Download PDF
The increasing availability of premium IOLs in the U.S. market is providing more choice and greater opportunity for patients seeking both better vision and the promise of spectacle independence. And today’s lenses can address a significant portion of refractive challenges with at least some success, said Cristos Ifantides, MD, MBA, who is in private practice in Cape Coral, Florida. At the same time, new IOL technologies are leading to more complex and intense preoperative decision-making by ophthalmologists and their patients in order to select the most appropriate path forward for patients’ individual needs, he said.
So how are surgeons navigating this diverse array of therapeutic options, especially in patients who hope to be free of glasses? Four leading refractive surgeons—Sumit Garg, MD, Preeya K. Gupta, MD, Rahul S. Tonk, MD, MBA, and Dr. Ifantides—review four hypothetical and uniquely challenging cases, which were supplied by Kendall E. Donaldson, MD, Cataract Section Editor of the EyeNet editorial board. Their differing recommendations illustrate the range of valid approaches, as well as the importance of discussing the pros and cons with patients to help them form realistic expectations regarding visual outcomes and possible complications.
CASE 1
PATIENT: A 51-year-old man is interested in freedom from glasses and contacts. He is currently wearing glasses only for reading but is very concerned about the possibility of halos.
PROBLEM: What to recommend: cornea refractive surgery, lens-based refractive surgery, medical management, or stick with glasses and contacts?
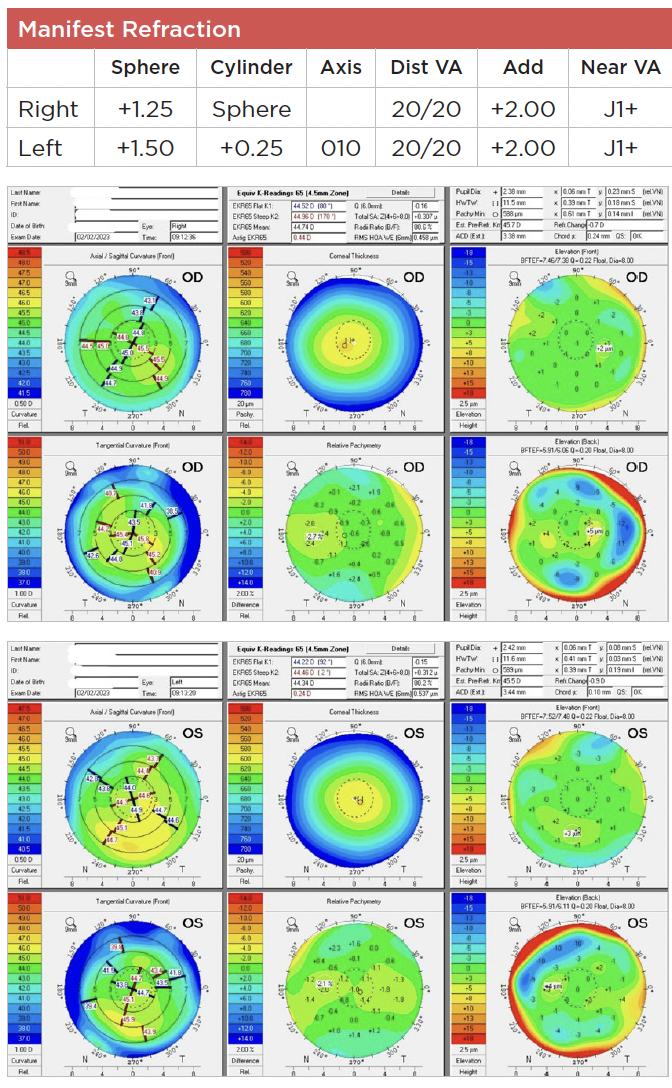
PRESENTS WITH:
___________________________
Dr. Ifantides: Although I think this patient would do well with surgery, I’d start with medical management since he is concerned with halos. There is potential to make him less happy if he undergoes surgery without first exploring the nonsurgical route. After doing a thorough dilated fundus exam, I’d offer Vuity (low-dose pilocarpine) as a first-line therapy, which would improve his near vision and likely also his distance vision as he continues to lose his ability to accommodate.
