Introduction
These are summary benchmarks for the Academy's Preferred Practice Pattern® (PPP) guidelines. The Preferred Practice Patterns series of guidelines has been written on the basis of three principles.
- Each Preferred Practice Pattern should be clinically relevant and specific enough to provide useful information to practitioners.
- Each recommendation that is made should be given an explicit rating that shows its importance to the care process.
- Each recommendation should also be given an explicit rating that shows the strength of evidence that supports the recommendation and reflects the best evidence available.
Preferred Practice Patterns provide guidance for the pattern of practice, not for the care of a particular individual. While they should generally meet the needs of most patients, they cannot possibly best meet the needs of all patients. Adherence to these Preferred Practice Patterns will not ensure a successful outcome in every situation. These practice patterns should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. It may be necessary to approach different patients' needs in different ways. They physician must make the ultimate judgment about the propriety of the care of a particular patient in light of all of the circumstances presented by that patient. The American Academy of Ophthalmology is available to assist members in resolving ethical dilemmas that arise in the course of ophthalmic practice.
The Preferred Practice Pattern® guidelines are not medical standards to be adhered to in all individual situations. The Academy specifically disclaims any and all liability for injury or other damages of any kind, from negligence or otherwise, for any and all claims that may arise out of the use of any recommendations or other information contained herein.
For each major disease condition, recommendations for the process of care, including the history, physical exam and ancillary tests, are summarized, along with major recommendations for the care management, follow-up, and education of the patient. For each PPP, a detailed literature search of PubMed and the Cochrane Library for articles in the English language is conducted. The results are reviewed by an expert panel and used to prepare the recommendations, which are then given a rating that shows the strength of evidence when sufficient evidence exists.
To rate individual studies, a scale based on the Scottish Intercollegiate Guideline Network (SIGN) is used. The definition and levels of evidence to rate individual studies are as follows:
- I++: High quality meta-analyses, systematic reviews of randomized controlled trials (RCTs), or RCTs with a very low risk of bias
- I+: Well-conducted meta-analyses, systematic reviews of RCTs, or RCTs with a low risk of bias
- I-: Meta-analyses, systematic reviews of RCTs, or RCTs with a high risk of bias
- II++: High-quality systematic reviews of case-control or cohort studies; high-quality case-control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal
- II+: Well-conducted case-control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal
- II-: Case-control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal
- III: Nonanalytic studies (e.g., case reports, case series)
Recommendations for care are formed based on the body of the evidence. The body of evidence quality ratings are defined by Grading of Recommendations Assessment, Development and Evaluation (GRADE) as follows:
- Good quality (GQ): Further research is very unlikely to change our confidence in the estimate of effect
- Moderate quality (MQ): Further research is likely to have an important impact on our confidence in the estimage of effect and may change the estimate
- Insufficient quality (IQ): Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; any estimate of effect is very uncertain
Key recommendations for care are defined by GRADE as follows:
- Strong recommendation (SR): Used when the desirable effects of an intervention clearly outweigh the undesirable effects or clearly do not
- Discretionary recommendation (DR): Used when the trade-offs are less certain -- either because of low-quality evidence or because evidence suggests that desirable and undesirable effects are closely balanced
The PPPs are intended to serve as guides in patient care, with greatest emphasis on technical aspects. In applying this knowledge, it is essential to recognize that true medical excellence is achieved only when skills are applied in such a manner that the patients' needs are the foremost consideration. The AAO is available to assist members in resolving ethical dilemmas that arise in the course of practice. (AAO Code of Ethics)
Age-Related Macular Degeneration (Initial and Follow-up Evaluation)
Initial Exam History (Key elements)
- Symptoms (metamorphopsia, decreased vision, scotoma, photopsia, difficulties in dark adaptation)
- Medications and nutritional supplement use
- Ocular history
- Medical history (any hypersensitivity reactions)
- Family history, especially family history of AMD
- Social history, especially smoking
Initial Physical Exam (Key elements)
- Comprehensive eye examination
- Amsler grid
- Stereo biomicroscopic examination of the macula
Diagnostic Tests
Optical coherence tomography is important in diagnosing and managing AMD, particularly with respect to determining the presence of subretinal and intraretinal fluid and in documenting the degree of retinal thickening. Optical coherence tomography defines the cross sectional architecture of the retina, which is not possible with any other imaging technology. It may reveal the presence of fluid that is not apparent on biomicroscopy alone. It also assists in evaluating the response of the retina and RPE to therapy by allowing structural changes to be followed accurately. Newer generation OCT modalities, including SD-OCT, are preferred technologies.
