INTRODUCTION
Tuberculosis (TB) is an infection caused by Mycobacterium tuberculosis, which can cause disease in multiple organs throughout the body, including the eye. The term “ocular TB” describes an infection mostly by the M. tuberculosis species that can affect any part of the eye (intraocular, superficial, or surrounding the eye), with or without systemic involvement. “Secondary ocular TB” is defined as ocular involvement as a result of seeding by hematogenous spread from a distant site or direct invasion by contiguous spread from adjacent structures, like the sinus or cranial cavity.
EPIDEMIOLOGY
General Information
- TB is an airborne communicable disease that most commonly involves the lungs.
- Nearly one-third of the world’s population is latently infected with TB, and more than 9 million new cases are diagnosed each year, 95% in developing countries.
- Ocular TB may not be associated with clinical evidence of pulmonary TB; up to 60% of patients with evidence of extrapulmonary TB may not have diagnosed pulmonary TB
- Ocular TB may be an initial presentation of extrapulmonary dissemination of infection
- Posterior uveitis is the most common presentation of intraocular TB.
Table 1. Selected Studies in Which Rates of Ocular Involvement Were Reported Among Patients With Tuberculosis
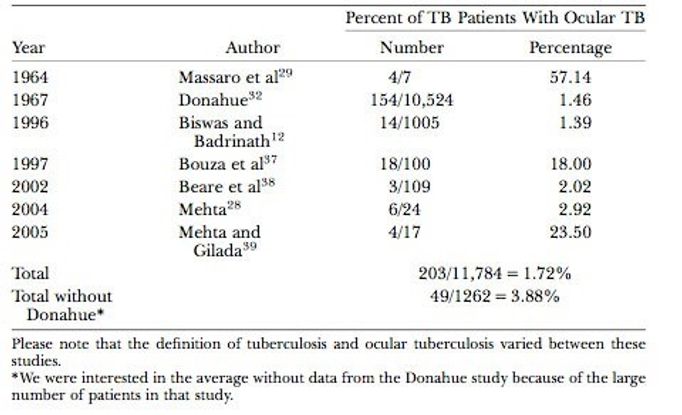
Reproduced, with permission, from Bramante CT, Tabot EA, Rathinam SR, et al. Int Ophthalmol Clin. 2007; 47(3): 45-62.
http://www.aravind.org/content/aravindnews/pdffiles/aug073.pdf
Region-Specific Information (Asia)
|
Country
|
Prevalence of presumed ocular TB
|
|
India
|
0.4-9.8%
|
|
China
|
4.0%
|
|
Japan
|
7.0%
|
|
Thailand
|
2.2%
|
|
Philippines
|
6.8%
|
PATHOPHYSIOLOGY/DEFINITION
Ocular involvement from TB can either occur as a primary active infection or a secondary infection from a distant site, usually through hematogenous spread. Ocular manifestations can result primarily from an active infection that invades the eye or secondarily by an immunologic reaction of delayed hypersensitivity. The conjunctiva, cornea, and sclera are sites of primary ocular involvement.
DIAGNOSIS
Clinical manifestations of ocular TB vary, which poses a challenge for diagnosis. The definitive diagnosis of TB is established by isolation of M tuberculosis bacilli from ocular tissues. However, because this is difficult to achieve, the diagnosis of ocular TB is often presumed in the presence of suggestive ocular findings in combination with any of the following:
- Systemic findings consistent with TB infection
- Positive interferon gamma release assay
- Positive tuberculin skin test in asymptomatic individuals
In addition, clinical response to anti-TB treatment (ATT) further supports a presumed diagnosis of ocular TB.
SIGNS/SYMPTOMS
In general, blurred vision and light sensitivity are the most common symptoms and may be the only reported symptoms. Patients can also be asymptomatic or have other complaints, such as headache, flashes, floaters, or redness of the eye.