If this solution isn’t ideal for the patient, I’d then move on to surgery. Although he does qualify for hyperopic LASIK or PRK, these patients can regress, and there are alternative lens-based solutions that are excellent. I’d advocate for a monovision contact lens trial to see if he tolerates this and, if so, offer refractive lens exchange (RLE) using monovision. If he doesn’t tolerate this, I’d recommend an RLE with a monofocal in the dominant eye and the AcuFocus IC-8 Apthera lens in the nondominant eye. This would assuage his serious concerns about halos, which could arise from a diffractive multifocal IOL.
Dr. Garg: I really want to know how concerned he is about halos and take the time to figure out his motivation for surgery. Is it really just to get rid of glasses? Does the patient understand that many procedures which provide spectacle independence may then necessitate wearing glasses for other tasks later on?
Hyperopic LASIK is one option, but the effect of this procedure is often short lived relative to patient expectations—especially given the lenticular changes that typically occur in this patient’s age range. Most patients don’t understand the difference between hyperopic and myopic LASIK or the longevity of the treatment. I would stick with glasses and contacts here and kick the can down the road, given his age and the fact that he may need cataract surgery relatively soon.
Another consideration would be a miotic drop (after a thorough ocular exam, including a dilated fundus exam) as a bridge to eventual surgery.
Dr. Gupta: First, it’s important to elicit any history of contact lens wear that might include a bad experience with multifocals. Given that the patient is wearing glasses for reading, I suspect he wears distance-only contact lenses, in which case he may not have any nighttime halo currently.
When patients state that they do not want halo, I tend to favor extended depth of focus (EDOF) lenses. You can aim for plano in the dominant eye and have slight near target of –0.3 D to boost near. If the patient has previously done monovision with contacts, I often aim –0.5 to –0.75 D to boost their near vision, as they’re already tolerant of a difference in their distance vision.
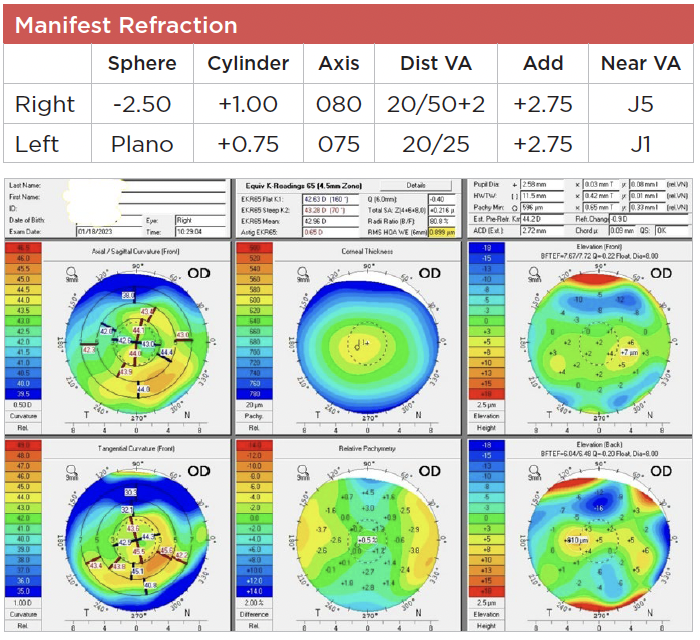
Looking at the tomography images, I see that a detailed slit-lamp exam is also necessary to make sure there are no ocular surface issues such as dry eye disease (DED) or anterior basement membrane dystrophy that might explain the mild irregular astigmatism seen on his map.
Dr. Tonk: I’d want additional data points to help advise the patient: a cycloplegic refraction, a wavefront analysis of the crystalline lens, and a monovision contact lens trial.
If the patient has 1) little to no latent hyperopia, 2) a clear crystalline lens, 3) some residual accommodation, and 4) tolerates monovision well, I would favor laser vision correction, targeting plano in the dominant eye and –0.50 to –1.5 D in the nondominant eye, depending on his willingness to wear readers for some activities. It’s important to alert the patient that he may need a lens-based procedure in five to 20 years.
If the patient has significant latent hyperopia or lens opacification, I’d consider either no surgery or RLE with some caveats. RLE performed with a monovision arrangement or with a pinhole IOL (IC-8 Apthera) in the nondominant eye would maintain excellent optical quality but might not provide a full range of vision without glasses. RLE with an EDOF lens (Alcon Vivity or Tecnis Symfony OptiBlue) may provide a better range but at the expense of some photic phenomena.