Optical coherence tomography angiography (OCTA) is a newer imaging modality that provides noninvasive evaluation of the retinal and choroidal vasculature and is being more commonly applied in the evaluation and management of AMD, but it has not replaced other angiographic methods.
Intravenous fundus fluorescein angiography of AMD is indicated:
- when patient complains of new metamorphopsia
- when patient has unexplained blurred vision
- when clinical exam reveals elevation of the RPE or retina, macular edema, subretinal blood, hard exudates or subretinal fibrosis or the OCT shows evidence of fluid
- to detect the presence of and determine the extent, type, size, and location of CNV
- to guide treatment (laser photocoagulation surgery or verteporfin PDT)
- to detect persistent or recurrent CNV or other retinal diseases following treatment
- to assist in determining the cause of visual loss that is not explained by clinical exam
Each angiographic facility should have a care plan for an emergency and a clear protocol to minimize the risks and to manage any complications.
Follow-up Exam History
- Visual symptoms, including decreased vision and metamorphopsia
- Changes in medications and nutritional supplements
- Interval ocular history and medical history
- Changes in social history, especially smoking
Follow-up Physical Exam
- Visual acuity at distance with correction
- Amsler grid
- Stereo biomicroscopic examination of the fundus
Follow-up after Treatment for Neovascular AMD
- Examine patients treated with intravitreal ijections of aflibercept, bevacizumab, or ranibizumab approximately at 4-week intervals
- Subsequent examinations, OCT, and fluorescein angiography should be performed as indicated depending on the clinical findings and the judgment of the treating ophthalmologist
Patient Education
- Educate patients about the prognosis and potential value of treatment as appropriate for their visual and functional status
- Encourage patients with early AMD or a family history of AMD to assess their own visual acuity using monocular vision testing and to have regular dilated eye exams for early detection of intermediate AMD
- Educate patients with a high-risk AMD phenotype about methods of detecting new symptoms of CNV and about the need for prompt notification to an ophthalmologist (III, GQ, SR)
- Instruct patients with unilateral disease to monitor their vision in their fellow eye and to return periodically even in absence of symptoms, but promptly after onset of new or significant visual symptoms
- Instruct patients to report symptoms suggestive of endophthalmitis, including eye pain or increased discomfort, worsening eye redness, blurred or decreased vision, increased sensitivity to light, or increased number of floaters promptly
- Encourage patients who are currently smoking to stop because there are observational data that support a causal relationship between smoking and AMD and other considerable health benefits of smoking cessation
