This article is from July/August 2004 and may contain outdated material.
Not long ago, a woman with active rheumatoid arthritis made an appointment to see Ernest W. Kornmehl, MD. But instead of requesting a basic checkup, she was after a LASIK evaluation. “You would be surprised how many patients with autoimmune disease come to me asking me to perform a refractive surgery procedure,” said Dr. Kornmehl, medical director of Kornmehl Laser Eye Associates in Boston. “For many of these individuals, LASIK and other refractive surgical procedures are contraindicated, but this doesn’t deter them” from looking for an ophthalmologist who will give them what they want.
Indeed, a considerable number of patients with connective tissue diseases, autoimmune diseases or immunodeficiency conditions persist in pursuing LASIK, indicating that ophthalmologists still need to keep their guard up when it comes to patient selection.
Risk of Poor Outcomes
The risk associated with autoimmune disease and refractive surgery was first identified in the late 1980s when a German patient with lupus experienced corneal melt and perforation after PRK, noted Joseph Trentacoste, MD, of the Laser Vision Eye Care Center in Miami Lakes, Fla.
In 2002, both the Academy and the FDA cited autoimmune and immunodeficiency conditions as contraindications for LASIK.¹
“A person with an autoimmune disorder who undergoes LASIK is at risk for corneal thinning, corneal melts, corneal ulcers and irregular healing, as well as scleritis, episcleritis, keratitis and inflammation in the eye,” said Dr. Trentacoste. “Additionally, with the inflammatory condition, the lacrimal gland is affected, potentially leading to extremely dry corneas.”
Another issue, added Dr. Kornmehl, relates to the medication patients with collagen vascular diseases must take. “Many of these patients are on systemic steroids and immunosuppressants, which are contraindications for refractive surgery,” said Dr. Kornmehl, who’s also associate clinical professor of ophthalmology at Tufts and clinical instructor of ophthalmology at Harvard. “Also, we don’t know what will happen to these patients down the road, years after undergoing the procedure. It’s one thing to have patients who simply present with dry eyes—we can manage them extremely well. But in patients with rheumatoid arthritis, lupus and so forth, we jaust can't predict long-term outcomes."
 |
|
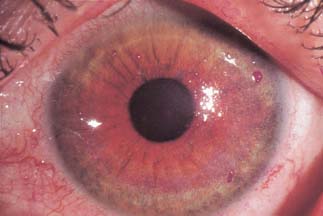
One reason why patients with autoimmune disease should steer clear of LASIK: an increased risk of corneal problems, such as the filamentary keratitis seen here.
|
When Diagnosis Is Elusive
Identifying patients with conditions that are contraindicated for LASIK can be tricky at times, Dr. Trentacoste pointed out. To address this challenge, he uses a standard list of questions that begins with pregnancy, lactation and ocular herpes and moves on to more general questions, such as whether the patient has stiff joints, which could indicate rheumatoid arthritis or a connective tissue disease, or tends to form keloids, as there is a risk of developing excess scar tissue when the flap heals.
A preoperative Schirmer test is also essential, Dr. Trentacoste said. “If I have any doubts or suspicions,” he said, “I send these patients back to their internist for a basic collagen vascular workup.”
Unfortunately, some patients with autoimmune disease can slip through the cracks. Dr. Trentacoste recalled a patient of his who, six months after he had undergone LASIK, was diagnosed with granulomatosis with polyangiitis (formerly Wegener’s granulomatosis), which often has a slow onset, with nonspecific coldlike symptoms.
“While [the patient] had absolutely no symptoms prior to surgery,” Dr. Trentacoste noted, “he experienced a difficult postoperative course, including inflammation that we treated with oral as well as topical steroids. While his vision was 20/20, I just didn’t know what was going on—until the diagnosis of granulomatosis with polyangiitis.”
