Download PDF
Although proper centration of intraocular lenses (IOLs) has long been known to affect pseudophakic visual acuity, the complex optics of today’s high-technology IOLs and other refractive implants have elevated centration to new prominence, according to ophthalmologists at the leading edge of this aspect of cataract surgery.
Decentrations that would be optically insignificant for conventional monofocal IOLs can hamper the visual performance of multifocal IOLs and other implanted devices such as the Kamra corneal inlay (AcuFocus), said George O. Waring IV, MD, the international surgical monitor for AcuFocus. Dr. Waring is also assistant professor of ophthalmology and director of refractive surgery at the Medical University of South Carolina Storm Eye Institute, in Charleston, and medical director of the Magill Vision Center in Mount Pleasant, S.C.
“We’ve learned a lot from refractive surgery technologies, particularly those aimed at correcting presbyopia, about how small deviations from the line of sight can have a large impact on acuity,” he said. “Cataract surgeons should think about this with IOL patients, particularly those with advanced IOLs. Even with current microscopes and phacoemulsification technology, surgeons should consider the impact of centration with multifocal IOLs,” Dr. Waring added.
Key factors to address in obtaining optimal results include the optics of the eye’s different axes, the characteristics of the specific implants, and their interaction with ocular anatomy.
Complexities of Centration
Brazilian refractive surgeon Marcony R. Santhiago, MD, agrees that today’s hallmarks of centration are more complex than ever before. “It is not enough to center the IOL in the capsular bag,” said Dr. Santhiago, who is an adjunct professor of ophthalmology at Federal University of Rio de Janeiro. He explained that the optical differences between a corneal inlay, a diffractive multifocal IOL, and a toric multifocal IOL mean that the centering position for each of them is a little different. In particular, multifocal IOLs must be perfectly centered for an optimal result, said Dr. Santhiago. “In fact, asymmetric contractions of the capsular bag or residual OVDs left behind after surgery are often a reason why the target was not achieved with multifocal IOLs.”
Refractive and cataract surgeon Jay S. Pepose, MD, PhD, who is professor of clinical ophthalmology and visual sciences at Washington University School of Medicine, St. Louis, said that several issues regarding optimal IOL centration remain unsettled. “We are just at the very beginning of understanding the changes in vector forces and biomechanics induced by new surgical tools and techniques and their potential influence on IOL decentration and tilt,” Dr. Pepose said. “We know that the eye is an optically antisymmetric system. Even in the phakic eye, the crystalline lens is not perfectly centered or free of tilt,” he added. “A goal of IOL surgery is to best align the IOL along the visual axis of the eye, but one challenge is to determine exactly where that is at the time of surgery.
“Another important question is whether the IOL will remain in the same location when the capsule constricts approximately 14 percent in diameter over the first three months postoperatively,” Dr. Pepose said. “We know from previous toric IOL studies that a certain percentage of IOLs may rotate significantly during postoperative healing, and so where you place the lens is not necessarily where it is going to stay in every case.”
Dr. Pepose believes that certain parameters and factors will need to be determined for specific IOLs in future studies; these include optimal capsulorrhexis size, extent of IOL overlap, and centration of the continuous curvilinear capsulorrhexis with respect to the center of the lens or the pupil.
Drs. Santhiago and Waring agree that objective data on positioning adjustments are lacking. But they believe that the available clinical information does support tailoring the location of the refractive implant device to the anatomy of the patient. They identified three general steps for ophthalmic surgeons to take in order to accomplish this goal.
|
Axes and Angles
|
 |
|
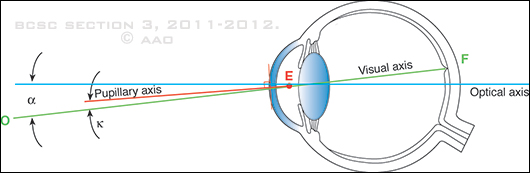
The pupillary axis (red line) is represented by the line perpendicular to the corneal surface that passes through the midpoint of the entrance pupil (E). The visual axis (green line) connects the fixation point (O) and the fovea (F). The angle between the pupillary axis and the visual axis is known as angle kappa (Κ), and the angle between the optical axis and the visual axis is known as angle alpha (α).
|
1. Optics: Go Back to Basics
“You have to go back to basic optical principles to understand centration problems,” said Dr. Santhiago. “The details can get very subtle, but the bottom line is that the optical properties of the eye are not like a regular optical system. The optics of the human eye are not centered around the optical axis.” (See Fig. 1.)
