When billing for office visits, ophthalmologists have two options or types of office visit codes to choose from: evaluation and management (E/M) codes (992XX) and eye visit codes (920XX). One of the most frequent questions we receive at coding@aao.org is, “Which one should I use?”
To answer this question, you’ll need to learn about the E/M and eye visit codes, know when not to bill an eye code for a visit, and familiarize yourself with certain procedures and the appropriate codes.
Differences Between E/M and Eye Visit Codes
First and foremost, you need to understand the unique documentation requirements for the two options.
E/M codes
On Jan. 1, 2021, office-based E/M codes were completely redefined. With these updates, the office or other outpatient services use either 1) medical decision-making (MDM) or 2) total physician time to select a code level. History and examination elements are not used in code selection but still need to be documented as medically relevant. You as the physician decide what is medically necessary for each history and examination. The critical medical decision-making component is comprised of three different components:
- The number and complexity of problems addressed at the encounter
- The amount and/or complexity of data to be reviewed and analyzed
- The risk of complications and/or morbidity or mortality of patient management
To determine the level of E/M code, you can use the Academy’s Final Determination Table for Medical Decision-Making tool along with aspects of the three components above. You must meet or exceed two of three categories at the same level of complexity for E/M code selection. Make sure your documentation supports your billing level.
Additional information and examples for E/M codes can be found at aao.org/em.
Eye Visit Codes
The Eye visit codes for both new and established patients have two classifications: comprehensive and intermediate. The Academy has developed guidance on how to appropriately document for both intermediate and comprehensive Eye visit code services outlined in the chart below.
|
Documentation Component
|
Eye Visit Code Comprehensive Exam Components
|
Eye Visit Code Intermediate Exam Components
|
|
|
CPT codes 92004 and 92014
|
CPT codes 92002 and 92012
|
|
History
|
- History (not defined)
- General medical observation (not defined)
- Chief Complaint
|
- History (not defined)
- General medical observation (not defined)
- Chief Complaint
|
|
Exam
|
Exam: all 12 elements of the exam
|
Exam: 3 or more, but less than 12 elements of the exam medically necessary to perform
|
|
Impression/Plan
|
Initiation or continuation of diagnostic and treatment programs
|
Initiation or continuation of diagnostic and treatment programs
|
The history and general medical observations requirements are not defined. Chief complaint, the reason why the patient is there, is always required. Eye visit codes always require the initiation or continuation of diagnostic and treatment programs and may include, but are not limited to: prescribing medication, arranging for special ophthalmological diagnostic or treatment services, consultations, laboratory procedures and radiological services. Essentially you need to state what the problem is and what you recommend doing about it.
What about dilation? The Comprehensive Eye code exam often includes — as indicated — biomicroscopy, exam with cycloplegia or mydriasis and tonometry. If dilation is not performed, documentation must clearly state why. Dilation is not a requirement for E/M codes.
Fact Sheet for the Comprehensive Eye Visit Codes: 92004 and 92014
When Not to Bill an Eye Visit Code
There are nine specific situations that you need to be aware of when you should bill an E/M code in place of an eye visit code. Billing for eye visit codes during these situations could lead to a denial and/or patient responsibility.
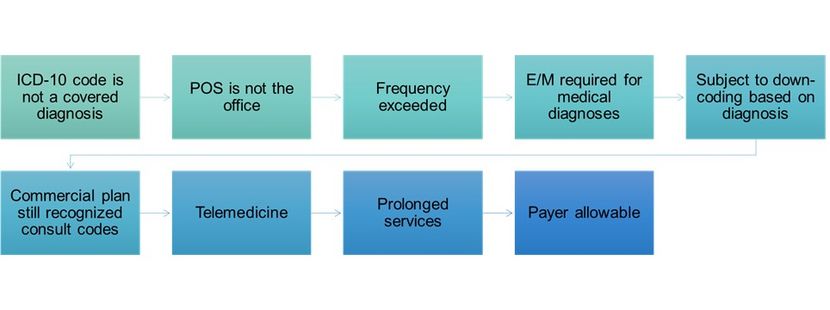
Systemic diseases such as Lupus, multiple sclerosis, and rheumatoid arthritis are all covered with E/M codes but not always covered with Eye visit codes. Some payers have frequency edits, or limits on how often you can bill eye visit codes in a year. Payers do not have frequency edits for E/M codes. Eye visit code use may be restricted by some commercial payers to routine/annual exam or vision plans. These same payers may also only permit use of E/M codes for medical diagnoses. Payer allowable is considering the amount payers reimburse for these codes and is discussed in detail below.