- Anterior Uveitis (Figure 1)
- Unilateral or bilateral
- Granulomatous, mutton-fat keratic precipitates
- Iris nodules may be present near pupillary border or on iris surface
- Broad-based posterior synechiae
- Hypopyon may be observed (Figure 2)
- Often accompanied by vitritis
- Posterior Uveitis
- Unilateral or bilateral
- 3 funduscopic patterns:
- Solitary tubercle
- Miliary choroidal tubercles
- Tuberculoma (single large lesion that may mimic tumor) (Figure 3)
- Usually complication of untreated tubercule
- Lesions predominantly present in choroid and can manifest as:
- Serpiginous-like choroiditis (SLC) (Figure 4)
- Multifocal lesions that progress in a serpiginoid pattern and coalesce
- Individual lesions heal centrally and show centrifugal spread in amoeboid fashion
- Usually bilateral, noncontiguous to optic disc and associated with mild vitreous inflammation
- 2 distinct patterns:
- Multifocal, discrete choroidal lesions that are initially noncontiguous and later progress to form diffuse lesions with an active edge resembling serpiginous choroiditis
- Solitary, diffuse plaque-like lesion with an amoeboid extension
Retinal vasculitis: predominantly involving veins with perivascular cuffing with infiltrates; may occur with or without choroiditis
- Choroidal Tubercles (Figure 5)
- Most recognized lesions in intraocular TB
- Yellowish lesions with poorly defined borders and typically elevated centrally
- Commonly situated in posterior pole
- Solitary and few in number
- Inflammatory cells and subretinal fluid may be present
- Tubercles near or at macula present with diminished visual acuity (otherwise, may be asymptomatic)
- Immune recovery uveitis (IRU) (Figure 6)
- Can occur among patients with concurrent HIV and TB infection during antiretroviral therapy
- Has also been reported among patients with HIV and concurrent TB, cytomegalovirus retinitis, and varicella zoster ocular infection.
- Retinal TB
- TB involvement of retina alone is uncommon
- Retina is often involved in setting of choroidal TB as retinochoroiditis
- Exudative retinal hemorrhagic periphlebitis in patient with uveitis is highly suggestive of tubercular etiology
- Orbit
- Orbital involvement occurs most commonly in children, although rare cases have been reported in adults
- Findings include a draining sinus tract and/or radiographic evidence of bony destruction
- Eyelid
- Often presents as an eyelid abscess or chalazion-like mass
- Spontaneous drainage of abscess can form draining sinus tract
- May also become involved as an extension of infection from surrounding skin
- Lacrimal gland
- Can present as symptomatic dacryoadenitis
- Presentation may be indistinguishable clinically from bacterial infection
- Conjunctiva
- May present as an ulcer, subconjunctival nodule, pedunculated polyp, or tuberculoma
- Diagnosis requires excisional biopsy, but the number of organisms is scarce so acid-fast bacilli may not be observed
- Keratoconjunctivitis
- Infection of cornea presents with pain and photophobia
- Examination may demonstrate corneal erosion with stromal infiltration
- Local lymph nodes may be enlarged
- Sclera (Figure 7)
- Involvement of sclera from hematogenous spread
- Diagnosis often based upon evidence of scleral inflammation in patient with active TB
LABORATORY EVALUATION
- Microbiological or histopathological evidence of M tuberculosis
- Acid-fast bacilli (AFB) on direct smear or culture of MTB from ocular samples
- Pros: gold standard, definitive
- Cons: low sensitivity, delayed diagnosis due to slow-growing nature of bacteria
- Tuberculin skin testing (TST)
- Used to assess immunological evidence of MTB infection, latent or active
- Pros: low cost and easy availability
- Cons: two-step process, subjective, low sensitivity and specificity, potential false- positive in prior Bacilli Calmette-Guerin (BCG) vaccinated patients, false-negatives in immunocompromised
- Interferon-gamma release assays (IGRA) (Quantiferon Gold)
- Objective, single-visit blood test that quantifies IFN-gamma response of T cells after in vitro stimulation of patient lymphocytes by MTB antigen
- Pros: more specific, not affected by prior BCG vaccination and atypical mycobacteria
- Cons: not superior to TST in sensitivity, high cost, technical difficulty; does not distinguish between latent and active disease
- Polymerase chain reaction (PCR)
Pros: powerful tool for rapidly detecting mycobacterial genome from small sample of ocular fluid; allows fast detection and quantifies pathogen load in sample, minimal risk of carryover and cross-contamination; can also be helpful in identifying drug-resistant strains of Mycobacterium
- Cons: can still lead to false-negatives from ocular fluid samples
- Chest x-ray (CXR)
- To evaluate patients with suspected intraocular TB, when lungs are primary site of TB infection
- Fluorescein angiography (FA)
- Used in the evaluation of retinal vascular leakage and active choroidal lesions
Reveals moderate to low internal reflectivity of large tuberculomas
Patients diagnosed with active TB should also be tested for HIV due to high incidence of co-infection.
