Visual field (VF) testing, although sometimes described as “torturous” by our patients, can be gratifying (and important) to interpret as an ophthalmologist, especially when done systematically.
This article provides quick pearls and a framework by which you can conquer interpretation of VFs and points you in the direction of relevant comprehensive resources.
First build a foundation. The Academy’s Basic and Clinical Science Course™ (BCSC®) and EyeWiki are particularly useful resources for learning the types of perimetry (static vs. kinetic), stimulus size and luminance and the difference between common testing strategies. They also present the basics about the most common automated static perimetry machines like Humphrey and Octopus.
 |
|
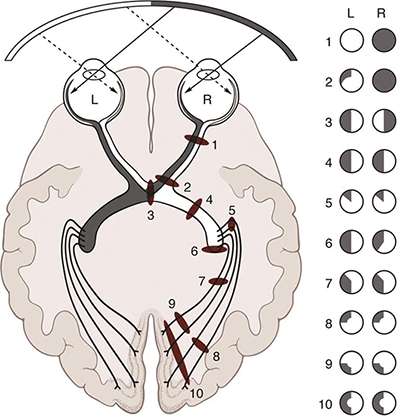
Examples of visual field defects along the visual pathway.
|
Take a VF yourself. This will allow you to sympathize with and explain the test to the patient if necessary. Don’t freak out if it’s not normal the first time. There is a significant “learning effect,” during which patients often become better test-takers over the first few VFs.
Familiarize yourself with the test printout from top to bottom. The EyeRounds article “Visual Field Testing: From One Medical Student to Another” has a helpful diagram and explanation of reliability indices, deviation maps and summary outputs.
Always interpret VFs systematically to avoid oversight of clinical importance. Follow these five steps or develop your own approach.
1. Is the test reliable? Look out for long test duration and false positives, false negatives or fixation losses >20%. False positives may underestimate defects; false negatives may represent a patient’s inattention or a patient with significant VF loss.
2. Have you ruled out common artifacts? These include cloverleaf artifacts (suggestive of malingering or a decrease in attention during the test), lid artifacts (may improve with lid taping) and rim artifacts (related to lens positioning and/or head positioning). Be sure to check out the Academy’s BCSC for in-depth illustrations of the most common artifacts and other pertinent details.
If patients have persistently unreliable VFs, their reliability may improve with a larger stimulus and/or faster test strategy. Never underestimate the importance of explaining test instructions or informing the patient that the Humphrey test will pause if the response button is held down (in case they need a break).
3. Is there a significant defect? Look for a cluster of two or more defects, and look at the summary data, including mean deviation, pattern standard deviation, visual field index (VFI) and the glaucoma hemifield test. (EyeWiki does a great job of simplifying this.) It’s also important to identify any VF correlation with a structural defect (on the opposite side of the nerve). In most cases, a true functional VF defect will have a corresponding notch, pallor or edema on exam or optical coherence tomography (OCT).
4. Where is the pathology? Be sure to think outside the box and rule out life-threatening patterns that respect the vertical midline and/or are homonymous. This requires careful VF examinations of both eyes simultaneously. These patterns could signify pituitary or optic tract abnormalities that require urgent evaluation and/or treatment. (The EyeRounds article has a compilation of patterns to familiarize yourself with).
After these are ruled out, look for glaucomatous patterns such as a nasal step, arcuate scotoma, bjerrum scotoma or paracentral defects. (The BCSC has some great examples.)
5. Is there evidence of progression? Look for change yourself, by comparing the current VF to the last one as well as the baseline. If a change has occurred, it is important to understand when and what the ocular vital signs were at that time.
Computerized progression analysis is also important to consider but not to rely on. Event-based progression analysis such as guided progression analysis highlights change from a prior or baseline VF. Trend-based progression analysis such as VFI calculates the rate of change. There are advantages and disadvantages to each method, and in many cases, only the physician can identify and exclude artifact.
If you believe there is progression on VF in a glaucoma patient, but no other red flags (intraocular pressure, OCT, disc hemorrhage), the gold standard is to confirm true progression with a repeat VF test.
Hopefully this framework will empower you to make the most of each visual field test — for patient care and also for your own education!
* * *
 Natasha Nayak Kolomeyer, MD,
Natasha Nayak Kolomeyer, MD, is a glaucoma specialist at Wills Eye Hospital in Philadelphia and joined the
YO Info editorial board in 2019.