CASE 2
PATIENT: A 55-year-old software engineer with a healthy eye exam wants freedom from glasses and contacts. He does not like monovision and does not want to wear reading glasses. He currently is wearing progressive glasses full-time.
PROBLEM: Is this patient best suited for cornea-based or lens-based refractive surgery?
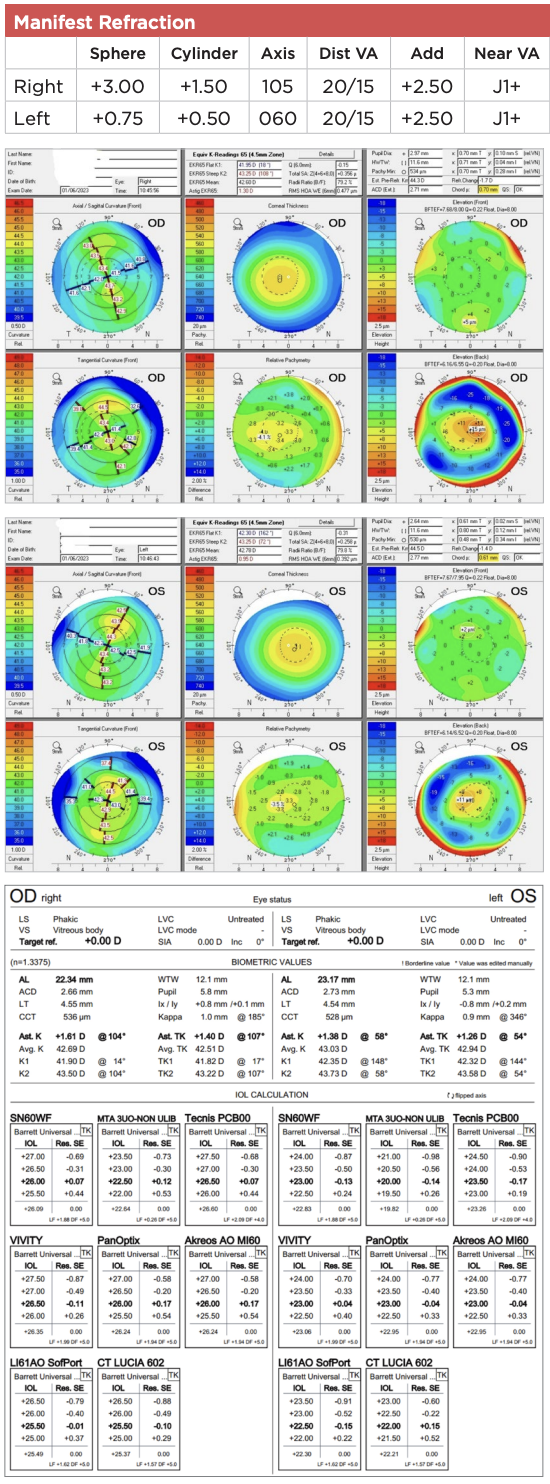
PRESENTS WITH:
___________________________
Dr. Tonk: This patient desires spectacle independence at distance, intermediate, and near. The option most likely to achieve this would be RLE with a trifocal IOL (Alcon PanOptix) or combination multifocal/EDOF IOL (Tecnis Synergy).