- Refer patients with reduced visual function for vision rehabilitation (see www.aao.org/low-vision-and-vision-rehab) and social services
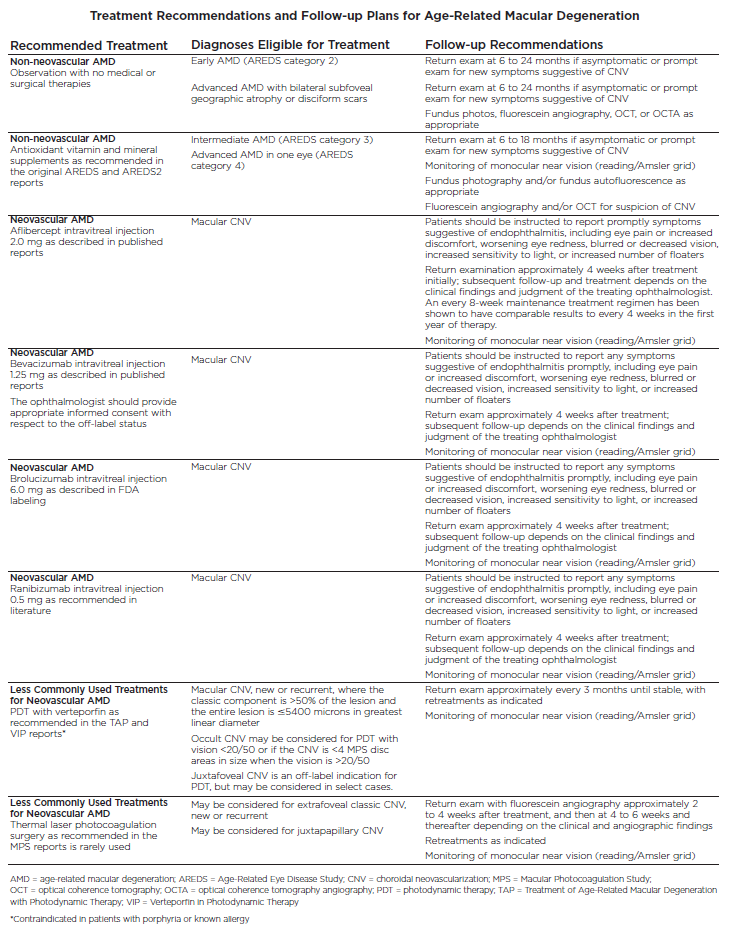
Age-Related Macular Degeneration (Management Recommedations)
Treatment Recommendations and Follow-up Plans for Age-Related Macular Degeneration
Diabetic Retinopathy (Initial and Follow-up Evaluation)
Initial Exam History (Key elements)
-
Duration of diabetes
-
Past glycemic control (hemoglobin A1c)
-
Medications
-
Medical history (e.g., obesity, renal disease, systemic hypertension, serum lipid levels, pregnancy)
-
Ocular history
Initial Physical Exam (Key elements)
-
Visual acuity
-
Slit-lamp biomicroscopy
-
Measurement of IOP
-
Gonioscopy before dilation when indicated (for neovascularization of the iris or increased IOP)
-
Pupillary assessment for optic nerve dysfunction
-
Thorough funduscopy including stereoscopic examination of the posterior pole
-
Examination of the peripheral retina and vitreous, best performed with indirect ophthalmoscopy or with slit-lamp biomicroscopy
Diagnosis
-
Classify both eyes as to category and severity of diabetic retinopathy and macular edema. (III, GQ, SR) Each category has an inherent risk for progression and is dependent on adherence to overall diabetes control.
Follow-up History
-
Visual symptoms
-
Systemic status (pregnancy, blood pressure, serum lipids, renal status)
-
Glycemic status (hemoglobin A1c)
- Other treatments (dialysis, fenofibrates)
Follow-up Physical Exam
-
Visual acuity
-
Slit-lamp biomicroscopy with iris examination
- Measurement of IOP
-
Gonioscopy (preferably before dilation when iris neovascularization is suspected or if IOP is elevated)
-
Stereoscopic examination of the posterior pole after dilation of the pupils
-
Examination of the peripheral retina and vitreous when indicated
-
OCT imaging when appropriate
Ancillary Tests
- Color fundus photography may be useful for documenting the severity of the diabetes presence of NVE and NVD, the response to treatment, and the need for additional treatment at future visits
-
Optical coherence tomography can be used to quantify retinal thickness, monitor macular edema, identify vitreomacular traction, and detect other forms of macular disease in patients with diabetic macular edema. Decisions to treat with anti-VEGF injections, change therapeutic agents (e.g., use of intraocular corticosteroids), initiate laser treatment, or even consider vitrectomy surgery are often based in part on OCT findings.
-
Fluorescein angiography is not routinely indicated as a part of the examination of patients with diabetes. Fluorescein angiography is used as a guide for laser treatment of CSME and as a means of evaluating the cause(s) of unexplained decreased visual acuity. Angiography can identify macular capillary nonperfusion as possible explanations for visual loss that is unresponsive to therapy.
