EPIDEMIOLOGY
Global Information
- Retinopathy of prematurity (ROP) is a leading cause of preventable childhood blindness in middle-income countries (Gilbert, 2008).
- ROP occurs primarily in infants of low birth weight and low gestational age at birth.
- Most studies report ROP incidences that are about 60% for babies less than 1500 g (Zin and Gole, 2013).
- The worldwide prevalence of blindness due to ROP is approximately 50,000.
- One of the greatest challenges in less-developed countries is having adequate screening done by ophthalmologists trained to diagnose ROP with indirect ophthalmoscopy. Telemedicine with the use of digital imaging and fundus photography may also be a potential strategy for ROP screening in regions where there are few trained ophthalmologists who can manage ROP.
Region-Specific Information (Africa/Middle East)
|
Table 1. Incidence of severe ROP in Africa/Middle East
|
|
Country
|
Definition of Severe ROP
|
Severe ROP Incidence
|
|
Kuwait
|
Treatable ROP
|
7.8%
|
|
Saudi Arabia
|
Treatable ROP
|
1.2 – 6.4%
|
|
Iran
|
ROP any stage
|
8.5%
|
|
South Africa
|
Treatable ROP (CRYO-ROP)
|
4.3%
|
DIFFERENTIAL DIAGNOSIS
- Familial exudative vitreoretinopathy (FEVR)/Norrie (Figure 1)
- Coats disease (Figure 2)
- Persistent fetal vasculature (formerly persistent hyperplastic primary vitreous (Figure 3)
- Retinoblastoma (Figure 4)
- Incontinentia pigmenti (Figure 5)
- Peripheral uveitis/pars planitis (Figure 6)
PATHOPHYSIOLOGY/DEFINITION
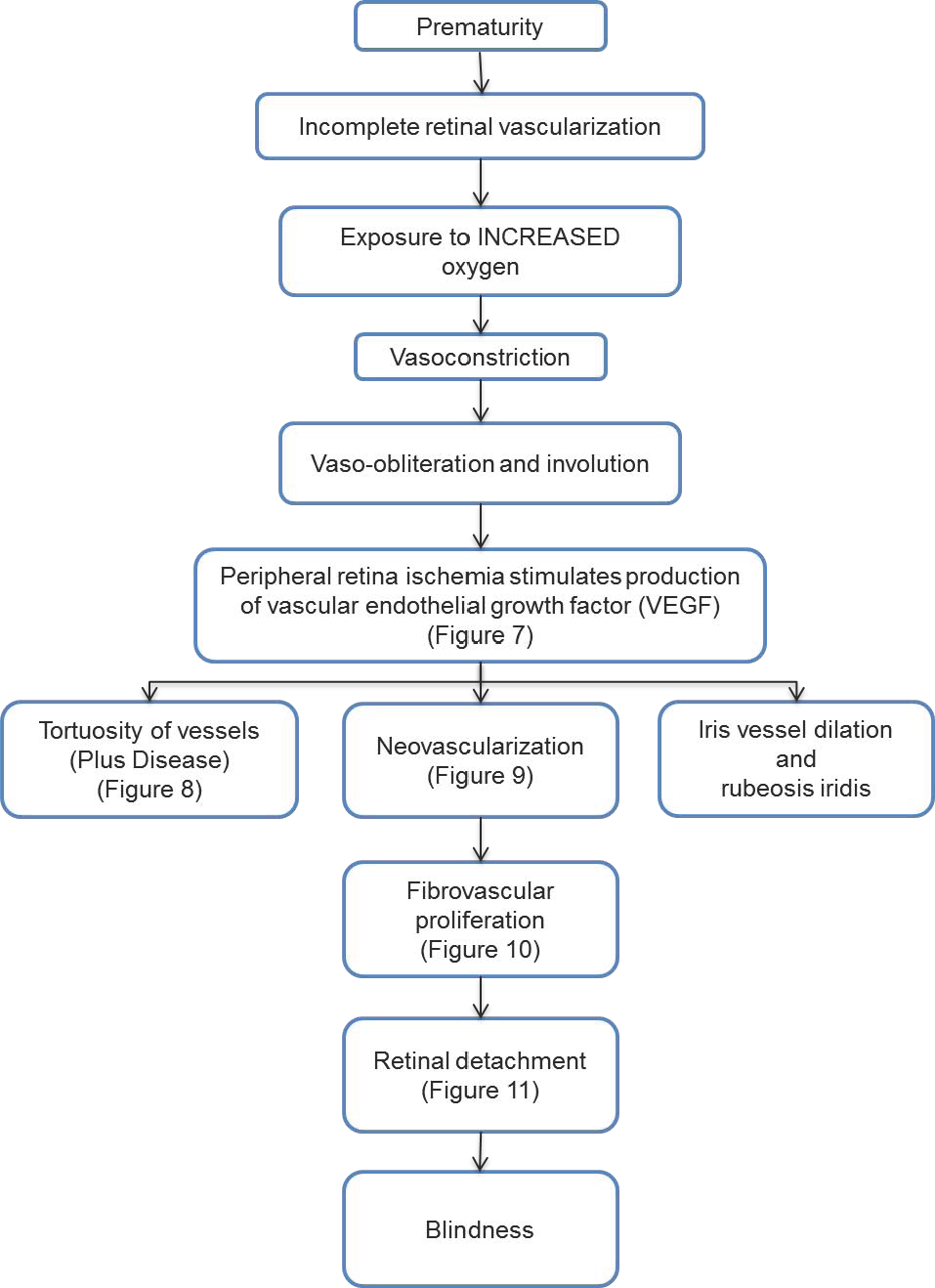
Chart 1. Pathophysiology/Definition. See the Image Library for selected figures.
The following factors may play a role in ROP. They have been shown to be angiogenic in ischemia-induced retinopathies:
- Insulin-like growth factor I (IGF-I)
- Growth hormone
- Angiopoietin (Suri, Jones et al, 1996; Sarlos, Rizkalla et al, 2003)
- Platelet-derived growth factor-β (PDGF-β)
Major Risk Factors
- Prematurity
- Low birth weight
- Hyperoxia
SIGNS, SYMPTOMS