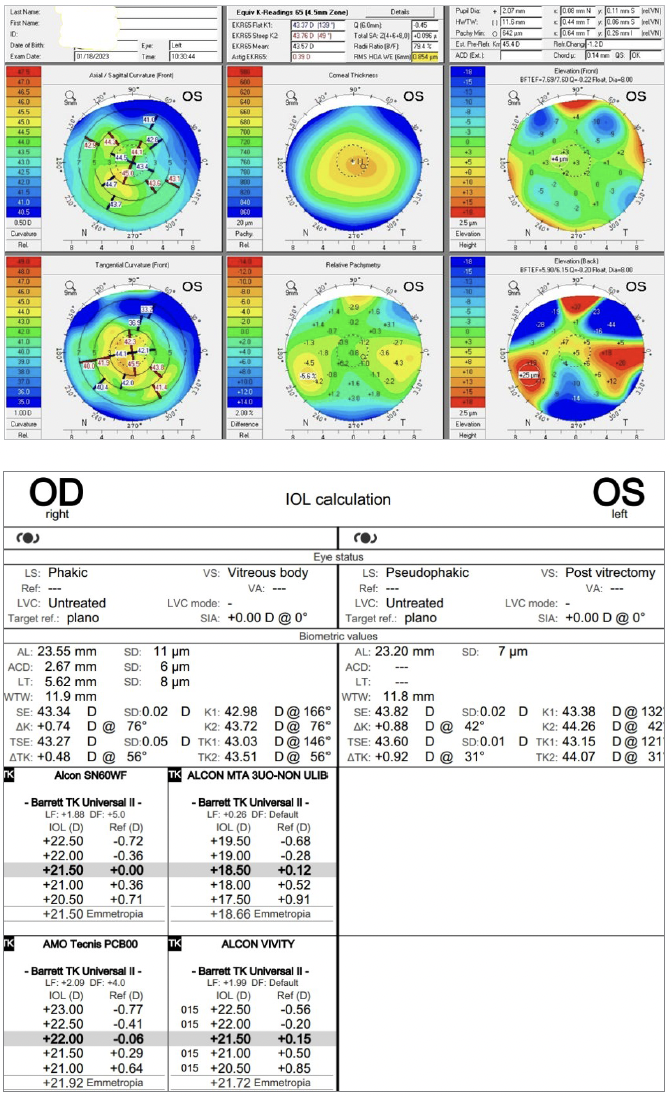
However, the patient would need to be counseled carefully about the possibility of photic phenomena with these IOLs, particularly because his posterior cornea is somewhat abnormal and his chord mu is above the 0.6-mm threshold where such phenomena may be more common.
If the patient is concerned about visual quality and doesn’t mind wearing readers for some activities, I would prefer RLE with an EDOF lens implanted bilaterally or mixed implantation of a monofocal IOL targeted to plano in the dominant eye and a pinhole IOL (IC-8 Apthera) in the nondominant eye.
Dr. Gupta: He has anisometropia, and so I would look at the patient’s goals, keeping his occupation in mind. He’s an engineer who does not want to wear glasses for near work. My experience is that engineers spend time dissecting the world around them, and our current diffractive presbyopia-correcting IOLs may not be well tolerated.
Based on his corneal imaging, there’s also significant posterior elevation, which is suspicious for an ectatic condition. He is over age 50 so progression is less likely than if he were younger, but his corneal shape may work against diffractive optics. I would therefore consider an EDOF lens but also would offer him a near-target in both eyes so he could have good near vision and only need glasses for distance.
Dr. Ifantides: Despite this patient’s almost 3 D of anisometropia, he does not do well with monovision and is currently in full-time progressive lenses. I would therefore avoid LASIK/PRK in this hyperope for the reasons previously mentioned in Case 1 regarding regression.
His spherical aberration (SA) and higher order aberration (HOA) are borderline for using a diffractive IOL. I would avoid using the multifocal that I rely on most often, the PanOptix. You could consider an EDOF toric such as the Vivity, but you run the risk of the HOAs causing issues with image ghosting and streaking of light.
Similar to Case 1, I would consider a monofocal in the dominant eye (RxSight Light Adjustable Lens [LAL], Bausch + Lomb enVista, or Tecnis Eyhance) and the IC-8 Apthera in the nondominant eye, which would pair nicely with this level of corneal aberration.
Dr. Garg: With respect to the posterior changes, they are unlikely to be progressive at his age, but you always want to make sure that these patients aren’t having any kind of progression on the corneal side of things. I’d ask him about any history of eye rubbing because that’s one risk factor for progression of ectasia due to keratoconus or after LASIK at any age.
I’d start by following him for a couple of months to make sure his cornea is indeed stable. If I were to do anything at that point, it would be a lens-based surgery—probably avoiding a multifocal lens and choosing a monofocal “plus” like the Eyhance. To give him the best range of vision at this stage, I’d advise a little offsetting in his nondominant eye. I typically try to get distance in the dominant eye and aim the nondominant eye anywhere between –0.3 to –0.6 D, staying within that range for a little depth of focus. By doing so, the patient is only slightly blurred in the nondominant eye, and they’re able to achieve good range of vision and certainly binocular summation. Alternatively, the Tecnis Symfony OptiBlue would be a reasonable option.