TREATMENT
- Ocular TB is generally treated under the same guidelines for active pulmonary and extrapulmonary TB
- Standard anti-TB treatment (ATT): 6 months of therapy based on WHO recommendations (Figure 8)
- First 8 weeks:
- Rifampin, Isoniazid, Ethambutol and Pyrazinamide
- Next 18 weeks:
- Pulmonary TB patients exhibiting drug resistance are switched to an alternate regimen based on culture reports; the same can be done for progressive ocular inflammation if drug resistance is suspected. Alternatively, escalation of corticosteroids may be helpful in case of increased ocular inflammation in presumed ocular TB.
- Currently, no randomized trials for optimizing therapeutic regimen of anti-TB treatment in intraocular TB
- Corticosteroids (topical and/or oral) may be used to control inflammation and are tapered over 6-12 weeks. Patients may have worsening of inflammation after starting ATT due to a Jarisch-Herxheimer reaction related to release of Mycobacterium antigens upon initiation of antimicrobial therapy. This reaction can be controlled with systemic steroid therapy.
DIFFERENTIAL DIAGNOSIS
- Granulomatous uveitis
- Sarcoidosis (Figure 9)
- Syphilis
- Herpes simplex
- Varicella zoster
- Leprosy
- Vogt-Koyanagi-Harada disease
- Sympathetic ophthalmia
- Choroidal granulomas or Chorioretinitis
CASE STUDY
Age:
Gender:
History of the Present Illness:
- Patient presented to the eye clinic with flare up of acute anterior granulomatous uveitis in the left eye
Past Medical History:
- For 20 years the patient was treated for bilateral recurrent non-granulomatous uveitis with topical steroids and cycloplegics
- 16 years prior to presentation, the patient had an episode of pyrexia associated with chest infection
- She was not treated with ATT because sputum culture was negative
Eye Exam:
- Visual acuity was 20/70 in right eye, 20/100 in left eye
- Posterior segment normal
Laboratory Evaluation:
- 1:1000 Mantoux test (10 TU PPD) strongly positive at 20 mm
Treatment:
Follow up:
- Uveitis completely resolved within 6 weeks of initiating ATT
- No recurrence for more than 1 year
IMAGE LIBRARY
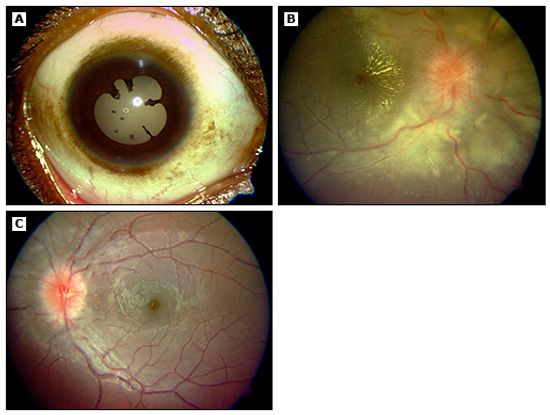
Figure 1. Anterior uveitis due to ocular TB. (Panel A) Granulomatous keratic precipitates and posterior synechiae in 12-year-old girl. (Panel B) Fundus examination shows neuroretinitis in the right eye. (Panel C) Fundus examination shows optic neuritis in the left eye. (©2014 UpToDate®. Reproduced with permission.)
