Glaucoma is a tip-of-the-iceberg phenomenon. At first glance, it seems simple (just lower the IOP!), but it can abruptly reveal its true nature the deeper you delve. How do you face such an opponent? Be alert, dynamic to change and willing to respond in kind as soon as glaucoma shows you an aggressive side. Follow these tips to handle glaucoma with confidence.
Get gonio comfy
Find the fit
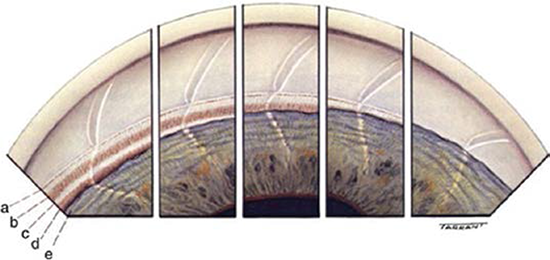
The Normal Angle. Various widths of the normal angle seen in consecutive inserts. Note that the corneal optical wedge narrows as it approaches Schwalbe’s line and seems to end there in the situation of a narrow angle. (a) Schwalbe’s line. (b) Trabecular meshwork. (c) Scleral spur. (d) Ciliary body band. (e) Peripheral iris.
(Image courtesy of Terry Tarrant; Alcon Labs, Fort Worth, Texas, and www.entokey.com.)
Many of us don’t feel completely at ease with gonioscopy. Let’s face it: It takes a delicate maneuver just to get a view of the angle. And once you do, what are you supposed to make of what you see? First, figure out what tool feels most comfortable in your hands. You have several body styles of gonioscopy lenses to choose from, and they may not be equally interchangeable for you. Use residency to explore your options and then commit to your own lens. You are much more apt to gonio a patient when you have your favorite lens ready in your pocket.
Learn the angles
Some angles are just tough! One pitfall is to mistake the Sampaolesi line for trabecular meshwork in a narrow angle where something obstructs the true trabecular meshwork. In this case, use the corneal wedge to delineate where Schwalbe’s line ought to be, and use dynamic gonioscopy with indentation to assess the extent of the drainage structures you can see.
When dealing with an anteriorly bowed iris, you may get a better look “over the hill” by tilting your gonio lens towards the angle being viewed or having the patient look toward your viewing mirror on the lens. All this business of being upside down and backwards with indirect gonioscopy is confusing! Check out Gonioscopy.org for helpful resources on these difficult angle techniques and more.
Practice, practice, practice!
The more angles you look at, the more natural it becomes to get a good view while reinforcing the “normal” angle in your mind. Then, when something different comes along, you’re more apt to catch it. All the images and videos in the world can’t replace your own experience, so just do it and do it often. One day, you’ll realize that it’s not so bad and that you’re actually pretty good at it!
Keep up with changes in surgery
In recent years, an explosion of newer techniques and devices has supercharged the field of glaucoma surgery, including the Ex-PRESS shunt, the iStent, canaloplasty, the Trabectome, the Kahook Dual Blade, gonioscopy-assisted transluminal trabeculotomy, the CyPass Micro-Stent, the InnFocus MicroShunt, the Hydrus Microstent and the Xen gel stent, as well as endoscopic cyclophotocoagulation and micropulse cyclophotocoagulation. Some devices are still pending FDA approval.
Many of the surgeries overlap in concept and territory. You may not need to practice them all, but it behooves you to gain a basic understanding of the available spectrum so you know what options your patients may be referred for.
Don’t fret if you are not exposed to any of these innovations during residency; those three years are meant to build your foundation of ophthalmic knowledge. You’ll learn most of your career knowledge after graduation.
You can discover more about these hot topics of discussion on Internet and video forums (EyeTube and even YouTube), journal publications and ophthalmology conferences like AAO 2017 in New Orleans, the biggest meeting in the profession. Be sure to also consider conferences with wet-lab workshops that offer hands-on coaching.
If you are really interested in bringing a new item into your practice, a good starting point is the device rep, who will always be happy to visit you. In some instances, you may also need to complete a certification process to use the device.
* * *
 About the author: Jiaxi Ding, MD, is in practice with Carolina Eye Associates in North Carolina, where she specializes in glaucoma. She joined the YO Info editorial board in 2016.
About the author: Jiaxi Ding, MD, is in practice with Carolina Eye Associates in North Carolina, where she specializes in glaucoma. She joined the YO Info editorial board in 2016.