You could always try a contact lens trial before surgery to see how well the patient tolerates a mild amount of monovision.
CASE 3
PATIENT: A 57-year-old man with a history of LASIK in both eyes 20 years ago followed a few months later by bilateral enhancement. He was a +7.0 D hyperope before LASIK and was happy with his vision after the second procedure until approximately two years ago when he noticed a gradual progressive decline in vision in both eyes. He has been wearing scleral lenses for the past year; however, he stopped wearing them two months ago, as they were no longer improving his vision.
PROBLEM: How to manage this patient’s irregular astigmatism now that he is potentially facing cataract surgery? How to choose the best IOL for this patient, and what refractive target to choose with a standard monofocal IOL versus some of the newer IOL options (which may be more dependent upon availability)?
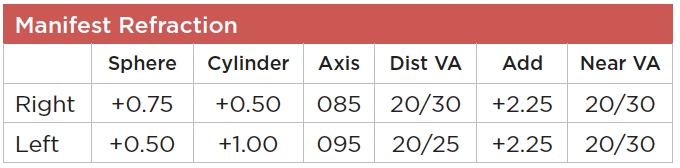
PRESENTS WITH:
___________________________
Dr. Ifantides: The patient now has high SA and HOAs as a result of his hyperopic LASIK and enhancements. Additionally, he is at high risk for refractive surprise following cataract surgery. He also has irregular astigmatism that will certainly impact his visual potential following lens-based surgery.
In these types of patients, I advocate heavily for the LAL as a way of handling stable irregular astigmatism and a high likelihood of refractive surprise. Monofocal IOLs paired with or without the IC-8 Apthera would also be a good option since it seems like this patient does not have issues with wearing scleral lenses in the event of refractive surprise.
Dr. Tonk: My IOLs of choice for this patient would be either the IC-8 Apthera or LAL.
The argument for the IC-8 Apthera is that its pinhole optics can compensate for the patient’s corneal aberrations and irregular astigmatism, improving both the patient’s uncorrected and best spectacle corrected acuity. However, this patient may have residual refractive error (this IOL only treats up to 1.5 D of astigmatism) and may note dimming of vision if the IC-8 Apthera is implanted bilaterally (for off-label use).
The argument for the LAL is that the likelihood of achieving emmetropia (or possibly a monovision target) in this complex, post-refractive cornea is much improved. Recall that this patient was generally happy with his vision for 18 years prior to the onset of cataract.
Dr. Garg: My first thought is, wow, 7 D hyperopic LASIK! That’s something we typically don’t recommend these days. I’m also concerned with his high irregular astigmatism, which leads me to believe that he will have poor quality of vision. In addition, he has high negative SA. Because of these challenges, I’d go with using a more traditional spherical lens like the Alcon SA60AT or Johnson & Johnson Vision’s Sensar AR40.
To achieve the best quality of vision possible, this patient probably will be dependent on contact lenses, given his corneal irregularity. And if that’s the case, I generally stick to more standard lenses and try not to complicate matters. Because he has ectasia (see the posterior bowing on the Pentacam), you also want to be careful of your IOL targeting because sometimes you can overestimate the spherical power of the eye and underpower the lens. So here I would fudge on the side of myopia with the hope of keeping him a little myopic—or as close to emmetropia as possible.
Depending on how well his eyes dilated, the IC-8 Apthera could be a good option in his nondominant eye. In the United States, the device is approved for use in only one eye. However, you could go off-label and use it bilaterally, as long as you have a proper discussion about the risks versus the benefits.
Dr. Gupta: This patient has had the extremes of refractive surgery, and his steep corneal curvature power shows it. His cornea is near 50 D in terms of steepness, and his baseline prior to developing a cataract was to wear scleral lenses.
I would give him two options: 1) a standard monofocal lens targeting slight myopia given the steepness of the cornea with a plan to use scleral lenses postop or 2) the IC-8 Apthera, especially if our patient desires to be less dependent on contacts.