Optical axis. As ophthalmologists know well, when a penlight is aimed through the geometric center of the cornea at the retina’s geometric center, the beam will land on the posterior pole halfway between the optic nerve and the foveola. The light rays travel along an axis defined by the geometric centers of cornea, pupil, and retina—the optical axis. The corneal reflex from the light on this axial path is Purkinje image I. If the eye were a camera lens, this optical axis would be the path to the eye’s crispest images, said Dr. Santhiago, but of course the eye is not a camera lens.
Visual axis. The visual axis traces a path that extends from the fixation point through the nodal points (near the posterior surface of the lens) and then to the foveola. But because the foveola is supratemporal on the retina, the visual axis is angled 5.2 degrees nasally and slightly inferior to the optical axis (the angle alpha).
The visual axis does not necessarily pass through the pupil’s geometric center. This explains why the corneal reflex from light rays on the visual axis occurs about 0.3 mm nasal and 0.1 mm inferior to the reflex from the pupillary axis, Dr. Santhiago said.
“It should also be emphasized that the corneal vertex provides the best approximation of the visual axis, defined as the line joining the fixation point and the fovea, passing through the nodal points,” he said. “That is why, when the patient has a large angle kappa, a corneal topography–guided LASIK treatment centered on the corneal vertex, and not on the pupil’s geometric center or the line of sight, would provide better results than wavefront-guided treatment centered on the entrance pupil,” Dr. Santhiago added. “The patient is actually looking along the visual axis and not the line of sight, and that difference in centration treatment might be significant when the angle is large.”
Dr. Waring agreed and noted that there is increasing evidence that the quality of postoperative vision will be better if a refractive implant (or laser ablation) is centered on or near the visual axis, not on the entrance pupil.1-5
Pupillary axis. This axial pathway goes through the center of the entrance pupil and is perpendicular to the corneal point that it transects. This point is about halfway between the position where the optical and visual axes pass through the cornea, putting it approximately 0.3 mm away from the other axes on the corneal surface. The angular difference between the pupillary axis and the visual axis is the angle kappa.
“Most technologies previously were based on centration over the center of the entrance pupil, with that point determined at the beginning of the case. However, we’ve learned from refractive surgery, multifocal IOLs, and corneal inlays that this might not be the best place,” Dr. Waring said.
Photoreceptor orientation. Positioned orthogonally on the retina, photoreceptors capture photons most efficiently when light rays are perpendicular to the fovea, said Dr. Santhiago. Because of this biological limitation, Dr. Waring added, refractive implants that reduce or fractionate incoming light should be placed, relative to the pupil, at the best possible location to maximize the amount of light energy available to the photoreceptors.
2. Match the Axis and the Optics
The center of the undilated pupil has long been favored as the axial center for IOLs, even though the pupillary axis is angled temporally away from the visual axis. But awareness of the importance of deviating from this norm in certain eyes is increasing, largely because of lessons learned from the current generation of multifocal IOLs, noted Drs. Santhiago and Waring.
Spherical and aspheric IOLs. Spherical IOLs are the most resistant to the negative effects of improper centration, followed by aspheric lenses. Consequently, moving their axis of centration off the pupil center does not have as much impact on the optics of these lenses as it would for multifocal IOLs, said Dr. Santhiago. Nonetheless, some experts now advise that aspheric IOLs will work best if moved to a centration axis that is between 0.3 mm and 0.6 mm supranasal from the pupillary axis.
Multifocal IOLs. Although the location of perfect centration for multifocal IOLs requires validation in prospective studies, Drs. Santhiago and Waring offer suggestions from their experience.
Dr. Santhiago believes that multifocal lenses should be centered as closely as possible on the entrance pupil because they need balanced light input to create two focal points via constructive interference of the diffracted light. “If the rays that pass through the rings are not perfectly balanced on both sides of the lens, then you lose image quality at the focal points and you get light scatter,” he said.
But, like conventional IOLs, these lenses will self-center in the capsular bag after implantation. This moves them off the best axis for multifocal acuity and has been associated with patients complaining of “waxy vision.” So Dr. Waring suggests avoiding this problem when implanting multifocal IOLs, by using the coaxial light source of the surgical microscope to align both corneal and lenticular Purkinje images (with patient-assisted fixation).
According to a recent study,6 if a previously implanted IOL is off center, temporal iridotomy might improve the patient’s vision. In this study, the mean corrected distance visual acuity improved from 20/35 to 20/25. In addition to sending more photons to the photoreceptors, iridotomy moves the eye’s effective center closer to the IOL’s center, Dr. Santhiago pointed out.