Advanced cases can present with:
- Leukocoria (secondary to retinal detachment)
- Strabismus
MANAGEMENT
- Diagnosis of ROP is made by sequential examinations, indirect ophthalmoscopy, and by digital imaging.
- The International Classification of ROP (ICROP) includes 5 parameters:
- (1) Zone: The location of the disease in the retina (Figure 12)
- Zone I is the posterior retina within 60 degrees of the optic disc
- Zone II is a concentric circle extending from Zone 1 to the nasal ora serrata
- Zone III is the remaining temporal retina
- (2) Clock hours: The extent of the developing vasculature that is involved quantified from 1-12 clock hours
- (3) Stage: The severity of the abnormal vascular changes observed
- Stage 1: Demarcation line between vascularized and non-vascularized retina (Figure 13)
- Stage 2: Demarcation line w/ elevation (Figure 14)
- Stage 3: Demarcation line with fibrovascular proliferation (Figure 15)
- Stage 4a: Partial detachment of retina not involving fovea (Figure 16)
- Stage 4b: Partial detachment of retina involving fovea (Figure 17)
- Stage 5: Total retinal detachment (Figure 18)
- (4) Plus disease: Venular dilation and arteriolar tortuosity in the posterior pole
(Figure 19)
- (5) Pre-plus disease Abnormal-appearing vasculature that does not make criteria for Plus disease (Figure 20)
- Aggressive posterior ROP (AP-ROP) is a severe form of ROP that rapidly causes total retinal detachment without going through the normal stages of ROP (Figure 21).
- AP-ROP (zone I or -posterior zone II) needs especially close follow-up.
Screening
- The Revised Joint Policy Statement issued in 2013 by the American Academy of Pediatrics, the American Association of Pediatric Ophthalmology and Strabismus, and the American Academy of Ophthalmology provides guidelines on screening and follow-up of premature neonates (Table 2).
- Indications for screening are region dependent. Those in Table 2 are guidelines by American physicians.