The Apthera’s pinhole optics may be advantageous to a patient like this who has irregular corneas and what appears to be DED due to the oversteepening of the cornea, as well as irregular astigmatism following refractive surgery. However, because patients do note some dimming of their vision with the IC-8 Apthera, it would not be suited for bilateral implantation. I would place it in the more irregular eye and plan for a monofocal IOL in the other eye, perhaps with a near target if tolerated.
CASE 4
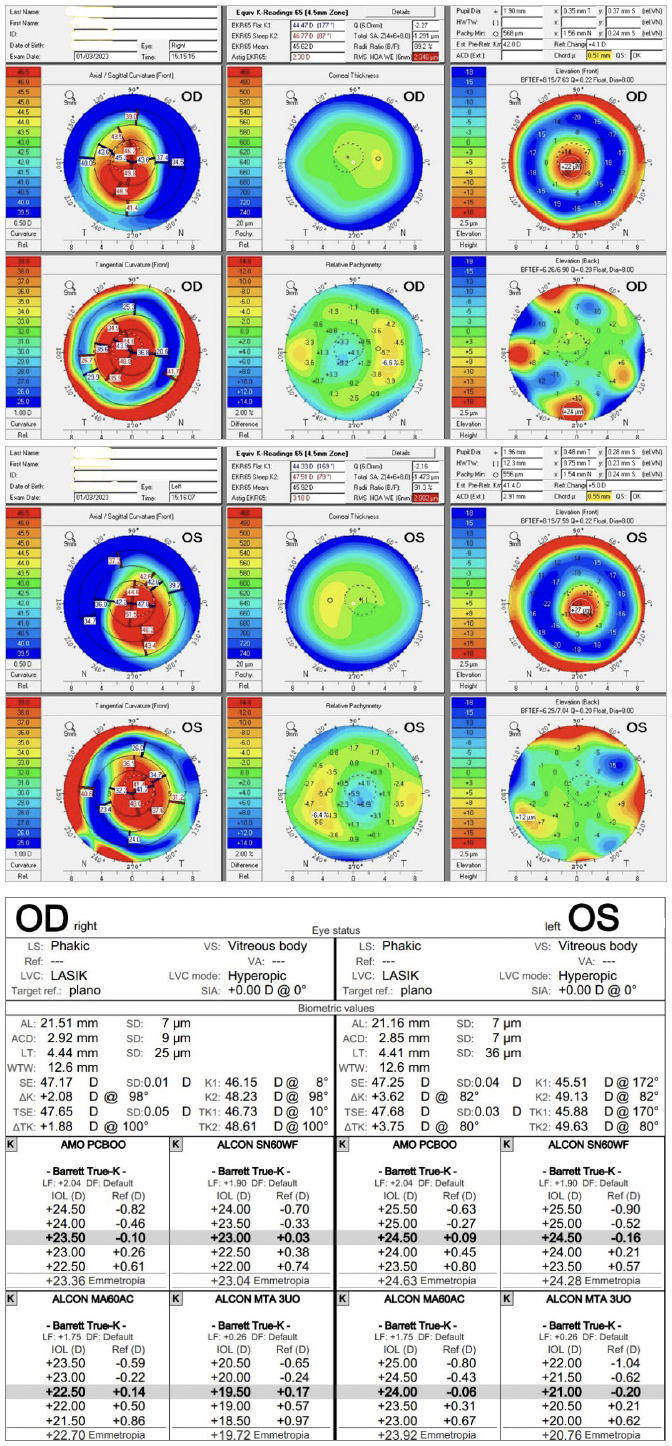
PATIENT: A 74-year-old woman with a history of pseudoexfoliation syndrome had cataract surgery in the left eye one year ago. Surgery in the left eye was followed by IOL dislocation (see photo, page 49) on post-op day 1, and the patient was referred to a retina specialist for scleral fixation. She now presents for cataract surgery in the right eye. On exam, pupillary dilation in the right eye is limited to 4 mm, but no signs of phacodonesis are present.
PROBLEM: How to address this with the patient before surgery? How to best prepare for this surgery? Which tools to have available in the OR just in case? Where to place the IOL, which type of IOL to place, and how to choose the refractive target?