Toric IOLs. These lenses obviously require accurate rotational orientation to correct corneal astigmatism. The best axis for centration is supranasal, between the pupillary axis and the visual axis (slightly more nasal than for diffractive multifocal IOLs), said Dr. Santhiago. Consequently, the optimal axis is between 0.3 mm and 0.6 mm nasal, and slightly superior, from the pupil center, he said.
Kamra corneal inlays. This annular device for presbyopia has an outer diameter of 3.8 mm and a central aperture of 1.6 mm. Implanted about 200 ?m deep, it lessens presbyopia symptoms by increasing depth of focus. FDA approval is expected this year.
Finding the correct location for centering the Kamra corneal inlay was crucial to demonstrating its effectiveness during premarket studies, said Dr. Waring. “We have had to go a step further to tease out anatomic variations that can result in decentrations that can be visually significant,” he said. Studies have determined that it’s not as simple as putting it over the center of the entrance pupil. “The best location appears to be on the eye’s achromatic visual axis, between the first Purkinje image and the pupillary center, determined in a coaxially fixated manner,” Dr. Waring explained.
Dr. Santhiago agreed that a satisfactory result with a small-aperture corneal inlay depends on accurate centration. “There are still some surgeons not achieving their targets because of centering on the pupillary center. It is crucial to make sure the center of the aperture is between the first Purkinje reflex and the pupillary center,” he said.
Improper centration of an inlay can be remedied, Dr. Santiago added. “It is important to remember that recentration of the inlay is easily possible, and this will significantly improve visual acuity if proper centration was not obtained from the first surgery.”
A special case: hyperopic eyes. In hyperopes, the ideal centration axis for devices that are especially sensitive to position (such as multifocal IOLs) is slightly inferonasal from the optimal location in other eyes.
“We know that the macula is supratemporal, but this becomes exaggerated in a short-axial hyperopic eye,” Dr. Waring explained. “When you ray trace a column of light, it will swing out the corresponding refractive reflective landmarks [Purkinje images] in the nasal direction, which accounts for the angle lambda observed in these eyes,” he said. “So for hyperopic patients, you would want to shift the axis on which you center the IOL [or Kamra inlay] slightly inferonasally from the ‘normal’ location. Your centration point would come closer to that first Purkinje reflex, or somewhere in between it and the pupil center.”
3. Avoid Fixation Error
Sometimes axial location errors occur because the surgeon is locating the pupillary center by using Purkinje reflections from an off-center light source, noted Dr. Santhiago. “During surgery, you cannot have the patient look up, even under topical anesthetic, at an illumination light and use that light reflex, because in most cases the light in the surgical microscope is not directly over the center of the eye,” he said. “When the patient looks at a light source on the edge of the microscope, he has to look downward instead of along the optical axis.”
In response to this problem, some ophthalmic equipment companies now sell central fixation lights that can be attached to the microscope barrel to ensure that the microscope’s fixation light is in the middle of the barrel, aligned with the optical axis. Without this adaptation, centering on the light reflex is not recommended.
If the fixation light is in the right place, Dr. Waring said, the concentric rings on a multifocal IOL will facilitate centration of the lens on the pupil. The first and third Purkinje reflections should be aligned within the smallest ring on the IOL. Dr. Waring noted that the rings also can give the surgeon a visual gauge when the IOL is being shifted away from the pupil’s center.
___________________________
1 Alió JL et al. J Cataract Refract Surg. 2011;37(2):241-250.
2 Reinstein DZ et al. J Refract Surg. 2012;28(2):139-143.
3 Arbelaez MC et al. Invest Ophthalmol Vis Sci. 2008;49(12):5287-5294.
4 Arba Mosquera S, Ewering T. J Refract Surg. 2012;28(8):567-573.
5 Vinciguerra P et al. New asymmetric centration strategy for excimer custom treatment: combining pupil and corneal vertex information. Presented at the 30th Congress of the European Society of Cataract & Refractive Surgeons, Sept. 2012, Milan, Italy.
6 Solomon R et al. J Refract Surg. 2012;28(4):281-283.
___________________________
Dr. Pepose is a consultant for Abbott Medical Optics, Bausch + Lomb, Elenza, and TearLab; has received grant support from AcuFocus and Bausch + Lomb; and is an equity owner of AcuFocus, Calhoun Vision, Elenza, and TearLab. Dr. Santhiago reports no related financial interests. Dr. Waring is a consultant for Ista, RevitalVision, and Topcon, and has equity ownership in and is world surgical monitor for AcuFocus.