context of other pandemics. These are the topics:
Part 1. Etiology of Pandemics
A pandemic is an epidemic of an infectious disease that has spread across a large region affecting a substantial number of people. Although our current problems are with COVID-19, there have been other viruses and bacteria such as tuberculosis and the Yersinia Plague (Black Death) which have also caused global pandemics. Although some of the earliest cases of COVID-19 had ophthalmic (conjunctivitis) and neuro-ophthalmic manifestations, in other pandemics ophthalmic findings have been less common.
The earliest recorded pandemics go back to ancient Greece, but the earliest record of an infectious disease (which had ophthalmic findings) was found in Australia and was probably trachoma. Egyptian mummies showed evidence of trachoma infection one to two centuries before the common era. These epidemics not only reduced the population but had major economic, cultural, and military consequences. Probably the earliest well recorded pandemic was in 6th century B.C. involved the Peloponnesian wars (between two Greek factions lead by Athens and Sparta). During the fighting most deaths (more than one-fourth of Athens’ population) were due to an epidemic, leading to the subjugation of Athens and, a couple of centuries later, the rise of Rome. More recent studies have suggested this was typhus based on the examination of corpses.
We can look at pandemics in four ways: 1) etiology 2) chronologically 3) death rate (which may be total number of deaths or a percentage of the population) or 4) The extent of disruption caused by the pandemic (either monetarily or with social disruption). This section is organized by etiology which was largely not understood at that time.
Documented outbreaks of previous pandemics go back to the plague of Athens, 430 to 426 B.C., during the Peloponnesian war which killed a quarter of the Athenian troops and a quarter of the population. It was so effective at killing people that it probably reduced its spread. Researchers at the University of Athens in 2006 analyzed teeth recovered from a mass grave and confirmed the presence of bacterium responsible for typhus. The plague of Athens included redness and inflammation of the eyes with possible blindness as can happen with epidemic typhus.
The Antonine plague between 165 and 180 A.D., could have been measles or smallpox (or even bubonic plague). It probably killed a quarter of those infected, or about 5 million people. The Antonine plague arrived in Rome from the east and ultimately involved approximately 15% of the entire empire. Galen described this as a black exanthem with fever and slight cough which may well have been early occurrence of smallpox. A second occurrence of this type of epidemic was the plague of Cyprian (also known as the plague of Commodus) in 251 to 266 A.D.
Bubonic Plague

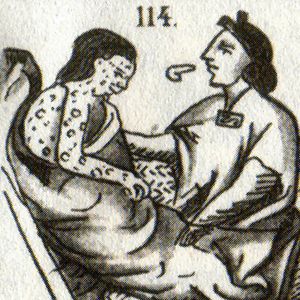
A medieval drawing of bubonic depicts plague victims with buboes.
Between 541 and 750 A.D., there was the earliest recorded outbreak of bubonic plague which started in Egypt and reached Constantinople, killing 10,000 people a day at its height and ultimately killing about 40% of the inhabitants of Constantinople. This was a foreshadowing of the great pandemic of Black Death (another name for bubonic plague) to come. This was later recognized to be due to the bacterium Pasteurella pestis.
The Black Death killed an estimated 75 million to 200 million people in the 14th-century and may have caused the most fatalities of any pandemic and certainly involved the highest percentage of the population . It is hard to deny that this pandemic had the greatest repercussions on civilization, religion, politics, and social organization. It may have been spread to Europe by one of the earliest uses of biological warfare during the siege of Kaffa (in the Crimea). Mongols catapulted corpses of Mongol warriors who had died of the plague into the city. From there it spread to nearby Constantinople and by ships to Genoa and Venice (via Messina), Italy in 1347.
Over the next few years, the Black Death killed an estimated 20% to 30% of Europe’s population. This disease would recur in England every two to five years from 1361 to 1480. The Black Death could have three forms, bubonic, pneumonic, systemic. Ocular manifestations were not common, but could include bilateral panophthalmitis, as well as infiltration of the choroid and retina with neutrophils, necrotizing vasculitis, and retinal detachment.
The last time this was a major epidemic was in England between 1665-1666 which killed approximately 100,000 or about 20% of London’s population. Between 1720 and 1723 the French port city of Marseille also suffered several rounds from bubonic plague. Daviel volunteered as a physician there before his development of cataract extraction and was thus honored by the king. A third incidence of Bubonic Plague occurred in 1855, starting in China and spreading to India where 10 million people died. It also involved the Western part of the United States.