PRESENTS WITH:
 |
|
Dislocated IOL in the patient’s eye.
|
___________________________
Dr. Tonk: I’d begin by expanding the pupil with iris hooks, which I find gives the greatest flexibility in complex cases. I would then utilize femtosecond laser or a phaco-chop technique for nuclear disassembly to minimize intraoperative zonule trauma. I would also meticulously clean the capsular bag to prevent phimosis and stabilize the bag with a capsular tension ring (CTR), suturing it to the sclera if needed and inserting the IOL into the capsular bag.
My preference would be a monofocal IOL targeted to plano or –0.5 D. Notably, the patient would lose the myopia in her right eye (which likely resulted from nuclear sclerosis), and she should be counseled accordingly.
Although a presbyopia-correcting IOL may be utilized in certain cases, I am concerned about intra- and postoperative centration and whether unilateral implantation of that IOL would achieve the desired goal of spectacle freedom.
A monovision near target may also be used, but I’m also concerned the impaired fellow eye may not carry the full weight of providing distance vision
Dr. Ifantides: This is a difficult case with multiple acceptable options. I have two similar pseudoexfoliation patients whom I am currently managing. In one case, I removed the dislocated IOL and placed a Gore-Tex–sutured enVista. For the other patient, I removed the dislocated IOL and placed a Zeiss CT Lucia 602 using a modified Yamane technique. I chose different techniques for different reasons, but both patients had a pars plana anterior vitrectomy at the time of the secondary IOL placement.
For this case, it’s difficult to know what happened during the first surgery and if anything could have been done differently. I would proactively place a CTR prior to IOL placement, even if the bag appeared stable. Although the literature suggests that a prophylactic CTR might not change outcomes in pseudoexfoliation,1 more recent studies have shown improved tilt and centration of IOLs when a CTR is used.2
I would target the first myopic target closest to plano and opt for a monofocal aspheric IOL like the enVista. The haptics are angulated at 56 degrees to provide total coverage of 112 degrees of bag, higher than other monofocals. In addition, the power is the same from center to the edge, making decentration less of an issue.
Dr. Gupta: Pseudoexfoliation is a difficult condition, as it’s quite variable in its presentation and variable in terms of how advanced the disease is.
Given these unknowns, I’d lean toward using a femtosecond laser to allow for less manipulation of the lens and clean placement of the rhexis before the pupil constricts. I would also use iris hooks or a Malyugin ring if I feel that the pupil dilation is inadequate. Surgical techniques should include gentle manipulation and rotation of the lens to avoid damaging zonules, and lens selection should be based upon the integrity of the capsular bag and zonules.
In this case, I would plan for a monofocal lens in the bag and consider placing a CTR for additional stability. In some instances, the entire bag is faulty, and an anterior chamber lens is required.
Dr. Garg: What I would want to know first is if the patient is happy with the sort of monovision she’s been left with. Her left eye has ended up better for distance, and the spherical equivalent in her right eye is about a –2 D. If she’s happy with that, it might be good to leave her a little bit nearsighted.
Because pseudoexfoliation is often asymmetric, I tend to go into these cases planning for the worst and make sure all of my tools are available. I’d definitely plan for a CTR. In my experience, the Zeiss CT Lucia works really well in these types of patients because you have the option of performing an intrascleral haptic fixation either at the time of original surgery or later, if something happens postoperatively.
I would aim for leaving the patient a little bit myopic because I think she’d probably benefit from a range of vision in which her left eye is more distance dominant and the right eye a little myopic. However, the risk here is that if there is progressive zonular weakening, the lens can move forward, resulting in additional myopia. So, the patient would need to be made aware of that.
___________________________
1 Kocabora MS et al. Ann Ophthalmol (Skokie). 2007;39(1):37-40.
2 Miyoshi T et al. PLoS One. 2020;15(2):e0228999.
Meet the Experts
Sumit Garg, MD Professor of ophthalmology and vice chair of clinical ophthalmology at the Gavin Herbert Eye Institute, University of California, Irvine. Relevant financial disclosures: Johnson & Johnson Vision: C; Zeiss: C.
Preeya K. Gupta, MD In private practice with Triangle Eye Consultants in Raleigh, N.C. Relevant financial disclosures: Alcon: C; Bausch + Lomb: C; and Johnson & Johnson: C.