- Optical coherence tomography angiography offers a noninvasive nature and the ability to visualize depth-resolved, capillary-level abnormalities in the three retinal plexuses, offering a much more quantitative assessment of macular ischemia. Although the technology is FDA approved, the guidelines and indications for use in diabetic retinopathy are evolving.
-
Ultrasonography enables assessment of the status of the retina in the presence of a vitreous hemorrhage or other media opacity, and may be helpful to define the amount of vitreous hemorrhage, the extent and severity of vitreoretinal traction, and diagnose diabetic retinal detachments in the setting of media opacity
Patient Education
-
Discuss results of exam and implications
-
Encourage patients with diabetes but without diabetic retinopathy to have annual dilated eye exams
-
Inform patients that effective treatment for diabetic retinopathy depends on timely intervention, despite good vision and no ocular symptoms, and that current treatments often require multiple visits and evaluations over time for adequate delivery of therapeutic effect
-
Educate patients about the importance of maintaining near-normal glucose levels and nearnormal blood pressure and lowering serum lipid levels
-
Communicate with the attending physician, e.g., family physician, internist, or endocrinologist, regarding eye examination findings
-
Provide patients whose conditions fail to respond to surgery and for whom further treatment is unavailable with professional support and offer referral for counseling, rehabilitative, or social services as appropriate
-
Refer patients with functionally limiting postoperative visual impairment for vision rehabilitation (see www.aao.org/low-vision-and-vision-rehab) and social services
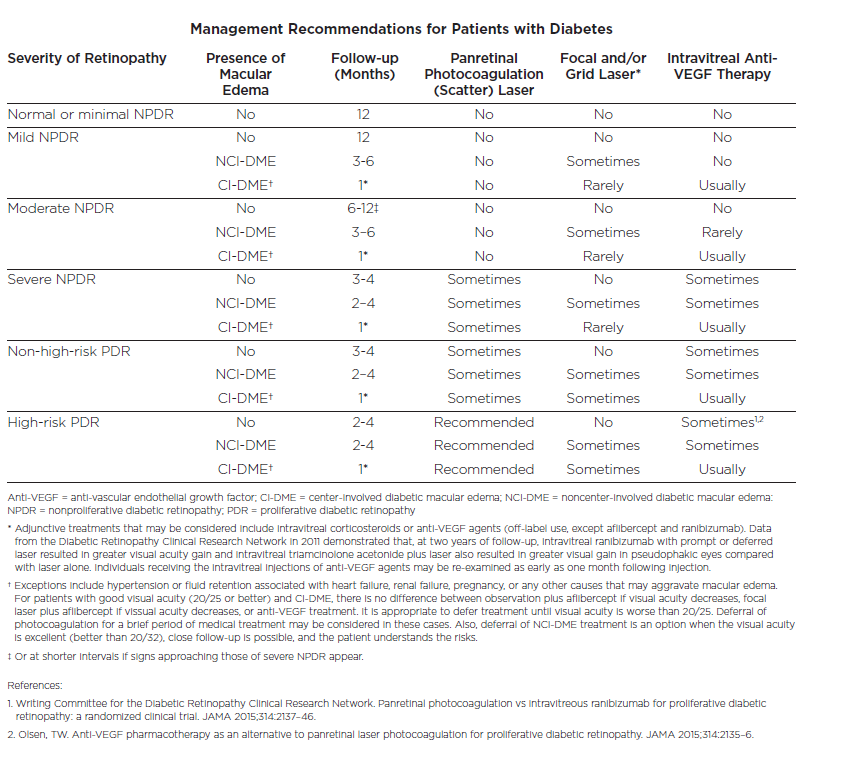
Diabetic Retinopathy (Management Recommendations)
Management Recommendations for Patients with Diabetes
Idiopathic Epiretinal Membrane and Vitreomacular Traction (Initial Evaluation and Therapy)
Initial Exam (Key elements)
-
Ocular history (e.g., posterior vitreous detachment, uveitis, retinal breaks, retinal vein occlusions, proliferative diabetic retinopathy, ocular inflammatory diseases, recent wound healing)
-
Duration of symptoms (e.g., metamorphopsia, difficulty using both eyes together, and diplopia)
-
Race/ethnicity
-
Systemic history
Physical Exam (Key elements)
-
Slit-lamp biomicroscopy the macula, vitreoretinal interface, and optic disc
-
An indirect peripheral retinal examination
-
Amsler grid test and/or Watzke-Allen test
-
OCT to diagnose and characterize VMA, ERM, VMT, and associated retinal changes
-