For additional information about each of these scenarios, review the Nine Scenarios When You Should Not Use an Eye Visit Code - American Academy of Ophthalmology (aao.org).
New vs. Established
This is an important code selection and reimbursement consideration for both E/M and eye visit codes. Review the rules at Is the Patient New or Established? Test Your Knowledge.
Code Selection
Now that you have reviewed your documentation, confirmed the appropriate level of E/M and/or eye visit code, and have taken into consideration the nine scenarios when not to use an eye visit code, you may find that either an E/M or an eye visit could could work. When both E/M and eye visit codes can be billed, consider billing the code with the highest allowable for that payer. To help determine this, create a simple spreadsheet that lists the allowables for office-based E/M and eye visit codes, for at least five of your top payers.
|
E/M, New Patient
|
Commercial #1
|
Commercial #2
|
Medicare
|
|
99202
|
$145.60
|
$141.44
|
$80.91
|
|
99203
|
$211.40
|
$205.36
|
$124.39
|
|
99204
|
$324.80
|
$315.52
|
$185.26
|
|
99205
|
$404.60
|
$393.04
|
$244.99
|
|
Eye Visit, New Patient
|
|
92002
|
$162.40
|
$138.88
|
$95.65
|
|
92004
|
$295.40
|
$199.77
|
$165.97
|
|
E/M, Established Patient
|
Commercial #1
|
Commercial #2
|
Medicare
|
|
99212
|
$85.40
|
$82.96
|
$62.76
|
|
99213
|
$142.80
|
$138.72
|
$100.57
|
|
99214
|
$210.70
|
$204.68
|
$141.78
|
|
99215
|
$282.10
|
$274.04
|
$200.00
|
|
Eye Visit, Established Patient
|
|
92012
|
$170.10
|
$128.34
|
$95.65
|
|
92014
|
$246.40
|
$198.22
|
$140.26
|
Hypothetical table listing the allowable payments for both E/M and Eye code visits for two commercial plans and Medicare. A table like this can help you understand which code to use when evaluating patients in the office.
When using E/M codes, all payers let you bill these codes as often as medically necessary. In addition, payers allow unrestricted diagnosis coverage. Medicare Part B doesn’t limit frequency for eye visit codes either; this includes comprehensive exams. Commercial payers vary, thus it is important \ to know the top payers’ guidelines and the 9 scenarios above.
Here are three example scenarios where you can test your understandiing of the information above.
Scenario 1
New patient cataract evaluation with Medicare. Documentation supports a new patient level 4 E/M code, 99204. The documentation also supports a comprehensive Eye visit code 92004. The Medicare allowable for 99204 is $185.26. The allowable for 92004 is $165.97. What code would you choose?
Answer: Choose 99204, as it has almost a $20.00 higher allowable than 92004.
Scenario 2
Established patient with commercial insurance #1 comes in for pain in both eyes. The patient had a routine examination previously with you earlier this year. Documentation supports an established level 3 E/M code, 99213 with an allowable of $142.80. The documentation also supports an established intermediate Eye visit code, 92012 with an allowable of $170.10. Which code would you choose?
Answer: 99213. Why? The commercial insurance has a frequency edit of only allowing one eye code per year for the routine eye examination. If you were to bill the 92012 based on the higher allowable amount when the payer had a frequency limitation the claim could be denied and the patient could be responsible for payment.
Scenario 3
Dry AMD Patient with commercial insurance #2 who was last seen in your practice two years ago by one of your colleagues but is new to you. Both eyes are stable, you recommend AREDS and monitor with amsler grid. Documentation supports either a level 3 E/M code and a comprehensive eye visit code. Note that the AREDS vitamins (OTC medication) do not count toward prescription drug management for the risk category. How should you code?
Answer: 99213. The patient is considered an established patient. This commercial insurance requires E/M codes when a medical diagnosis is the primary diagnosis and only accepts eye visit codes for routine or annual exams.
This process can seem daunting at first, but just like everything else you have learned in your training, the more you do something the easier it becomes. It would be easier to bill only eye visit or only E/M codes all the time, but this is not appropriate. Learning the differences and rules will be worth the
About the author: Matthew Baugh, MHA, COT, OCS, OCSR, is an Academy manager of coding and reimbursement.