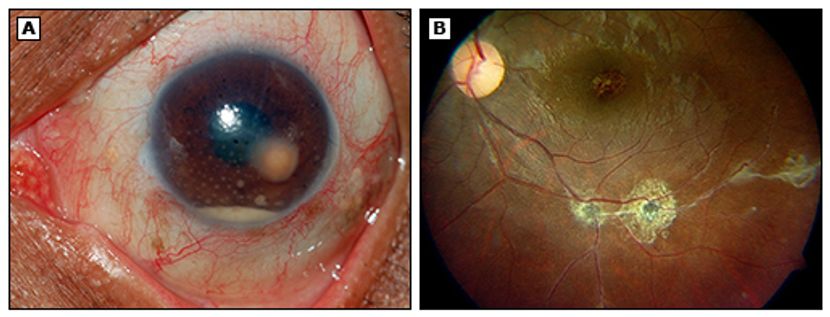
Figure 2. Anterior chamber granuloma due to ocular TB. (Panel A) Anterior chamber granuloma with granulomatous keratic precipitates and hypopyon. Aspiration of the granuloma demonstrated acid fast bacilli in Ziehl-Neelsen stain. (Panel B) Following antituberculous treatment, the posterior segment demonstrates healed pigmented scars along the vasculature. (©2014 UpToDate®)
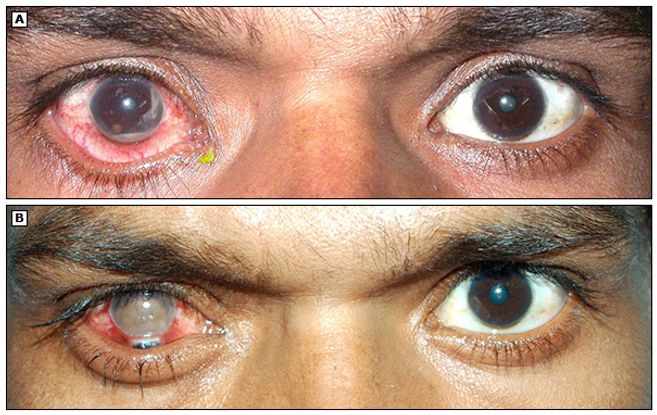
Figure 3. Iris granuloma due to tuberculosis followed by immune recovery tuberculous uveitis. (A) Right eye of a HIV patient with coexisting tubercular uveitis showing iris granuloma and hypopyon. Anterior chamber aspiration revealed acid-fast bacilli, confirming the diagnosis of tuberculosis. (B) Severe form of immune recovery uveitis resulting in perforation of the right eye following highly active antiretroviral therapy (HAART) and antitubercular treatment. Iris is seen prolapsed through the perforation site at the limbus. (©2014 UpToDate® Reproduced with permission.)
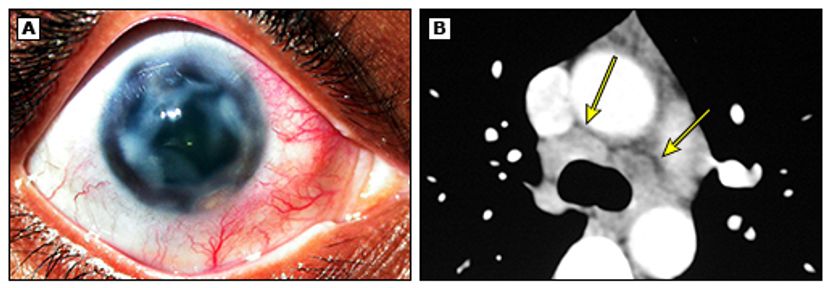
Figure 4. Sclerokeratitis due to ocular TB. (A) Recurrent sclerokeratitis resulting in corneal thinning and melt with adjacent active scleritis. (B) Chest computed tomography (CT) revealed enlarged lymph nodes with necrosis involving pretracheal, paratracheal, and subcarinal groups, with the largest lymph node measuring 1.89 x 1.35 cm. (©2014 UpToDate®. Reproduced with permission.)