Fluorescein angiogram or OCTA may be helpful to evaluate ERMs and/or VMT
Management Plan
-
The decision to intervene surgically in patients with ERM/VMT usually depends upon the severity of symptoms, especially the impact on daily activities
-
Patients should be informed that the majority of ERMs will remain stable and do not require therapy
-
Patients should be reassured that there is a very successful surgical procedure that could address worsening symptoms or decreasing visual acuity
-
Risks versus benefits of vitrectomy surgery should be discussed. Risks include visual acuity, cataract, retinal tears, retinal detachment, and endophthalmitis
Surgery and Postoperative Care
-
Vitrectomy surgery is often indicated in patients who are affected with a decrease in visual acuity, metamorphopsia, and double vision or difficulty using their eyes together
-
Patients should be examined postoperatively day 1, and again 1 to 2 weeks following surgery, or sooner depending upon the development of new symptoms or new findings during early postoperative examination
Follow-up Physical Exam:
- Internal history
- Measurement of IOP
- Slit-lamp biomicroscopy of anterior segment
- Indirect binocular ophthalmoscopy of peripheral retina
- Counseling on use of post-op medications
- Counseling on signs and symptoms of retinal detachment
- Precautions on intraocular gas if used
Patient Education and Follow-up
-
Comparing OCT images in the abnormal versus normal eye can aid patient understanding
-
Patients should be encouraged to periodically test their central vision monocularly to detect changes that may occur over time, like increasing metamorphopsia small central scotoma
-
Patients should be informed to notify their ophthalmologist promptly if they have symptoms such as an increase of floaters, loss of visual field, metamorphopsia, or a decrease in visual acuity
- Patients with functionally limiting postoperative visual impairment should be referred for vision rehabilitation (see www.aao.org/low-vision-and-vision-rehab) and social services
Idiopathic Macular Hole (Initial Evaluation and Therapy)
Initial Exam History (Key elements)
-
Duration of symptoms
-
Ocular history: glaucoma, retinal detachment or tear, other eye diseases, eye or head injuries, ocular surgery, or sun or eclipse gazing or use of a laser pointer or other laser
-
Medications that may be related to macular cystoid edema (e.g., systemic niacin, topical prostaglandin analogues, tamoxifen)
Initial Physical Exam (Key elements)
-
Slit-lamp biomicroscopic examination of the macula and the vitreoretinal interface
- Indirect peripheral retinal examination
- Amsler grid test and/or Watzke-Allen test