Cholera
Cholera is spread by fecal contamination as recognized by Dr. John Snow, an OB/GYN who noted the victims all worked or lived near the Broad Street Pump. This observation led to an intervention. The handle was removed from the pump and an upgrading of the sewer system was instituted leading to a dramatic reduction in contamination. But more recently, viruses have been the major cause of pandemics.
A third etiology are obligate organisms that are phylogenetically somewhere in between bacteria and viruses. These include rickettsia, including that responsible for typhus (“camp fever”). Although other rickettsial diseases may cause epidemics, they usually do not spread widely enough to be responsible for pandemics.
The World Health Organization (WHO) has a six-stage classification system describing how the disease begins, usually when animals are infected with a virus, and followed sometimes when animals with a virus infect people with a mutation:
Phase 1) animal to animal
Phase 2) animal to human
Phase 3) sporadic and cluster cases in human
Phase 4) sustained community level outbreaks
Phase 5) sustained in two countries
Phase 6) sustained in country and other WHO regions
Although parasites can cause epidemics they do not spread widely enough to be recognized as a cause of pandemics. These include malaria, which was particularly a problem during the American Civil War.
Viral epidemics are probably the leading cause of systemic human infection worldwide as recognized at the Rockefeller Institute. Viruses are compact vessels containing coded instructions in the form of either DNA or RNA. This distinction is important since while DNA based viruses may repair defects in their DNA, this is not possible in RNA based viruses. Hence, there is a much higher rate of mutation and potential clinical change seen in RNA viruses. RNA viruses include flaviviruses (yellow fever, dengue, Zika, West Nile) but while extremely infectious with a high mortality, they are usually too localized to be produce a pandemic.
Yellow Fever
Even before the better-known experimental work by Dr. Walter Reed, Army Institute of Research, Dr. Carlos Finley, a Cuban epidemiologist (who trained in France and Jefferson Medical College in Philadelphia), first theorized that mosquitos were the vector in yellow fever.
Yellow fever is still endemic in sub-Sahara Africa and tropical South America. This may produce choroidal thickening, vitreous cells, and yellowish sub-retinal lesions. Although perhaps not extensive enough to be called a pandemic it was one of the major reasons for the failure of the French to build the Panama Canal. William Gorgas had been sent to Cuba to study yellow fever and then was sent to Panama when the U.S. took over the building of the Canal. He was largely responsible for aggressive efforts to control mosquitos.
Yellow fever epidemics involved the Mississippi River Valley (in 1878, leading to a statement to Congress that yellow fever should be dealt with as an enemy which imperils life and cripple’s commerce and industry) and also Philadelphia. Yellow fever caused several devastating epidemics particularly involving the U.S., occurring in New York, Philadelphia, and Boston, with an episode in 1793, killing as many as 5,000 people in Philadelphia which was roughly 10% of the population at that time. Yellow fever was also present during the Spanish American War.
Measles
A measles-like syndrome was initially described in Persia 854 to 925. Major outbreaks of measles-like syndrome occurred in the Pacific in 1875, killing one-third of the population. The incubation period was 10-12 days followed by cough, conjunctivitis, coryza, and fever. The most common ophthalmic complications included keratitis, non-purulent conjunctivitis, and rarely attenuated arterioles, retinal edema, neuroretinitis and retinal hemorrhages. This may result in pigmentary retinopathy with bone spicule or salt and pepper configuration usually when acquired in utero.
A late subsequent development related to measles can be sub-acute sclerosing panencephalitis, which produces focal and necrotizing retinitis and choroiditis, retinal folds, hemorrhage, serous detachments, and occlusive central nervous system vasculitis. The World’s worst known epidemic of measles occurred in January 2020 in the Democratic Republic of the Congo but did not spread sufficiently to rate as a pandemic.
HIV
Other previous epidemics include human immunodeficiency virus (HIV), which is no longer uncontrolled, outside of Africa. HIV probably originated in monkeys in Africa around 1920 (although not causing human disease until the 1950’s). It was likely spread to the United States via Haiti. It is still a pandemic in Africa, with infection rates as high as 25% in some regions. Proactive education about safer sexual practices and blood born infection have markedly flattened the curve. Impairment of the immune system causes a tremendous susceptibility to secondary infections including pneumocystis and also neoplastic diseases including Kaposi’s sarcoma.
Overall, HIV may have infected 75 million people and caused 32 million deaths. With the advent of HARRT (Highly active antiretroviral therapy), fatalities have become much less common. HIV causes ophthalmic microvasculopathy and frequently secondary bacterial and viral infectious disease. HIV patients also may have a high incidence of side effects of medications such as Ethambutol and Cidofovir.