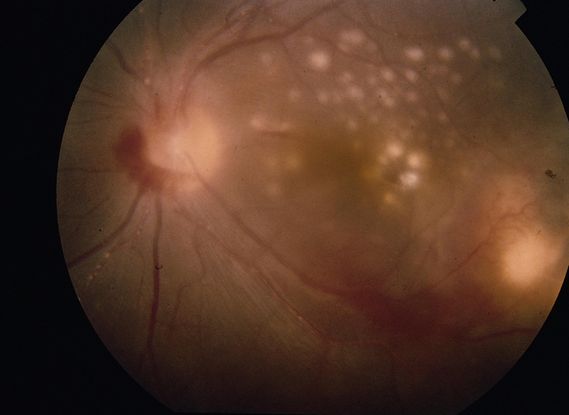
Figure 5. Choroidal tuberculomas. (© 2013 American Academy of Ophthalmology.)
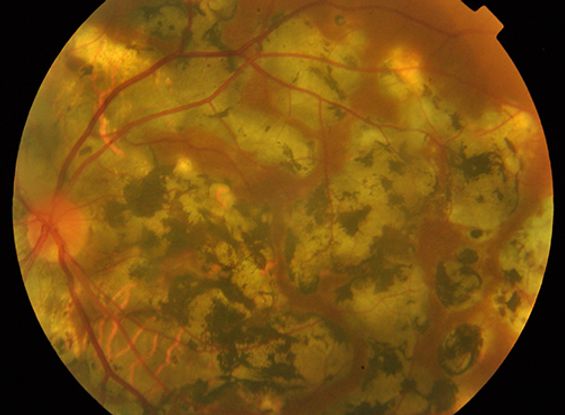
Figure 6. Serpiginous-like choroiditis due to ocular TB. Highly pigmented serpiginous-like choroiditis in a patient with pulmonary TB. (©2014 UpToDate®. Reproduced with permission.)
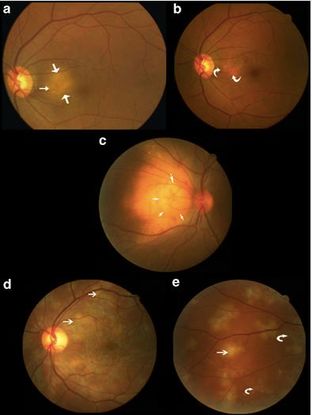
Figure 7. (a, b) Case 1 showing large area of peripapillary choroiditis before and after ATT; (c) Case 2 showing a large choroidal tubercle; (d, e) Case 3 showing multifocal choroiditis before and after ATT. (Straight arrows indicate active lesions and curved arrows healed lesions.) (© 2005 Eye. Reproduced, with permission.)
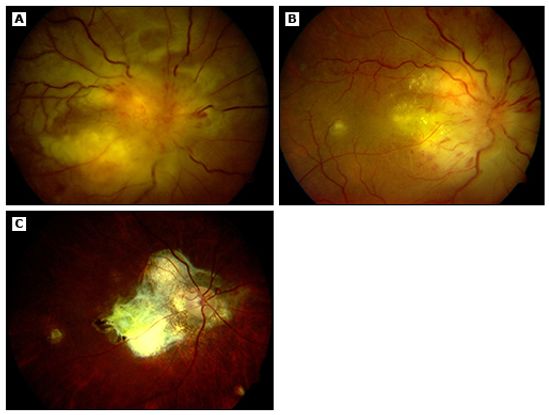
Figure 8. Posterior uveitis due to ocular TB. (A) A 35-year-old woman presented with massive subretinal abscess and optic nerve granuloma with neovascularisation in her left eye. Her Mantoux test was positive and necrotic, and ultrasonography demonstrated thickened choroid. (B) Interval improvement was observed after one month of antituberculous therapy (ATT). (C) Resolution of funduscopic findings and choroidal thickening was observed after three months of antituberculous therapy. (©2014 UpToDate®. Reproduced with permission.)