Ancillary Test
- OCT offers detailed information about the macular anatomy size if an FTMH is present, and presence of any VMT or epiretinal membrane
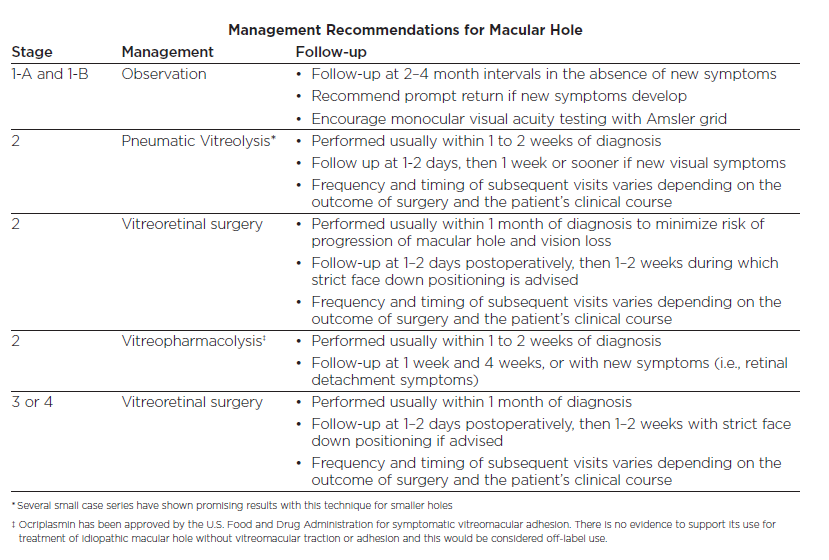
Management Recommendations for Macular Hole
Surgical and Postoperative Care if Patient Receives Treatment
-
Patients should be informed about relative risks, benefits, and alternatives to surgery, and the need for use of expansile intraocular gas or facedown positioning postoperatively
-
Formulate a postoperative care plan and inform the patient of these arrangements
-
Patients should be informed of possible postoperative increase in IOP
-
Examine postoperatively within 1 or 2 days and again 1 to 2 weeks after surgery
- Components of follow-up visit should include interval history, visual acuity measurement, measurement of IOP, slit-lamp biomicroscopy, and OCT evaluation to document post-op macular anatomy when indicated of the anterior chamber and central retina, and indirect ophthalmoscopy of the peripheral retina
Patient Education
-
Patients should be informed to notify their ophthalmologist promptly if they have symptoms such as an increase in floaters, a loss of visual field, metamorphopsia, or a decrease in visual acuity
-
Patients should be informed that air travel, travel to higher or lower altitudes, or general anesthesia with nitrous oxide should be avoided until the gas tamponade is nearly completely gone
-
Patients who have had a macular hole in one eye should be informed that they have a 10% to 15% chance of macular hole formation in the fellow eye, especially if the vitreous remains attached
-
Patients with functionally limiting postoperative visual impairment should be referred for vision rehabilitation (see www.aao.org/low-vision-and-vision-rehab) and social services
Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration (Initial and Follow-up Evaluation)
Initial Exam History (Key elements)
-
Symptoms of PVD
-
Family history of RD, related genetic disorders (e.g., Stickler syndrome)
-
Prior eye trauma
-
Myopia
-
History of ocular surgery including refractive lens exchange and cataract surgery
- History of YAG laser capsulotomy
- History of intravitreal injection
Ophthalmic Exam (Key elements)
-
Confrontation visual field examination
- Visual acuity testing
- Pupillary assessment for the presence of a relative afferent pupillary defect
-
Examination of the vitreous for hemorrhage, detachment, and pigmented cells
-
Examination of the peripheral fundus using scleral depression. The preferred method of evaluating peripheral vitreoretinal pathology is with indirect ophthalmoscopy combined with scleral depression.