- In the United States premature neonates are examined for ROP if they have a birth weight of less than or equal to 1500 g or a gestational age of 30 weeks or less. Select infants with a birth weight between 1500 g and 2000 g or a gestational age at birth of greater than 30 weeks with an unstable clinical course should also have an eye exam.
|
Table 2. Screening Guidelines for Retinopathy of Prematurity
|
|
Screening Interval
|
Disease Features
|
|
1 week or less follow-up
|
- Zone I retinal vessels ending without ROP, stage 1 or 2 ROP
- Zone II, Stage 2 or 3 ROP
|
|
1 to 2 week follow-up
|
- Zone I, regressing ROP
- Zone II, Stage 1 ROP
|
|
2 week follow-up
|
- Zone II, Stage 1 or regressing ROP
|
|
2 to 3 week follow-up
|
- Zone II, immature vascularization without ROP
- Zone III, Stage 1 or 2 or regressing ROP
|
TREATMENT
- Treatment is based on 2 multicenter trials: the Cryotherapy for Retinopathy of Prematurity (CRYO-ROP) trial and the Early Treatment for Retinopathy of Prematurity (ETROP) trial (CRYO-ROP Cooperative Group, 1988 and ETROP Cooperative Group, 2008)
- Laser photocoagulation is the preferred treatment of choice. If laser is not available, cryotherapy may be performed.
- Laser photocoagulation is performed when ROP reaches type 1 pre-threshold disease. See Table 3.
- It is important to diagnose aggressive posterior ROP (AP-ROP) and treat it immediately, as this form of ROP can rapidly progress to retinal detachment.
|
Table 3. Disease Features of Pre-threshold Disease in Retinopathy of Prematurity
|
|
Type 1 ROP
|
- Zone I, any stage ROP with Plus disease
- Zone I, Stage 3 ROP without Plus disease
- Zone II, Stage 2 or 3 ROP with Plus disease
|
|
Type 2 ROP
|
- Zone I, Stage 1 or 2 ROP without Plus disease
- Zone II, Stage 3 ROP without Plus disease
|
Anti-VEGF Injections
Intravitreal injections of anti-vascular endothelial growth factor (Anti-VEGF) may cause rapid resolution of AP-ROP (Mintz-Hittner et al., 2011). However, laser photocoagulation remains the standard of care for most cases of treatment requiring ROP.
Surgery
- If laser or cryotherapy fails to prevent progression of ROP and the patient develops a retinal detachment, surgery (vitrectomy, scleral buckle) may be performed.
- Results are best when done before the fovea has detached.
- Stage 5 ROP has a poor visual prognosis
Follow-Up
Patients with a history of ROP have a higher incidence of astigmatism, high myopia, and retinal detachment and should be followed routinely.
IMAGE LIBRARY
Differential Diagnosis
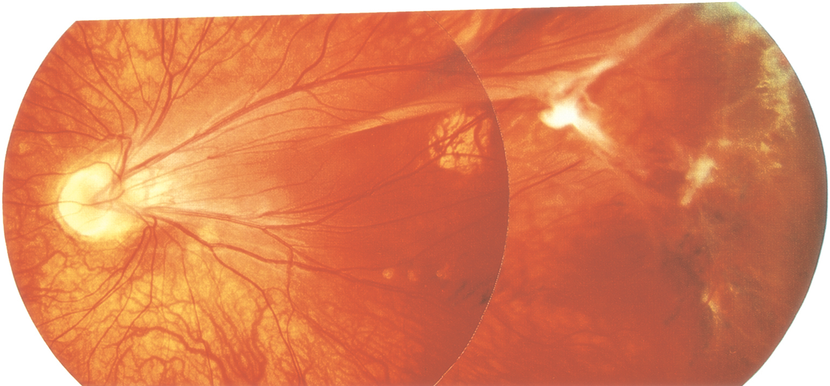
Figure 1. Familial exudative vitreoretinopathy (FEVR)/Norrie. (© 2013 American Academy of Ophthalmology.)

Figure 2. Coats disease. (© 2013 American Academy of Ophthalmology.)