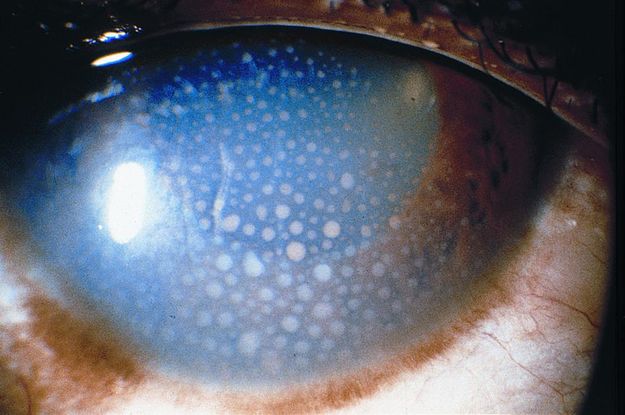
Figure 9. Sarcoidosis. (© 2013 American Academy of Ophthalmology.)
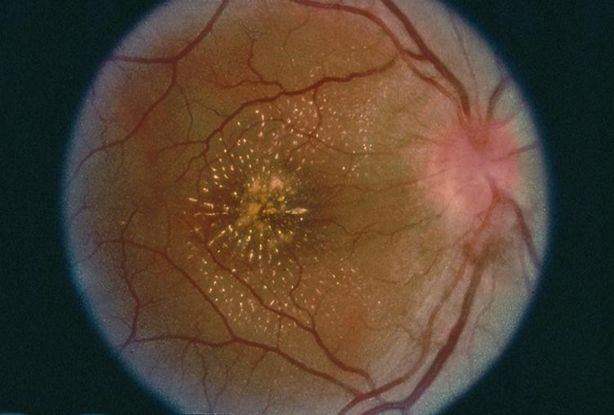
Figure 10. Syphilitic chorioretinitis. (© 2013 American Academy of Ophthalmology. Courtesy of Donald M. Gass, MD.)
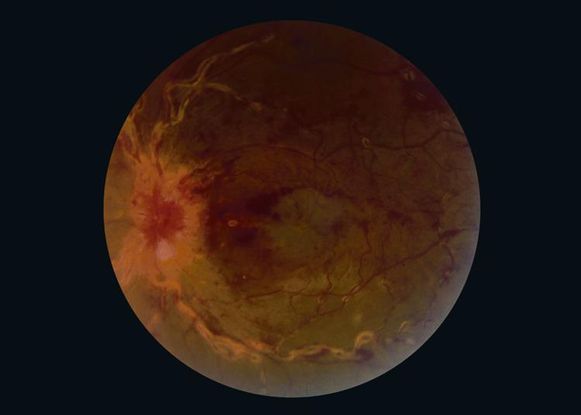
Figure 11. Sarcoidosis. (© 2013 American Academy of Ophthalmology. Courtesy of Ramin Schadiu, MD.)
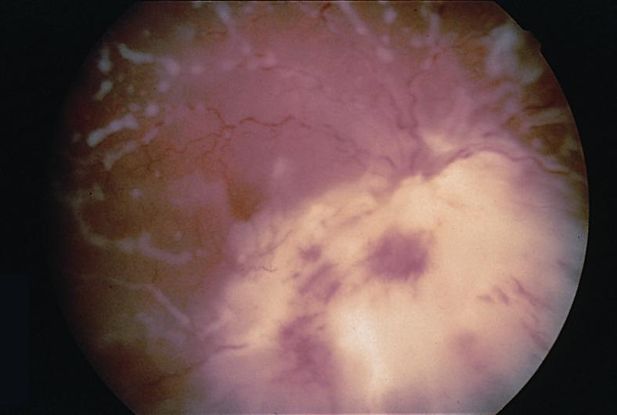
Figure 12. Cryptococcal chorioretinitis. (© 2013 American Academy of Ophthalmology.)