Diagnostic Tests
-
Optical coherence tomography may be helpful to evaluate and stage the PVD
-
Perform B-scan ultrasonography if peripheral retina cannot be evaluated
-
If no abnormalities are found, frequent follow-up examinations are recommended (i.e., every 1-2 weeks initially)
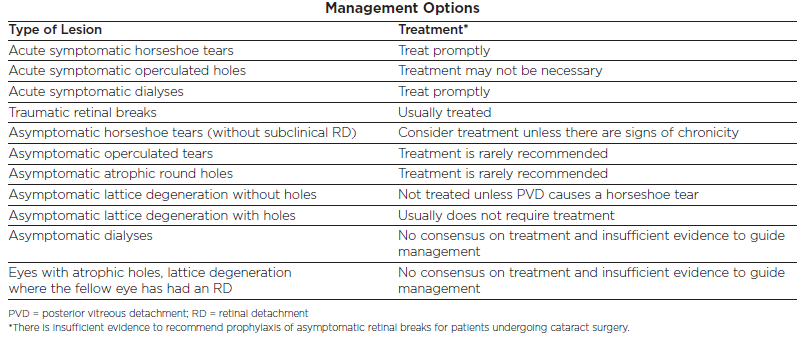
Management:
-
Patients should be informed about the relative risks, benefits, and alternatives to surgery
-
Formulate a postoperative care plan and inform patient of these arrangements
-
Patients should be advised to contact ophthalmologist promptly if they have a substantial change in symptoms such as floaters, peripheral visual field loss, or decreased visual acuity
Follow-up History
-
Visual symptoms
-
Interval history of eye trauma, intraocular injection, or intraocular surgery
Follow-up Physical Exam
-
Visual acuity
-
Evaluation of the status of the vitreous, with attention to the presence of pigment, hemorrhage, or syneresis
-
Examination of the peripheral fundus with scleral depression or a fundus contact or non-contact lens using the slit-lamp biomicroscope
-
Wide-field photography may help but does not replace careful ophthalmoscopy
-
Optical coherence tomography if vitreomacular traction is present
-
B-scan ultrasonography if the media are opaque
Patient Education
-
Patients at high risk of developing retinal detachment should be educated about the symptoms of PVD and retinal detachment and the value of periodic follow-up exams
-
Patients who undergo refractive surgery should be informed they remain at risk of RRD despite reduction of their refractive error
Retinal and Ophthalmic Artery Occlusions (Initial Evaluation and Therapy)
Initial Exam (Key elements)
-
Duration of vision loss
-
Symptoms of GCA (e.g., vision loss, headaches, scalp tenderness, malaise, fatigue, temporal tenderness, jaw claudication, weakness, fever, myalgia, and diplopia)
-
Medications
- Family history of cardiovascular disease, diabetes, systemic hypertension, or hyperlipidemia
- Medical history (e.g., hypertension diabetes, hyperlipidemia, cardiovascular disease, hemoglobinopathy, and polymyalgia rheumatica) or drug history (e.g., cocaine)
- Ocular history (e.g., trauma, other eye diseases, ocular injections, surgery)
- Social history (e.g., smoking)
Physical Exam (Key elements)
-
Visual acuity
-
Slit-lamp biomicroscopy
- IOP
-
Gonioscopy when IOP is elevated or when iris neovascularization risk is suspected (prior to dilation)
-
Relative afferent pupil defect assessment
-
Slit-lamp biomicroscopy of the posterior pole
-
Examination of the peripheral retina using indirect ophthalmoscopy through a dilated pupil to assess: retinal hemorrhages, cotton-wool spots, retinal emboli, retinal vascular “boxcarring,” and optic disc neovascularization and/or neovascularization elsewhere
Diagnostic Tests
-
Color and red-free fundus photography
- OCT
-
Fluorescein angiogram
-
Ultrasonography in the setting of significant media opacity (to rule out other acute causes of vision loss)
- Indocyanine green angiography
Care Management
-
Physicians should first consider GCA in patients 50 years of age or older
-
In cases of GCA, physicians should consider urgent systemic corticosteroid therapy to prevent vision loss in the fellow eye or vascular occlusion elsewhere
-
Diabetics with GCA should be carefully monitored since systemic corticosteroid treatment may destabilize glucose control
-
Ophthalmologists should refer patients with retinal vascular disease to the appropriate setting, depending on the nature of the retinal occlusion
-
Acute, symptomatic OAO, CRAO, and BRAO from embolic etiologies should prompt an immediate referral to the nearest stroke center for prompt assessment for consideration of intervention
-
When presented with an asymptomatic BRAO, clinicians should conduct a systemic evaluation (careful medical history, assessment for systemic disease), preferably in conjunction with the patient's interest
Patient Follow-up
-
Follow-up should consider the extent of retinal or ocular ischemia neovascularization. Patients with greater ischemia require more frequent follow-up
-
Many patients with retinal vascular disease will lose substantial vision despite various treatment options and should be referred for appropriate social services and vision rehabilitation (see www.aao.org/low-vision-and-vision-rehab)