Cristos Ifantides, MD, MBA In private practice with Tyson Eye in Cape Coral, Fla., and adjunct assistant professor of ophthalmology at the University of Colorado in Aurora, Colo. Relevant financial disclosures: Ace Vision Group: C; Acufocus: C; Alcon: C; Bausch + Lomb: C; Zeiss: C.
Samuel Masket, MD In practice at Advanced Vision Care in Los Angeles and clinical professor of ophthalmology at the Stein Eye Institute, University of California, Los Angeles. Relevant financial disclosures: None.
Rahul S. Tonk, MD, MBA Assistant professor of clinical ophthalmology and associate medical director at the Bascom Palmer Eye Institute in Miami, Fla. Relevant financial disclosures: None.
Full Financial Disclosures
Sumit Garg, MD Alderya Therapeutics, Inc.: C; Allergan, Inc.: C; Avellino Labs: C; Carl Zeiss Meditec: C; Centricity Vision: C; CorneaGen: C; Dompe: C; Expert Opinion: PS,C; ForSight Robotics: C,PS; Glaukos Corporation: C; Johnson & Johnson Vision: C; Kala Pharmaceuticals, Inc.: C; LensGen Inc: C,PS; New World Medical Inc: C; Novartis Pharma AG: C; Ocutrx Technologies: PS; Oyster Point Pharma: C; Samsara Vision: C; SightSciences: C; Spyglass Pharma: C,PS; Tarsus Pharmaceuticals: C,SO;Trefoil: C; Visus Therapeutics Inc: C,PS.
Preeya K. Gupta, MD Alcon Laboratories, Inc.: C; Aldeyra Therapeutics Inc: C; Allergan, Inc.: C; Azura Ophthalmics: C,SO; Bausch + Lomb: C; Dompe: C; Expert Opinion: C,SO; HanAll BioPharma: C; Johnson and Johnson Vision: C; Kala Pharmaceuticals, Inc.: C; Lensar: C; New World Medical Inc: C; Novartis Pharma AG: C; Ocular Science: C,SO; Ocular Therapeutix: C; Orasis Pharmaceuticals Inc: C,SO; Oyster Point Pharma: C,SO; Sight Sciences, Inc.: C; Spyglass: C,SO; Sun Pharmaceutical Industries Inc: C; Surface: C,SO; Tarsus Pharmaceuticals: C,SO; Tear Lab: C; TearClear: C,SO; TissueTech, Inc.: C; Trukera Medical: C; Visant: SO; Visionology: C,SO; Zeiss Carl Ltd.: C.
Cristos Ifantides, MD, MBA AbbVie: C; Ace Vision Group: C; AcuFocus: C; Alcon Laboratories: C; Bausch and Lomb: I; BVI: C; Centricity Vision: C; Hu-Med Technologies: C,P; Johnson & Johnson: C,S; New World Medical: P,I; Spect: C; Tarsus: C; Trefoil: C; Vision 2020 USA: C; Visus Therapeutics: C; Zeiss: C,I.
Samuel Masket, MD Alcon: C; CAPSULaser: C; Haag Streit: C,P; Morcher: P; Ocular Therapeutix: C.
Rahul S. Tonk, MD, MBA Bruder: C; Glaukos: L; LayerBio: PS; Sight Sciences: C; Tarsus: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Hired to work for compensation or received a W2 from a company. |
| Employee, executive role |
EE |
Hired to work in an executive role for compensation or received a W2 from a company. |
| Owner of company |
EO |
Ownership or controlling interest in a company, other than stock. |
| Independent contractor |
I |
Contracted work, including contracted research. |
| Lecture fees/Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Patents/Royalty |
P |
Beneficiary of patents and/or royalties for intellectual property. |
| Equity/Stock/Stock options holder, private corporation |
PS |
Equity ownership, stock and/or stock options in privately owned firms, excluding mutual funds. |
| Grant support |
S |
Grant support or other financial support from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and\or pharmaceutical companies. Research funding should be disclosed by the principal or named investigator even if your institution receives the grant and manages the funds. |
| Stock options, public or private corporation |
SO |
Stock options in a public or private company. |
| Equity/Stock holder, public corporation |
US |
Equity ownership or stock in publicly traded firms, excluding mutual funds (listed on the stock exchange). |
|