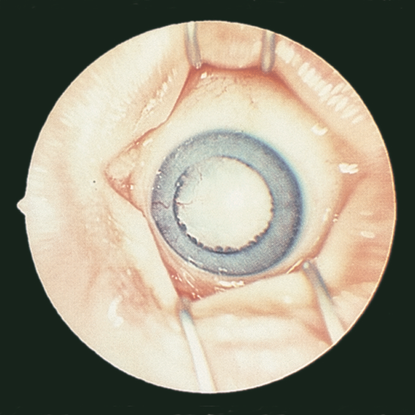
Figure 3. Persistent fetal vasculature (formerly persistent hyperplastic primary vitreous). (© 2013 American Academy of Ophthalmology.)
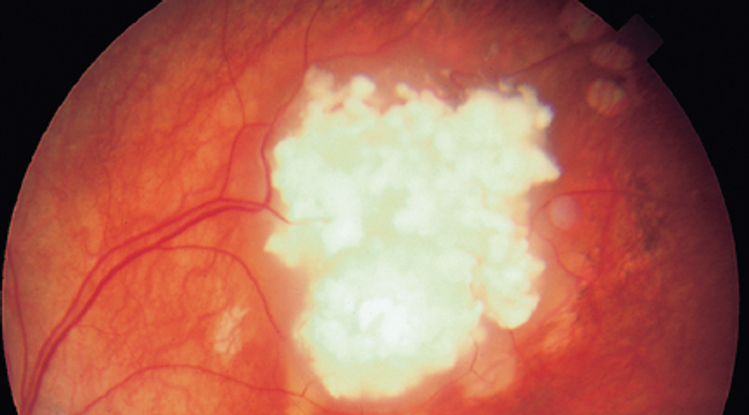
Figure 4. Retinoblastoma. (© 2013 American Academy of Ophthalmology.)
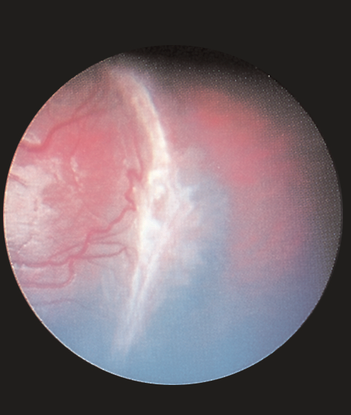
Figure 5. Incontinentia pigmenti. (Reproduced, with permission, from Lueder GT. Pediatric Ophthalmology and Strabismus.Basic and Clinical Science Course, Section 6, American Academy of Ophthalmology, 2013–2014.)
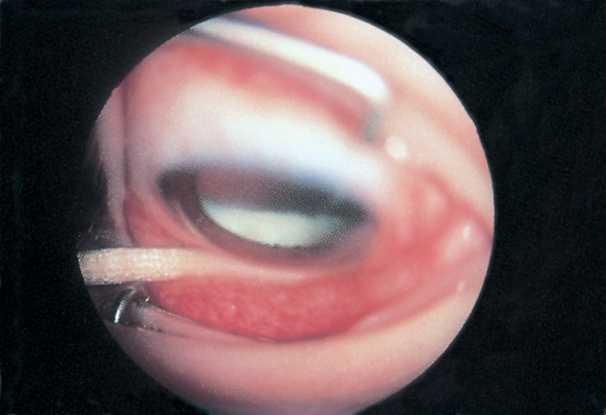
Figure 6. Peripheral uveitis/pars planitis. (Reproduced, with permission, from Lueder GT. Pediatric Ophthalmology and Strabismus.Basic and Clinical Science Course, Section 6, American Academy of Ophthalmology, 2013–2014.)
Pathophysiology/Definition
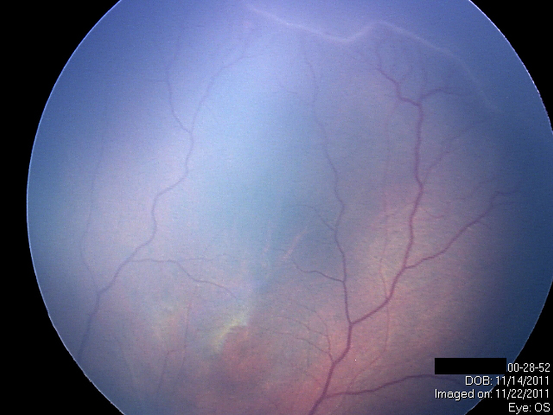
Figure 7. Peripheral retina ischemia. (Courtesy of Sjakon G. Tahija, SpM.)