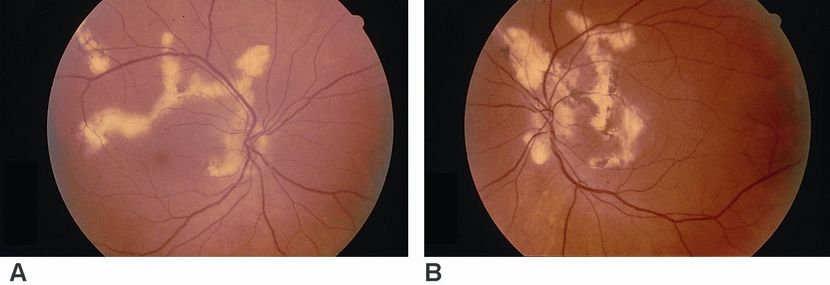
Figure 13 (A,B). Serpiginous choroidopathy. (© 2013 American Academy of Ophthalmology.)
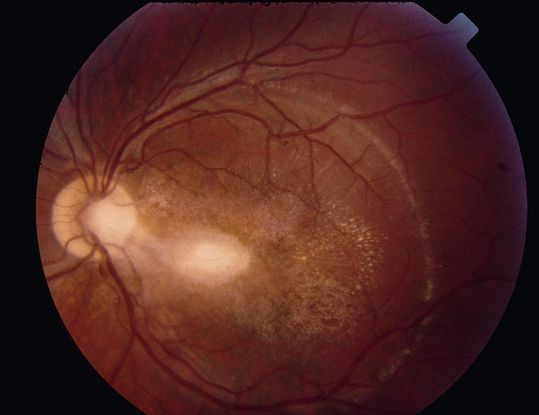
Figure 14. Active toxoplasmic retinochoiditis. (© 2013 American Academy of Ophthalmology.)
REFERENCES
Alvarez S, McCabe WR. Extrapulmonary tuberculosis revisited: a review of experience at Boston City and other hospitals. Medicine (Baltimore). 1984; 63(1): 25–55.
Bansal R, Gupta A, Gupta V, Dogra MR, Bambery P, Arora SK. Role of anti-tubercular therapy in uveitis with latent/manifest tuberculosis. Am J Ophthalmol. 2008; 146: 772-779.
Beare NA, Kublin JG, Lewis DK, et al. Ocular disease in patients with tuberculosis and HIV presenting with fever in Africa. Br J Ophthalmol. 2002; 86: 1076
Bouza E, Merino P, Muñoz P, et al. Ocular tuberculosis. A prospective study in a general hospital. Medicine (Baltimore). 1997; 76: 53
Cutrufello NJ, et al. Intraocular tuberculosis. Ocul Immunol Inflamm. 2010; 18(4): 281–291.
Gupta A, Bansal R, Gupta V, Sharma A, Bambery P. Ocular signs predictive of ocular tuberculosis. Am J Ophthalmol. 2010; 149(4): 562-570.
Sivakumar R. Tuberculosis and the eye. Uptodate. http://www.uptodate.com/contents/tuberculosis-and-the-eye#. Accessed August 29, 2016.
Varma D, Anand S, Reddy A R, et al. Tuberculosis: an under-diagnosed aetiological agent in uveitis with an effective treatment. Eye. 2006; 20 (9):1068-1073.
CONTRIBUTORS
Executive Editor:
R. V. Paul Chan, MD, FACS, Weill Cornell Medical College, New York, New York
Section Editor:
Asia-Pacific:
Timothy Y. Lai, MBBS, MD, MMedSc, FRCS, FRCOphth, FHKAM, Department of Ophthalmology & Visual Sciences, The Chinese University of Hong Kong
Associate Editors:
Jeff Pettey, MD, University of Utah Department of Ophthalmology and Visual Sciences, John Moran Eye Center's Residency Program Director
Grace Sun, MD, Weill Cornell Eye - Lower Manhattan, Weill Cornell Medical College Residency Program Director
Assistant Editors:
Samir Patel, BS, Weill Cornell Medical College, New York, New York
Peter Coombs, MD, Weill Cornell Medical College; New York, New York
American Academy of Ophthalmology
P.O. Box 7424
San Francisco, CA 94120-7424
415.561.8500
Copyright © 2014 American Academy of Ophthalmology®. All Rights Reserved.