Zika
Zika virus has been endemic in Africa and Asia for more than 60 years, probably transmitted by mosquitos producing a macular-papular rash, arthralgias, but also ophthalmic manifestations of uveitis, acute maculopathy, and non-purulent conjunctivitis. Other findings include macular scaring, focal pigmentation, iris coloboma, lens subluxation, cataracts, glaucoma, and micro-ophthalmia. Ocular coherence tomography (OCT) of infants may demonstrate outer retina pathology and hyperreflectility of the retinal pigment epithelium. Although this may produce significant morbidity there is no evidence that it has risen to the level of pandemic. Zika vaccines are the subject of investigation. Other findings include macula scaring, focal pigmentation, iris coloboma, lens subluxation, cataracts, glaucoma, and micro-ophthalmia. OCT taken in infants may demonstrate outer retina pathology and hyperreflectility of the retinal pigment epithelium.
16th-century Aztec drawing of smallpox victims
Smallpox
Smallpox (a DNA virus) was largely responsible for eliminating 80-90% of the indigenous populations of the Americas. Smallpox epidemics in the 16th century probably killed 56 million people in the Americas. It devastated the Australian aboriginal population, killing up to 50% of those infected. It also killed many of the native New Zealand Maori. Interestingly, it had been recognized in the middle of the second millennium in Africa and the Middle East (possibly first recognized in China around the year 1000) that patients that had previous episode of smallpox could not be re-infected. The mechanism behind this protection from previous infection was not understood but the concept probably was key to H.G. Wells’ “War of the Worlds”.
Smallpox produced multiple pandemics throughout the world. It was during one epidemic in Boston (1721) that a therapeutic approach was investigated. Smallpox has always been a recurring epidemic, both in Africa and the Middle East. Protection from previous infection was understood in China, Africa and the Middle East. This was introduced to the colonies during the smallpox epidemic in Boston in 1721 when Cotton Mather, who played a role in the Salem witch trials, emphasized the use of variolization where smallpox scabs were applied to healthy individuals with the idea that if they got a mild-form of the infection then they would then be protected in the future, although there was really no understanding of the pathophysiology. He may have been influenced by the wife of the British ambassador to the Ottoman Empire (Lady Mary Wortley Montagu) where variolization was routinely practiced. Abigail Adams, (married to our second president, John Adams), probably saved hers and many other children in the Boston area by promoting this variolization process.
By the end of the 18th century (1796), Jenner noticed that milkmaids that developed cowpox were also protected from infection from smallpox. This was the beginning of vaccination to decrease the chance of a more severe episode of smallpox associated with variolization. George Washington supported vaccination for his troops and Thomas Jefferson as president (and having consulted with Abigail Adams for this) also strongly supported vaccination. Dr. Jean de Carro helped introduce vaccination to India and worked to discourage variolization. Vaccination for smallpox became mandatory in England in 1853. This did not save some Confederate soldiers who died of smallpox following the Battle of Antietam (U.S. Civil War).
Interestingly there is evidence that smallpox may have affected Egyptian mummies from the 18th Egyptian Dynasty (1570 to 1850 B.C.), although the first clinical report was from 1350 B.C. during the Egyptian-Hittite War. There were ophthalmic complications, potentially producing blindness. Initial symptoms after an incubation period of two weeks included fever, malaise, and headache with progressive exanthem, first flat macular lesions then raised pustules vesicles with a mortality rate of about 30%.
About 2% to 3% of the infections would develop the hemorrhage form, which was nearly always fatal. About 5% to 9% of patients with smallpox developed ocular complications including involvement of the eyelids and possible corneal involvement. This could lead to corneal ulceration, hypopyon, iris prolapse, perforation, and endophthalmitis. Patients that survived could have disciform keratitis, iritis, iridocyclitis, and possible proptosis.
Ebola
By 1911, Peyton Rous realized that viruses could also cause cancer, for which he would eventually win the Nobel Prize in 1966. More recently, potential epidemics include other extremely virulent viral diseases such as Ebola, Lassa fever, Rift Valley fever and Marburg virus. These have not extended as widely as some of the other diseases we have previously discussed thus not technically pandemic. Dengue fever was also caused by an RNA virus.
Ebola is a viral hemorrhagic fever first identified in 1976 with an epidemic in West Africa in 2013 and 2016 with an average fatality rate of greater than 50%. These patients tend to develop conjunctival injection, sub conjunctival hemorrhage, and vision loss of unknown etiology. Those that survive may develop post Ebola virus syndrome. Ocular complications include posterior, anterior and panuveitis as well as optic neuropathy and motility disturbance. Because this disease is so efficient in killing off its host, it does not seem to be capable of producing a pandemic.