- Follow-up evaluation includes a history (symptoms, systemic conditions) and examination (visual acuity, slit-lamp biomicroscopy with iris examination, IOP, undilated gonioscopy for iris neovascularization, biomicroscopic exam of posterior pole after dilation, peripheral retina and vitreous exam when indicated, OCT imaging when appropriate, fluorescein angiography)
- Patients with asymptomatic BRAO could be referred to a primary care physician
Retinal Vein Occlusions (Initial Evaluation and Therapy)
Initial Exam (Key elements)
-
Location and duration of vision loss
-
Current medications
-
Medical history (e.g., systemic hypertension, diabetes, hyperlipidemia, cardiovascular disease, sleep apnea, coagulopathies, thrombotic disorders, pulmonary embolus)
- Ocular history (e.g., glaucoma, other ophthalmologic disorders, ocular injections, surgery, including retinal laser treatment, cataract surgery, refractive surgery)
Physical Exam (Key elements)
-
Visual acuity
- Pupillary assessment for relative afferent pupillary defect that corresponds to level of ischemia and predictive risk for neovascularization
-
Slit-lamp biomicroscopy to detect fine abnormal new iris vessels
- Measurement of IOP
-
Gonioscopy prior to pupil dilation; especially in cases of an ischemic CRVO, when IOP is elevated, or when iris neovascularization risk is high
-
Binocular funduscopic evaluation of the posterior pole
- Examination of the peripheral retina and vitreous. Slit-lamp biomicroscopy with appropriate lenses is recommended to evaluate retinopathy of the posterior pole and midperipheral retina. Examination of the far peripheral retina is best performed using indirect ophthalmoscopy.
Diagnostic Tests
-
Color fundus and red-free fundus photography for documenting the severity of the retinal findings, NVE, extent of intraretinal hemorrhages and NVD
-
Optical coherence tomography to detect the presence and extent of macular edema, vitreoretinal interface changes and subretinal fluid
- Optical coherence tomography angiography to detect capillary nonperfusion, enlarged foveal avascular zone, and vascular abnormalities
- Fluorescein angiography to evaluate extent of vascular occlusion, degree of ischemia, and extent of macular edema
-
Ultrasonography (e.g., when vitreous hemorrhage is present)
Care Management
-
Optimizing control of diabetes mellitus, hypertension, and hyperlipidemia and IOP are important to manage risk factors
-
Systematic reviews have shown the efficacy of anti-VEGF agents in treating macular edema associated with RVO (I++, GQ, SR)
-
Laser treatment remains a viable treatment in eyes with BRVO, even if the duration of the disease is greater than 12 months
-
Sectoral pan retinal photocoagulation is still recommended for neovascularization when complications such as vitreous hemorrhage or iris neovascularization occur
-
Ophthalmologists caring for patients with retinal vascular occlusion should be familiar with specific recommendations of relevant clinical trials due to the complexity of diagnosis and treatment
Patient Follow-up
- Follow-up evaluation includes a history of changes in symptoms and systemic status (pregnancy, blood pressure, serum cholesterol, and blood glucose) and examination (visual acuity, undilated slit-lamp biomicroscopy and gonioscopy) monthly for 6 months with CRVO and in eyes with ischemic CRVO after discontinuing anti-VEGF to detect neovascularization, pupillary assessment for a relative afferent pupillary defect, measurement of IOP, stereoscopic exam of posterior pole after dilation, OCT imaging when appropriate, and peripheral retina and vitreous exam when indicated
-
Ophthalmologist should refer patients with an RVO to a primary care physician for appropriate management of their systemic condition and communicate results to the physician managing the patient’s ongoing care
-
Risk to the fellow eye should be communicated to both the primary care provider and the patient
-
Patients whose conditions fail to respond to therapy and when further treatment is unavailable should be provided with professional support and offered a referral for counseling, vision rehabilitation (www.aao.org/low-vision-and-vision-rehab), or social services as appropriate