Figure 8. Tortuosity and dilation of the vessels in the posterior pole (Plus disease). (Courtesy of Sjakon G. Tahija, SpM.)
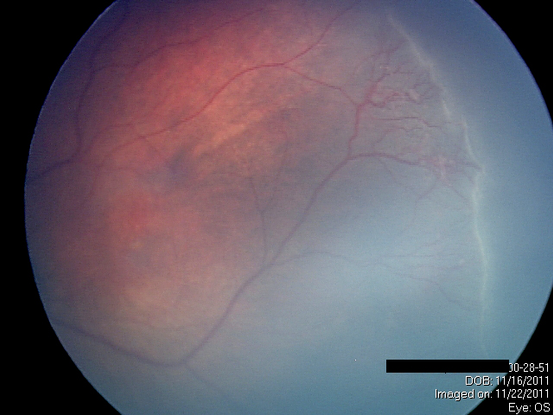
Figure 9. Neovascularization. (Courtesy of Sjakon G. Tahija, SpM.)
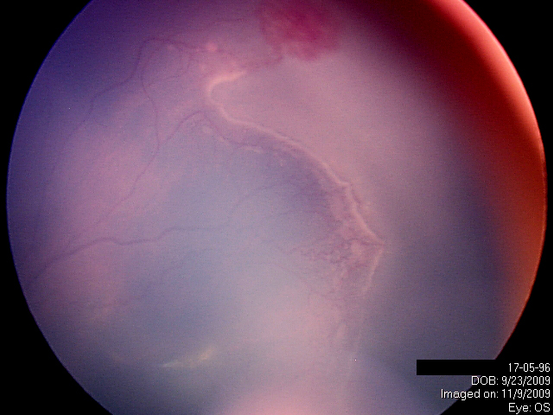
Figure 10. Extraretinal fibrovascular proliferation. (Courtesy of Sjakon G. Tahija, SpM.)
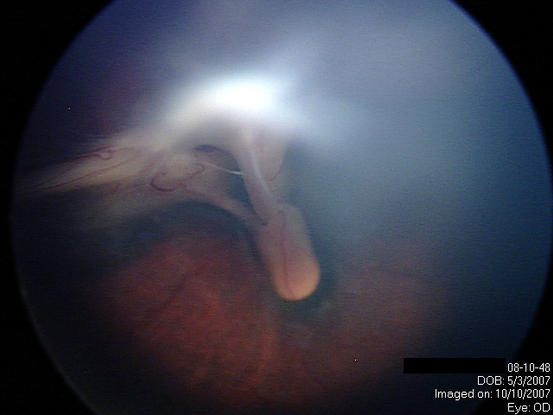
Figure 11. Retinal Detachment. (Courtesy of Sjakon G. Tahija, SpM.)
Management
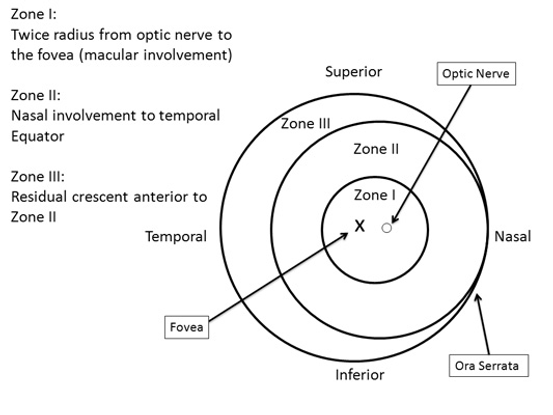
Figure 12. Zones depict the location of the disease in the retina. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
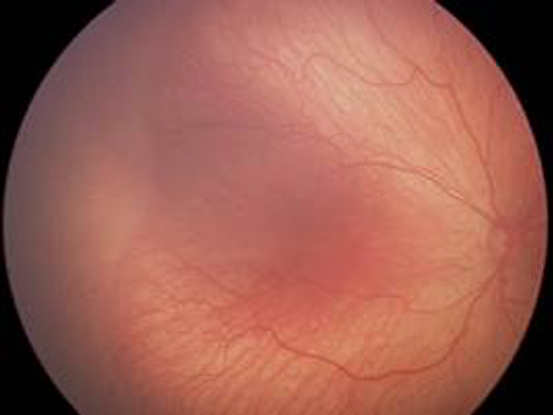
Figure 13. International Classification of ROP, Stage 1. Demarcation line between vascularized and vascular retina. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
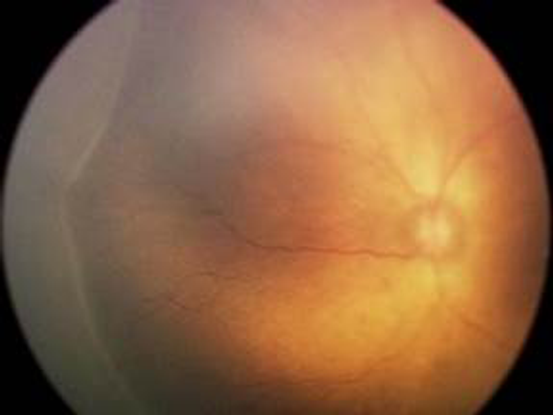
Figure 14. International Classification of ROP, Stage 2. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
