A good history and physical is key for achieving a high rate of diagnostic success when assessing a patient with cataract. However, sometimes ancillary imaging can assist you in diagnoses and help you anticipate any intraoperative issues.
Here are five tips for using anterior-segment imaging to produce the best surgical outcomes.
1. Determine Whether Cataract Is Indeed the Cause
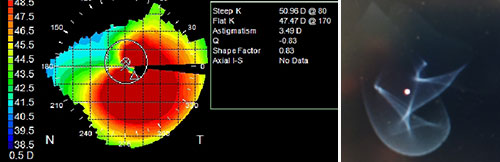
Is the vision proportional to the cataract appearance? This appears self-evident; however, often a cataract referral will arrive when another pathology is the predominant source of the decreased vision. So if the change in the lens is not consistent with the decrease in vision, consider adjunct testing in the form of corneal topography/tomography (see Figure 1) or macular optical coherence tomography (OCT). Clinical aberrometers such as wavefront sensors or ray-tracing technology also can be helpful in characterizing deviations in the optics of the eye and explaining symptoms that overlap with those commonly caused by cataracts.
 |
|
Figure 1. Findings of ectasia as evidenced by irregular astigmatism and inferior steepening.
|
2. Look Beyond Complex IOL Calculations
Advanced testing in the form of topography, anterior-segment OCT or other high-resolution corneal imaging, such as high-frequency ultrasound, is important for any cataract surgery — especially in the context of prior corneal refractive surgery.
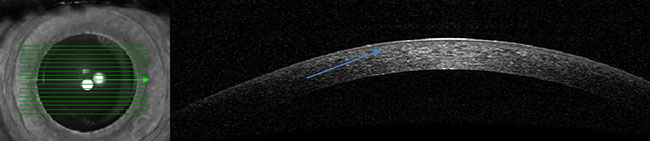
However, it is often helpful to know the flap depth and diameter (especially in the case of hyperopic ablations with larger flaps) so that you can avoid entering a flap interface with a long anterior multiplanar keratome wound (see Figure 2).
In these circumstances, scleral tunnel-based incisions for cataract surgery may help. You also can apply the same approach to patients who have had endothelial surgery (Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty) if originally performed without simultaneous cataract surgery.
3. Employ Anterior-Segment Imaging to Assist in MIGS
Gonioscopy is mandatory for any cataract surgery with adjunct micro-invasive glaucoma surgery (MIGS). However, anterior-segment imaging like OCT or ultrasound biomicroscopy can help quantify with measurable detail the anatomical spacing that could house stenting devices and can help inform surgical approaches for altering the angle anatomy, including canal procedures or a goniotomy. These imaging technologies will assist in postoperative assessments as well.
 |
|
Figure 2. Anterior-segment OCT to help delineate a prior LASIK flap.
|
4. Keep an Eye on Abnormal Cataracts
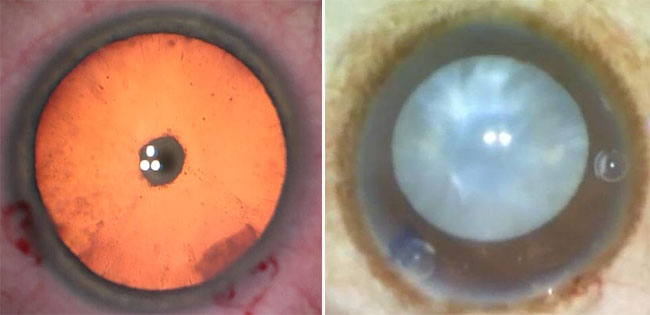
B-scan ultrasonography is necessary for mature cataracts in which the lens opacity precludes the observation of any vision-threatening posterior-segment anomalies. This type of imaging is especially important when dealing with posterior polar cataract, as it can help determine whether the lens is fused to the posterior capsule (see Figure 3). B-scan ultrasonography also can help you anticipate any surgical complications or anatomical limitations, such as the inability to perform hydrodissection.
 |
|
Figure 3. Posterior polar cataract (left) and a mature cataract (right).
|
5. Make Investments in Technology
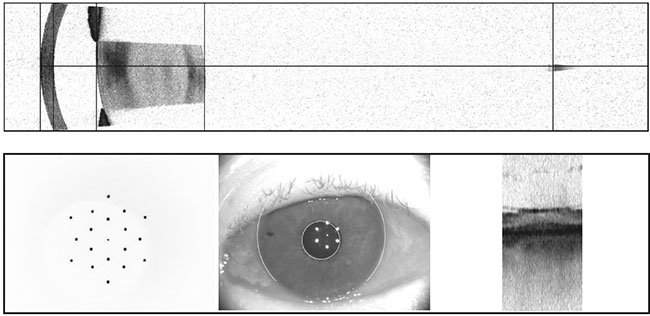
Optical biometry has been a common test for decades and is critical for appropriately assessing cataracts in the context of IOL power selection. This traditional test recently has become more sophisticated with adjunct imaging technologies such as swept-source OCT, which can assist patients and surgeons alike when discussing the nuances of cataract treatment or anticipating surgical challenges (see Figure 4).
When associated with femtosecond laser-assisted cataract surgery, intraoperative imaging, such as OCT, also will provide in vivo images during the surgical procedure. In addition, intraoperative aberrometry and other technologies, such as superimposable video imaging systems, can help with toric alignment, IOL centration and refractive effects in a live fashion.
Having at least one device with some advanced anterior-segment imaging (swept-source OCT or Scheimpflug-based imaging) will help you handle a broader array of cataract surgeries and avoid situations in which cataract surgery may not yield the ideal result. Postoperatively, some of these devices also may be helpful for critically assessing IOL centration, pantoscopic tilt and other factors that can affect surgical outcomes.
 |
|
Figure 4. Optical biometry via swept-source OCT demonstrating anatomy, fixation and general anatomic landmarks of the eye.
|
* * *
About the author: Hoon C. Jung, MD, is an assistant professor in the University of Washington’s Department of Ophthalmology. Dr. Jung received his medical degree from the University of Rochester. He completed his internship in Johnson City, NY, ophthalmology residency at the University of Buffalo and cornea, external disease and refractive surgery fellowship at the University of Rochester.