When Disease Is Inactive
Are patients with inactive collagen vascular disease candidates for LASIK? Dr. Trentacoste says no. “First, there is no guarantee that the disease is actually inactive, leaving the patient open to the risk of corneal inflammation or a corneal melt developing. In addition, many of these patients are taking steroids, which place patients at risk for wound infection and delayed healing.”
When It’s HIV
Robert K. Maloney, MD, director of the Maloney Vision Institute of Los Angeles, has “no hesitation” performing refractive surgical procedures on patients with immunodeficiency conditions, such as HIV. The two key issues here, he explained, are whether the surgeon is at risk for contracting HIV if he or she performs the surgery, and whether the patient is at an increased risk of infection.
Concerning the former issue, “it is highly unlikely that HIV is transmitted by the laser. Thus, I don’t think the laser ablation poses a risk to me or my staff. As for a risk of a needle stick, that should be on the mind of every surgeon whether the patient has HIV or not. And every surgeon should be using universal precautions. Additionally, research has shown that HIV is difficult to transmit via a needle stick unless it is a hollow needle. A bloody point is not enough.”
The risk to the patient of infection is not much of an issue either, Dr. Maloney explained. “While patients with HIV who get infections are more difficult to treat, I have performed refractive surgery on a large number of HIV patients without infection,” he said. “However, I will only operate on patients who are on triple drug therapy with an undetectable viral load. In addition, I always suggest performing the procedure one eye at a time because I don’t want to be faced with treating a bilateral infection. With that said, half the time they elect to have both eyes treated, and I am certainly comfortable doing that with proper informed consent.”
Pro and Con
Dr. Maloney has his own opinions on performing refractive surgery on patients with autoimmune or immunodeficiency disorders. Recently, he and Ronald Smith, MD, compiled statistics on this topic. “We reviewed every patient whom I treated since June 1998,” Dr. Maloney said, “and out of 10,000 charts, we found 19 patients with autoimmune diseases—five with rheumatoid arthritis, six with lupus and the remainder with a smattering of other diseases. Interestingly, none of these patients developed corneal thinning or melting."
Dr. Maloney noted that the study population was small and that the review did not analyze dry eye. Additionally, these patients all had autoimmune diseases that were either inactive or well controlled by medical therapy. "My personal feeling on the topic," he said, "is that it is acceptable to do LASIK if you carefully select the patients and they are well informed about the risks."
Dr. Trentacoste said he believes the key word for ophthalmologists considering refractive surgery options for their patients with autoimmune and immunodeficiency conditions is caution. "In my opinion," he noted, "anyone who does LASIK on these patients is treading on thin ice." He added, "I think an ounce of prevention is worth several pounds of cure. Do no harm."
______________________________
1 See Preferred Practice Pattern on refractive errors at www.aao.org/ppp. The FDA statement is at www.fda.gov under "Hot Topics."
______________________________
More Reasons to Rule Out LASIK
Certain systemic drugs. For instance, isotretinoin (Accutane) is used to treat severe acne and is secreted in the tears via the lacrimal gland. This can cause irritation, including a drug-induced conjunctivitis with corneal irritation. Other drugs to screen for include sumatriptan (Imitrex) and levonorgestrel implants (Norplant).
Diabetes. “The main thing to look for is decreased corneal sensation,” said Dr. Kornmehl, “because corneal sensation is linked to wound healing. Diabetics with intact corneal sensation do very well.”
Glaucoma. Certain patients with early glaucoma who do not have nerve damage could sustain a spike in pressure from the keratome without sustaining damage. However, Dr. Kornmehl warned that caution is of the essence with these patients. Additionally, after laser vision correction, these patients can have a lower Goldmann reading from the center of the eye and thus should be told to look to the right or left for an accurate reading. “A few millimeters can make a big difference in glaucoma patients and glaucoma suspects,” he said.
Graves’ disease with proptosis. “However, someone with no ocular findings and controlled Graves’ disease may be an appropriate candidate,” Dr. Kornmehl said.
Pregnancy or lactation. These patients are more likely to have refractive instability, as hormones alter collagen remodeling.