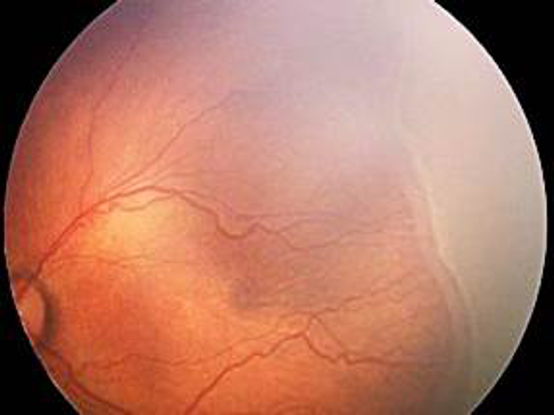
Figure 15. International Classification of ROP, Stage 3. Extraertinal fibrovascular proliferation. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
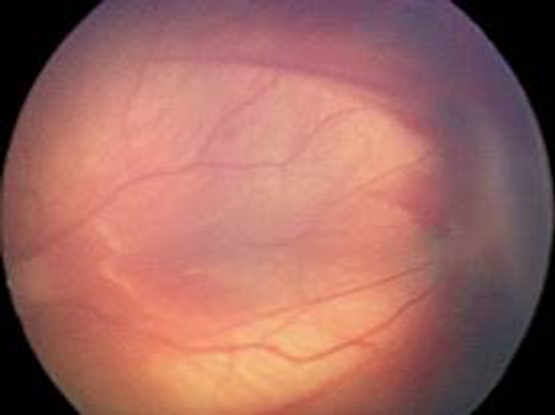
Figure 16. International Classification of ROP, Stage 4a. Partial detachment of the retina not involving the fovea. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
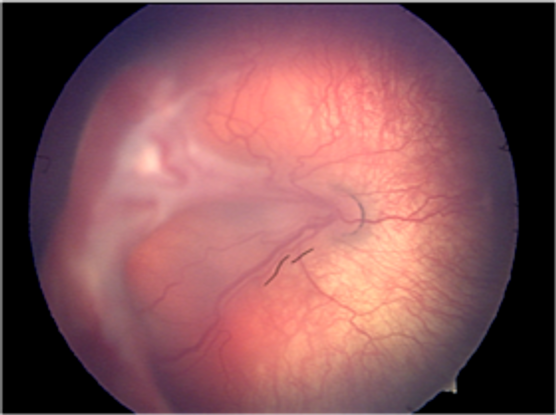
Figure 17. International Classification of ROP, Stage 4b. Partial detachment of the retina involving the fovea. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
Figure 18. International Classification of ROP, Stage 5. Total retinal detachment. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
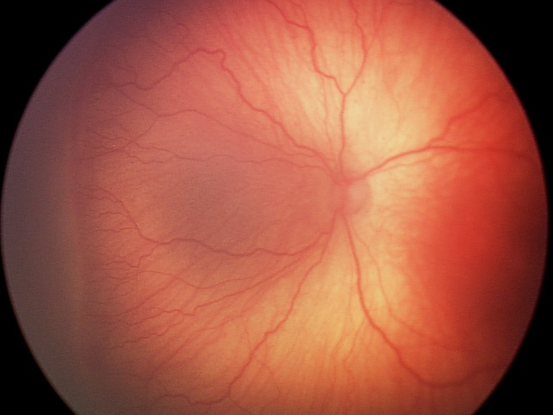
Figure 19. Pre-plus disease. Abnormal-appearing vasculature that does not meet criteria for Plus disease. (Courtesy of R.V. Paul Chan, MD, FACS and Michael F. Chiang, MD.)
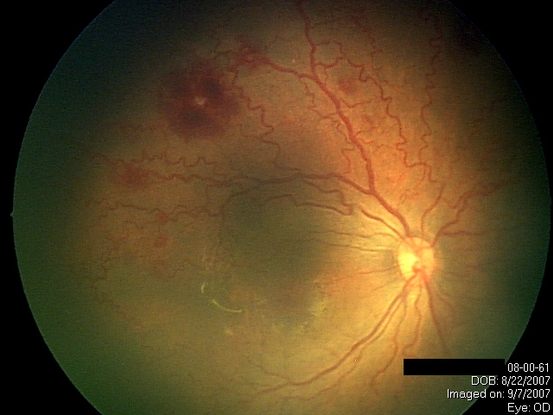
Figure 20. Aggressive Posterior ROP (AP-ROP)is a severe form of ROP that rapidly causes total retinal detachment without going through the normal stages of ROP. (Courtesy of Sjakon G. Tahija, SpM.)
REFERENCES
[No authors listed.] An international classification of retinopathy of prematurity. The Committee for the Classification of Retinopathy of Prematurity. Arch Ophthalmol. 1984;102:1130–1134.
[No authors listed.] Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 1988;106:471–479
Carden SM, Luu LN, Nguyen TX, Huynh T, Good WV. Retinopathy of prematurity: postmenstrual age at threshold in a transitional economy is similar to that in developed countries. Clin Experiment Ophthalmol. 2008;36:159–161.
Early Treatment For Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–1694.
Early Treatment for Retinopathy of Prematurity Cooperative Group. Grating visual acuity results in the early treatment for retinopathy of prematurity study. Arch Ophthalmol. 2011;129:840–846.
Flynn JT, Chan-Ling T. Retinopathy of prematurity: two distinct mechanisms that underlie zone 1 and zone 2 disease. Am J Ophthalmol. 2006;142:46–59.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–999.
Lad EM, Hernandez-Boussard T, Morton JM, Moshfeghi DM. Incidence of retinopathy of prematurity in the United States: 1997 through 2005. Am J Ophthalmol. 2009;148:451–458.
Larsson E, Carle-Petrelius B, Cernerud G, Ots L, Wallin A, Holmström G. Incidence of ROP in two consecutive Swedish population based studies. Br J Ophthalmol. 2002;86:1122–1126.
Mintz-Hittner HA, Kennedy KA, Chuang AZ; BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;17;364:603–615.
Section on Ophthalmology, American Academy of Pediatrics, American Academy of Ophthalmology and American Association for Pediatric Ophthalmology and Strabismus. Joint Policy Statement AAO, AAP, and AAPOS on screening examination of premature infants for retinopathy of prematurity. September 2006.
Zin A, Gole GA. Retinopathy of prematurity-incidence today. Clin Perinatol. 2013;40:185-200.
CONTRIBUTORS
Section Editors:
North Africa/Middle East:
Ebtisam S. Kadhem Al-Alawi, FRCS, MRCOpht, DO, Salmaniya Medical Center, Bahrain
Assistant Editors:
Swetangi D. Bhaleeya, MD, Weill Cornell Medical College; New York, New York
Kristin Chapman, MD, Weill Cornell Medical College, New York, New York
Peter Coombs, MD, Weill Cornell Medical College; New York, New York
Michael Klufas, MD, Weill Cornell Medical College, New York, New York
Samir Patel, medical student, Weill Cornell Medical College; New York, New York
Copyright © 2013 American Academy of Ophthalmology®. All Rights Reserved.